Korean J Transplant.
2022 Sep;36(3):197-202. 10.4285/kjt.22.0020.
Prevalence and clinical significance of pancreatic cystic lesions in immunosuppressed patients following solid organ transplantation
- Affiliations
-
- 1Department of Surgery, Korea University College of Medicine, Seoul, Korea
- 2Division of HBP Surgery and Liver Transplantation, Department of Surgery, Korea University College of Medicine, Seoul, Korea
- 3Division of Transplant and Vascular Surgery, Department of Surgery, Korea University College of Medicine, Seoul, Korea
- KMID: 2533957
- DOI: http://doi.org/10.4285/kjt.22.0020
Abstract
- Background
Pancreatic cystic lesions (PCLs) are occasionally found in solid organ transplant (SOT) recipients. In such recipients, the risk of cancer is increased due to immunosuppressive therapy. This study investigated the prevalence of PCLs and de- scribed their clinical course in immunosuppressed patients following SOT.
Methods
The presence of PCLs in a retrospective cohort of 805 consecutive SOT re-cipients from 2009 to 2019 was examined. The characteristics of PCLs were compared using initial and follow-up imaging, where available. These results were compared to an age- and sex-matched immunocompetent control group monitored for at least 12 months.
Results
PCLs were present in 15 of 805 SOT patients (seven liver and eight kidney transplantations). The median diameter of the largest lesion was 20 mm (range, 0.2–60 mm) and 60% of lesions were benign. During follow-up imaging, the cyst size remained stable in 46.7%, increased in 13.3%, and decreased in 40.0% of the SOT group. Signifi-cantly more of the SOT patients showed PCL size reductions (P=0.007). Among SOT patients diagnosed with intraductal papillary mucinous neoplasms (6/15), worrisome features were noted in one patient at the time of cyst diagnosis. Differences in the development of worrisome features between the study and control groups were not statistically significant.
Conclusions
The malignant transformation of PCLs in SOT recipients is rare and most such PCLs can be managed conservatively. The presence of a PCL should therefore not affect transplant eligibility.
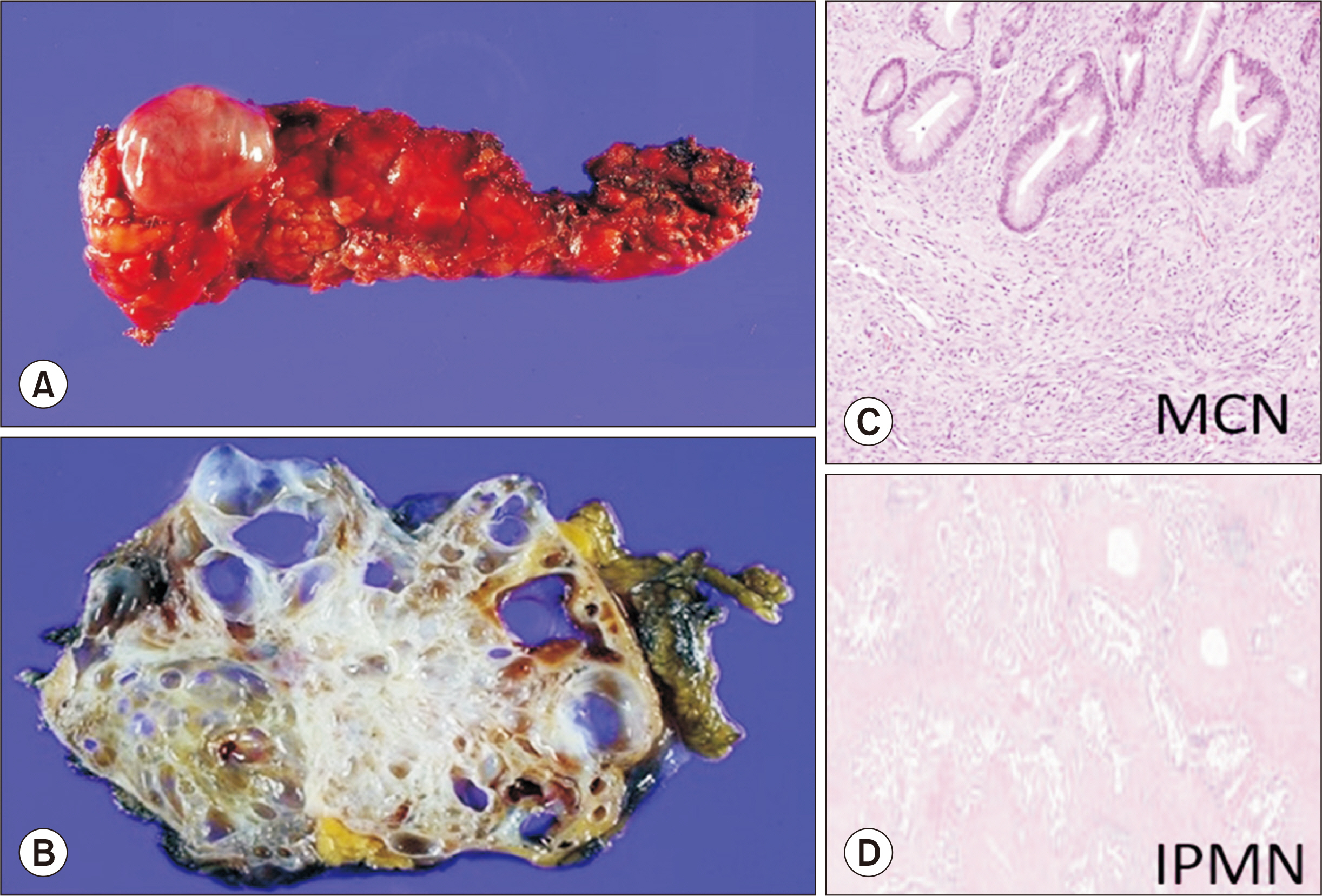
Figure
Reference
-
1. van Huijgevoort NC, Del Chiaro M, Wolfgang CL, van Hooft JE, Besselink MG. 2019; Diagnosis and management of pancreatic cystic neoplasms: current evidence and guidelines. Nat Rev Gastroenterol Hepatol. 16:676–89. DOI: 10.1038/s41575-019-0195-x. PMID: 31527862.2. Ip IK, Mortele KJ, Prevedello LM, Khorasani R. 2011; Focal cystic pancreatic lesions: assessing variation in radiologists' management recommendations. Radiology. 259:136–41. DOI: 10.1148/radiol.10100970. PMID: 21292867.3. Girometti R, Intini S, Brondani G, Como G, Londero F, Bresadola F, et al. 2011; Incidental pancreatic cysts on 3D turbo spin echo magnetic resonance cholangiopancreatography: prevalence and relation with clinical and imaging features. Abdom Imaging. 36:196–205. DOI: 10.1007/s00261-010-9618-4. PMID: 20473669.4. Chang YR, Park JK, Jang JY, Kwon W, Yoon JH, Kim SW. 2016; Incidental pancreatic cystic neoplasms in an asymptomatic healthy population of 21,745 individuals: large-scale, single-center cohort study. Medicine (Baltimore). 95:e5535. DOI: 10.1097/MD.0000000000005535. PMID: 28002329. PMCID: PMC5181813.5. de Jong K, Nio CY, Hermans JJ, Dijkgraaf MG, Gouma DJ, van Eijck CH, et al. 2010; High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol. 8:806–11. DOI: 10.1016/j.cgh.2010.05.017. PMID: 20621679.6. Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. 2012; International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 12:183–97. DOI: 10.1016/j.pan.2012.04.004. PMID: 22687371.7. Del Chiaro M, Verbeke C, Salvia R, Klöppel G, Werner J, McKay C, et al. 2013; European experts consensus statement on cystic tumours of the pancreas. Dig Liver Dis. 45:703–11. DOI: 10.1016/j.dld.2013.01.010. PMID: 23415799.8. Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. 2017; Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 17:738–53. DOI: 10.1016/j.pan.2017.07.007. PMID: 28735806.9. European Study Group on Cystic Tumours of the Pancreas. 2018; European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 67:789–804. DOI: 10.1136/gutjnl-2018-316027. PMID: 29574408. PMCID: PMC5890653.10. Al-Haddad M, Gill KR, Raimondo M, Woodward TA, Krishna M, Crook JE, et al. 2010; Safety and efficacy of cytology brushings versus standard fine-needle aspiration in evaluating cystic pancreatic lesions: a controlled study. Endoscopy. 42:127–32. DOI: 10.1055/s-0029-1215351. PMID: 19998218.11. Thomas T, Bebb J, Mannath J, Ragunath K, Kaye PV, Aithal GP. 2010; EUS-guided pancreatic cyst brushing: a comparative study in a tertiary referral centre. JOP. 11:163–9.12. Sendino O, Fernández-Esparrach G, Solé M, Colomo L, Pellisé M, Llach J, et al. 2010; Endoscopic ultrasonography-guided brushing increases cellular diagnosis of pancreatic cysts: a prospective study. Dig Liver Dis. 42:877–81. DOI: 10.1016/j.dld.2010.07.009. PMID: 20810331.13. Basar O. 2018; Pancreatic cyst biopsy: improvement in diagnosis with micro forceps biopsy. Cancer Cytopathol. 126:227–8. DOI: 10.1002/cncy.21975. PMID: 29405615.14. Stark A, Donahue TR, Reber HA, Hines OJ. 2016; Pancreatic cyst disease: a review. JAMA. 315:1882–93. DOI: 10.1001/jama.2016.4690. PMID: 27139061.15. Vidhyarkorn S, Siripongsakun S, Yu J, Sayre J, Agopian VG, Durazo F, et al. 2017; Longterm follow-up of small pancreatic cystic lesions in liver transplant recipients. Liver Transpl. 23:324–9. DOI: 10.1002/lt.24680. PMID: 27875639.16. Doycheva I, Amer S, Watt KD. 2016; De novo malignancies after transplantation: risk and surveillance strategies. Med Clin North Am. 100:551–67. DOI: 10.1016/j.mcna.2016.01.006. PMID: 27095645.17. Buell JF, Brock GN. 2008; Risk of cancer in liver transplant recipients: a look into the mirror. Liver Transpl. 14:1561–3. DOI: 10.1002/lt.21634. PMID: 18975288.18. Liu K, Joshi V, van Camp L, Yang QW, Baars JE, Strasser SI, et al. 2017; Prevalence and outcomes of pancreatic cystic neoplasms in liver transplant recipients. World J Gastroenterol. 23:8526–32. DOI: 10.3748/wjg.v23.i48.8526. PMID: 29358860. PMCID: PMC5752712.19. Lennon AM, Victor D, Zaheer A, Ostovaneh MR, Jeh J, Law JK, et al. 2014; Liver transplant patients have a risk of progression similar to that of sporadic patients with branch duct intraductal papillary mucinous neoplasms. Liver Transpl. 20:1462–7. DOI: 10.1002/lt.23983. PMID: 25155689. PMCID: PMC4322915.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and clinical significance of pancreatic cystic lesions in immunosuppressed patients with solid organ transplantation
- Role of contrast-enhanced harmonic endoscopic ultrasonography (EUS) and EUS elastography in pancreatic lesions
- Current Status of Solid Organ Xenotransplantation
- Pathologic Features of Pancreatic Cystic Neoplasms
- Management of Opportunistic Infections after Organ Transplantation