Prog Med Phys.
2022 Sep;33(3):25-35. 10.14316/pmp.2022.33.3.25.
Comparison of Dose Statistics of IntensityModulated Radiation Therapy Plan from Varian Eclipse Treatment Planning System with Novel Python-Based Indigenously Developed Software
- Affiliations
-
- 1Department of Radiation Oncology, Thangam Cancer Hospital, Namakkal, Tamil Nadu, India
- 2PG & Research, Department of Physics, Jamal Mohamed College (Autonomous), Affiliated to Bharathidasan University, Tiruchirappalli, Tamilnadu, India
- 3Department of Medical Physics, Hind Institute of Medical Sciences and Hospital, Lucknow, Uttar Pradesh, India
- 4Department of Radiation Oncology, KLES Belgaum Cancer Hospital, Belgaum, Karnataka, India
- 5Department of Medical Physics, Bharathidasan University,Trichy, India
- KMID: 2533865
- DOI: http://doi.org/10.14316/pmp.2022.33.3.25
Abstract
- Purpose
Planning for radiotherapy relies on implicit estimation of the probability of tumor control and the probability of complications in adjacent normal tissues for a given dose distribution.
Methods
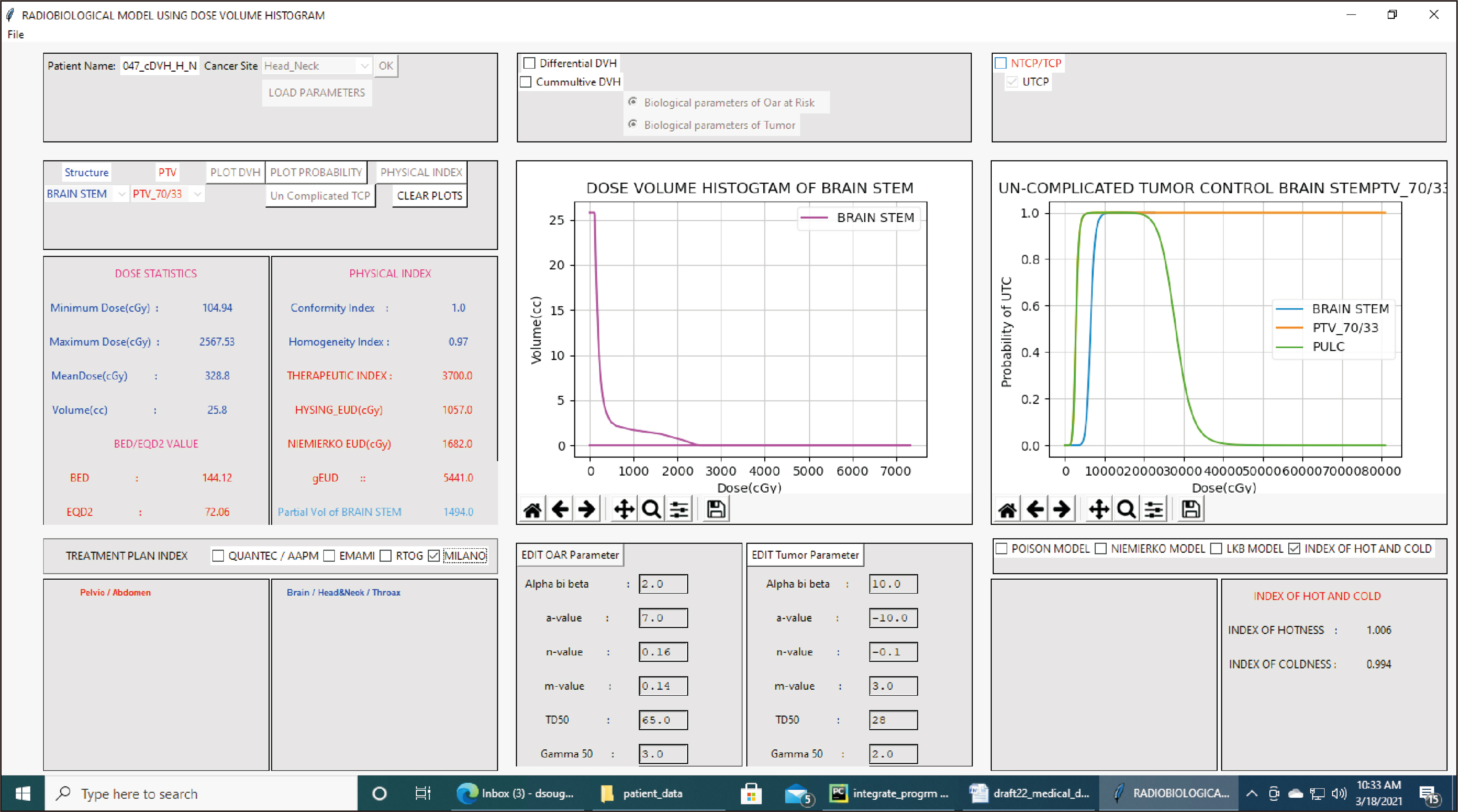
The aim of this pilot study was to reconstruct dose-volume histograms (DVHs) from text files generated by the Eclipse treatment planning system developed by Varian Medical Systems and to verify the integrity and accuracy of the dose statistics.
Results
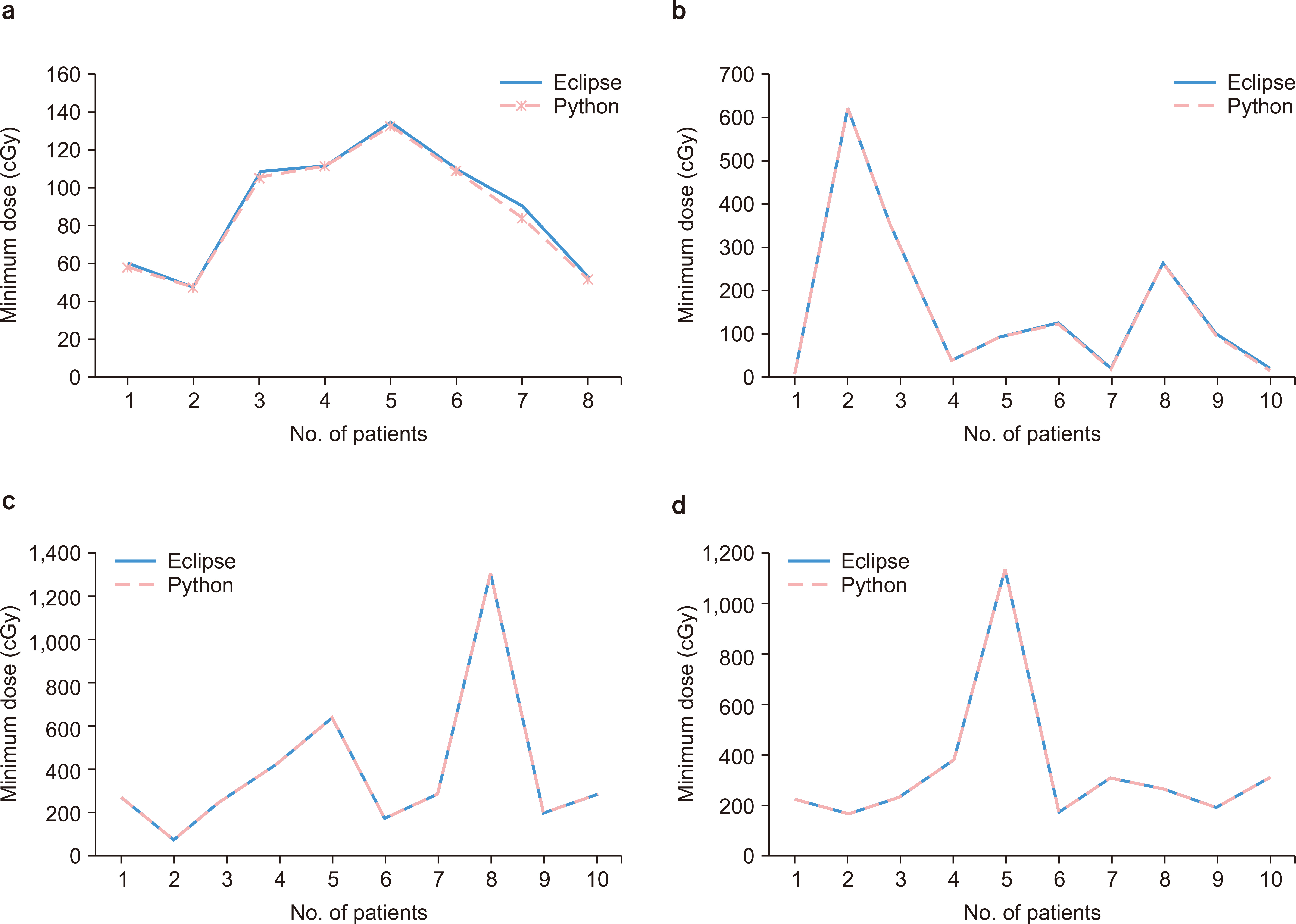
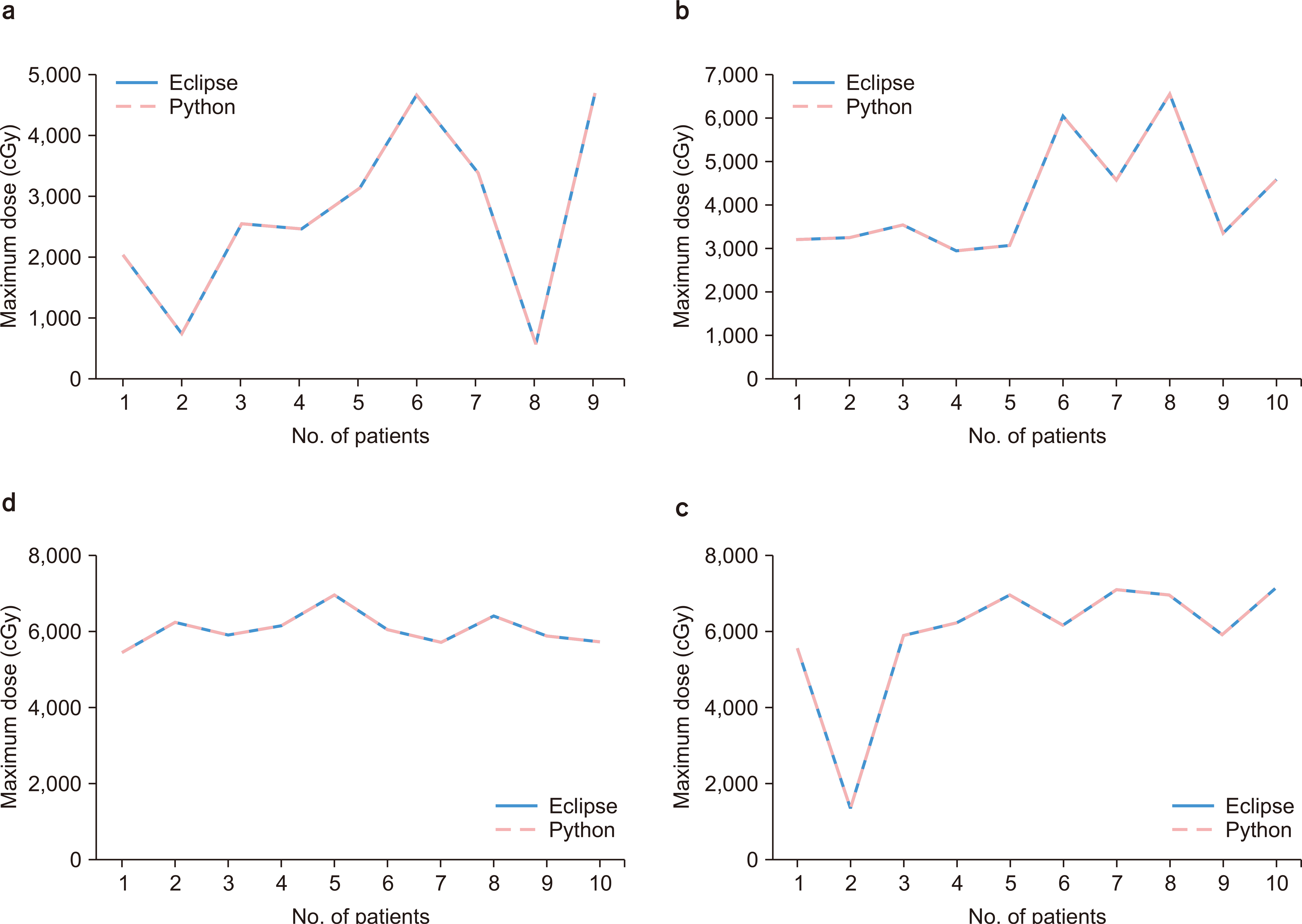
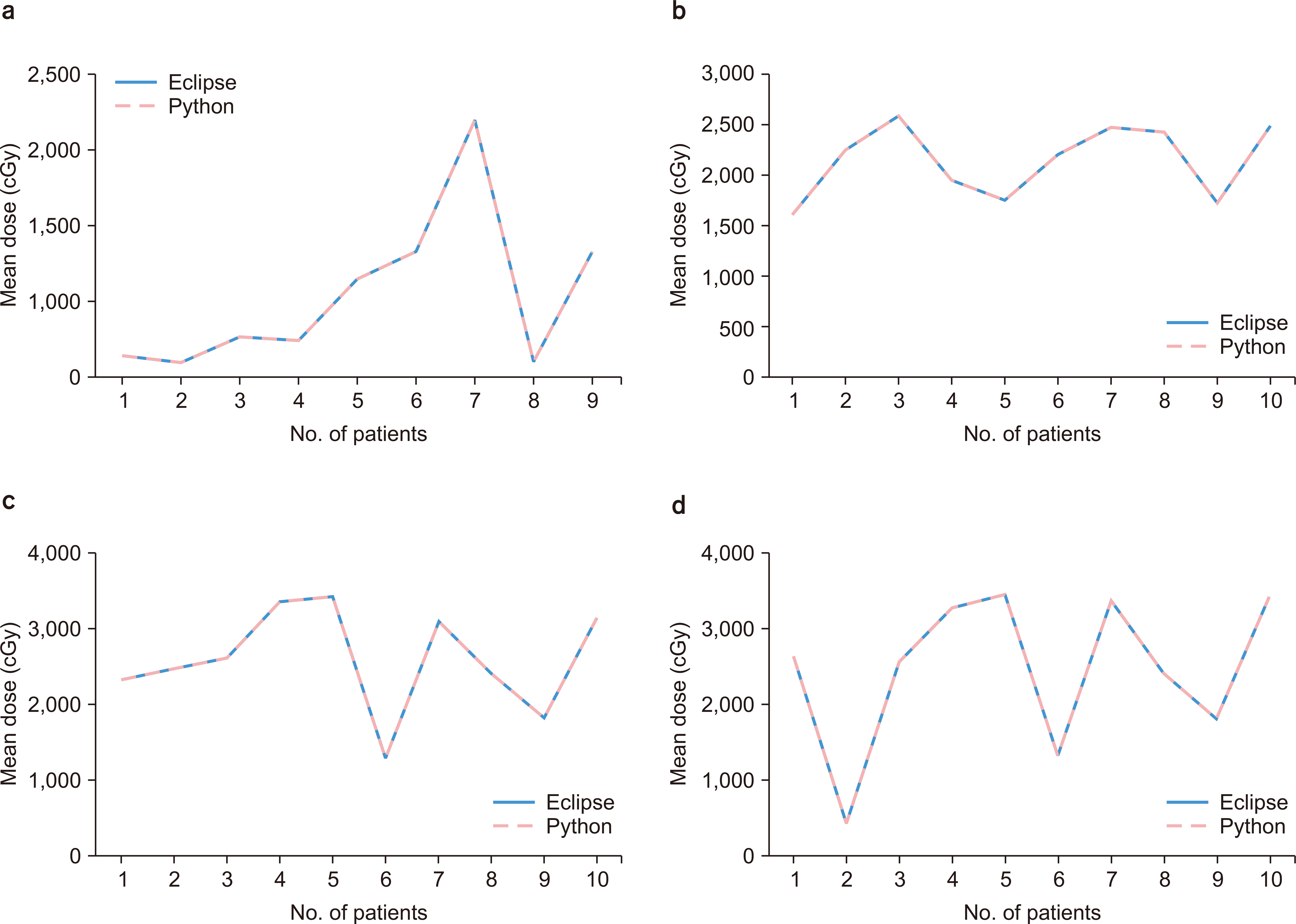
We further compared dose statistics for intensity-modulated radiotherapy of the head and neck between the Eclipse software and software developed in-house. The dose statistics data obtained from the Python software were consistent, with deviations from the Eclipse treatment planning system found to be within acceptable limits.
Conclusions
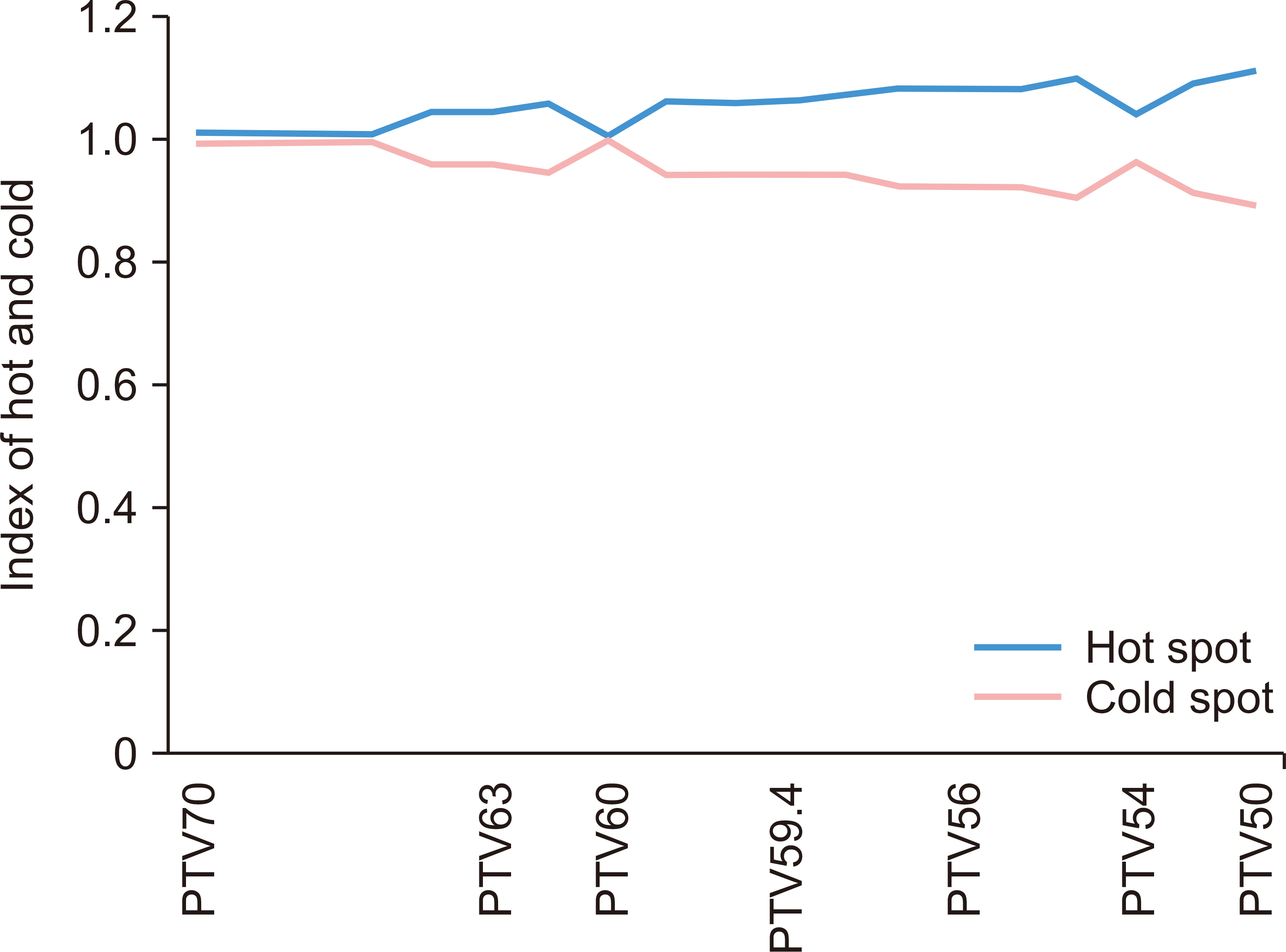
The in-house software was able to provide indices of hotness and coldness for treatment planning and store statistical data generated by the software in Oracle databases. We believe the findings of this pilot study may lead to more accurate evaluations in planning for radiotherapy.
Keyword
Figure
Reference
-
References
1. Zhao B, Joiner MC, Orton CG, Burmeister J. 2010; "SABER": a new software tool for radiotherapy treatment plan evaluation. Med Phys. 37:5586–5592. DOI: 10.1118/1.3497152. PMID: 21158270.
Article2. Deasy JO, Blanco AI, Clark VH. 2003; CERR: a computational environment for radiotherapy research. Med Phys. 30:979–985. DOI: 10.1118/1.1568978. PMID: 12773007.
Article3. The Histogram Analysis in Radiation Therapy (HART). 2014. An open source software system designed for clinical and research applications in radiation therapy (2008-2014). HART Research Group;Chicago: DOI: 10.1118/1.1568978.4. El Naqa I, Suneja G, Lindsay PE, Hope AJ, Alaly JR, Vicic M, et al. 2006; Dose response explorer: an integrated open-source tool for exploring and modelling radiotherapy dose-volume outcome relationships. Phys Med Biol. 51:5719–5735. DOI: 10.1088/0031-9155/51/22/001. PMID: 17068361.
Article5. Sanchez-Nieto B, Nahum AE. 2000; BIOPLAN: software for the biological evaluation of. Radiotherapy treatment plans. Med Dosim. 25:71–76. DOI: 10.1016/S0958-3947(00)00031-5. PMID: 10856684.
Article6. Bruzzaniti V, Abate A, Pedrini M, Benassi M, Strigari L. 2011; IsoBED: a tool for automatic calculation of biologically equivalent fractionation schedules in radiotherapy using IMRT with a simultaneous integrated boost (SIB) technique. J Exp Clin Cancer Res. 30:52. DOI: 10.1186/1756-9966-30-52. PMID: 21554675. PMCID: PMC3117739.
Article7. Lee S, Cao YJ. Kim CY: Physical and radiobiological evaluation of radiotherapy treatment plan. 2015. Evolution of Ionizing Radiation Research. IntechOpen;London: DOI: 10.5772/60846.8. Pyakuryal A, Myint WK, Gopalakrishnan M, Jang S, Logemann JA, Mittal BB. 2010; A computational tool for the efficient analysis of dose-volume histograms from radiation therapy treatment plans. J Appl Clin Med Phys. 11:3013. DOI: 10.1120/jacmp.v11i1.3013. PMID: 20160690. PMCID: PMC2897015.9. Kim JS, Yoon M, Park SY, Shin JS, Shin E, Ju SG, et al. 2009; A dose volume histogram analyzer program for external beam radiotherapy. J Korean Soc Ther Radiol Oncol. 27:240–248. DOI: 10.3857/jkstro.2009.27.4.240.
Article10. Park YK, Park S, Wu HG, Kim S. 2014; A new plan quality index for dose painting radiotherapy. J Appl Clin Med Phys. 15:4941. DOI: 10.1120/jacmp.v15i4.4941. PMID: 25207424. PMCID: PMC5875497.
Article11. Lee TF, Chao PJ, Wang HY, Hsu HC, Chang P, Chen WC. 2012; Normal tissue complication probability model parameter estimation for xerostomia in head and neck cancer patients based on scintigraphy and quality of life assessments. BMC Cancer. 12:567. DOI: 10.1186/1471-2407-12-567. PMID: 23206972. PMCID: PMC3536655.
Article12. Warkentin B, Stavrev P, Stavreva N, Field C, Fallone BG. 2004; A TCP-NTCP estimation module using DVHs and known radiobiological models and parameter sets. J Appl Clin Med Phys. 5:50–63. DOI: 10.1120/jacmp.v5i1.1970. PMID: 15753933. PMCID: PMC5723441.
Article13. Alfonso JC, Herrero MA, Núñez L. 2015; A dose-volume histogram based decision-support system for dosimetric comparison of radiotherapy treatment plans. Radiat Oncol. 10:263. DOI: 10.1186/s13014-015-0569-3. PMID: 26715096. PMCID: PMC4696205.
Article14. Gay HA, Niemierko A. 2007; A free program for calculating EUD-based NTCP and TCP in external beam radiotherapy. Phys Med. 23:115–125. DOI: 10.1016/j.ejmp.2007.07.001. PMID: 17825595.
Article15. Oinam AS, Singh L, Shukla A, Ghoshal S, Kapoor R, Sharma SC. 2011; Dose volume histogram analysis and comparison of different radiobiological models using in-house developed software. J Med Phys. 36:220–229. DOI: 10.4103/0971-6203.89971. PMID: 22228931. PMCID: PMC3249733.
Article16. Pasciuti K, Iaccarino G, Strigari L, Malatesta T, Benassi M, Di Nallo AM, et al. 2011; Tissue heterogeneity in IMRT dose calculation for lung cancer. Med Dosim. 36:219–227. DOI: 10.1016/j.meddos.2010.03.008. PMID: 20970989.
Article17. Kutcher GJ, Burman C, Brewster L, Goitein M, Mohan R. 1991; Histogram reduction method for calculating complication probabilities for three-dimensional treatment planning evaluations. Int J Radiat Oncol Biol Phys. 21:137–146. DOI: 10.1016/0360-3016(91)90173-2. PMID: 2032884.
Article18. Kataria T, Sharma K, Subramani V, Karrthick KP, Bisht SS. 2012; Homogeneity Index: an objective tool for assessment of conformal radiation treatments. J Med Phys. 37:207–213. DOI: 10.4103/0971-6203.103606. PMID: 23293452. PMCID: PMC3532749.
Article19. Cheung MLM, Kan MWK, Yeung VTY, Poon DMC, Kam MKM, Lee LKY, et al. 2021; Analysis of hepatocellular carcinoma stereotactic body radiation therapy dose prescription method using uncomplicated tumor control probability model. Adv Radiat Oncol. 6:100739. DOI: 10.1016/j.adro.2021.100739. PMID: 34355107. PMCID: PMC8321929.
Article20. Kutcher GJ, Burman C. 1989; Calculation of complication probability factors for non-uniform normal tissue irradiation: the effective volume method. Int J Radiat Oncol Biol Phys. 16:1623–1630. DOI: 10.1016/0360-3016(89)90972-3. PMID: 2722599.
Article21. Marks LB, Yorke ED, Jackson A, Ten Haken RK, Constine LS, Eisbruch A, et al. 2010; Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 76(3 Suppl):S10–S19. DOI: 10.1016/j.ijrobp.2009.07.1754. PMID: 20171502. PMCID: PMC4041542.
Article22. Wu Q, Manning M, Schmidt-Ullrich R, Mohan R. 2000; The potential for sparing of parotids and escalation of biologically effective dose with intensity-modulated radiation treatments of head and neck cancers: a treatment design study. Int J Radiat Oncol Biol Phys. 46:195–205. DOI: 10.1016/S0360-3016(99)00304-1. PMID: 10656393.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Intensity Modulated Radiation Therapy Dose Calculations with a PBC and AAA Algorithms in the Lung Cancer
- A Study of Energy Dependency in Intensity Modulated Radiation Therapy of Lung Cancer
- A Comparison Study of Volumetric Modulated Arc Therapy Quality Assurances Using Portal Dosimetry and MapCHECK 2
- Institutional Applications of Eclipse Scripting Programming Interface to Clinical Workflows in Radiation Oncology
- Property of Dose Distribution in Accordance with Dose Rate Variation in Intensity Modulated Radiation Therapy