J Korean Med Sci.
2022 Oct;37(38):e281. 10.3346/jkms.2022.37.e281.
Long-Term Changes in HbA1c According to Blood Glucose Control Status During the First 3 Months After Visiting a Tertiary University Hospital
- Affiliations
-
- 1College of Pharmacy, Sookmyung Women’s University, Seoul, Korea
- 2Department of Biostatistics, Clinical Research Coordinating Center, Catholic Medical Center, The Catholic University of Korea, Seoul, Korea
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Medical Informatics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2533562
- DOI: http://doi.org/10.3346/jkms.2022.37.e281
Abstract
- Background
We evaluated patients visiting a tertiary university hospital due to a diagnosis of diabetes with a goal of achieving blood glucose control and evaluated blood glucose persistence over 7 years according to the change in blood glucose evident at 3 months after the first visit.
Methods
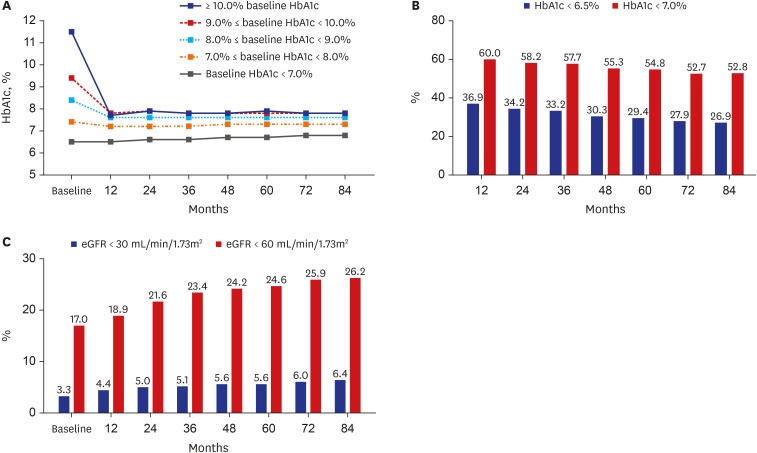
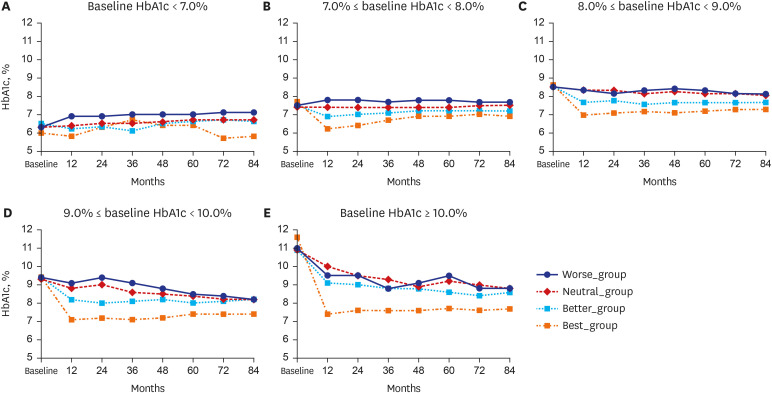
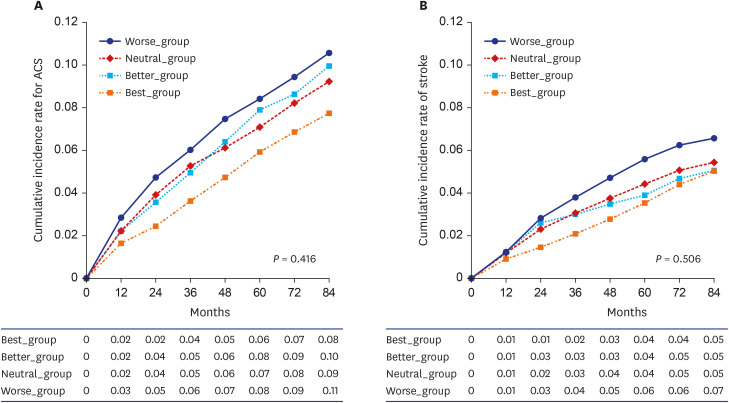
Patients treated from 2009 to 2013 were categorized into four groups according to the change in HbA1c levels during the first 3 months of follow-up (Best_group, ≥ 1.6% decrease; Better_group, 0.5–1.5% decrease; Neutral_group, maintained at −0.4% to +0.4%; Worse_group, ≥ 0.5% increase). Each patient’s blood glucose control status was then monitored for 7 years. The incidence of stroke and acute coronary syndrome during this period was confirmed.
Results
Overall, 9,776 patients were included. HbA1c values were lower in the Best_group than in the other groups at all time points (all P < 0.001). The rate of reaching targets of < 6.5% or < 7.0% HbA1c decreased over time; the rate at which the estimated glomerular filtration rate decreased to < 30 or < 60 mL/min/1.73m 2 increased over time (all trends, P < 0.01).
Conclusion
Blood glucose control status in the first 3 months after initiating hospital care enabled estimation of the patient’s glycemic control status for the next 7 years. In cases with poor initial blood glucose control, a new or more active method of blood glucose control should be sought.
Keyword
Figure
Cited by 1 articles
-
The Degree of Glycemic Control for the First Three Months Determines the Next Seven Years
Nami Lee, Dae Jung Kim
J Korean Med Sci. 2022;37(38):e301. doi: 10.3346/jkms.2022.37.e301.
Reference
-
1. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843. PMID: 31518657.
Article2. Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018; 138:271–281. PMID: 29496507.
Article3. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021; 45(1):1–10. PMID: 33434426.
Article4. Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993; 329(14):977–986. PMID: 8366922.
Article5. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352(9131):837–853. PMID: 9742976.6. Laiteerapong N, Ham SA, Gao Y, Moffet HH, Liu JY, Huang ES, et al. The legacy effect in type 2 diabetes: impact of early glycemic control on future complications (the diabetes & aging study). Diabetes Care. 2019; 42(3):416–426. PMID: 30104301.
Article7. Kim KJ, Burns LR. Success factors in hospital network performance: evidence from Korea. Health Serv Manage Res. 2007; 20(3):141–152. PMID: 17683653.
Article8. Seo DH, Kang S, Lee YH, Ha JY, Park JS, Lee BW, et al. Current management of type 2 diabetes mellitus in primary care clinics in Korea. Endocrinol Metab (Seoul). 2019; 34(3):282–290. PMID: 31565881.
Article9. Lim DJ, Kwon HS, Kim HS, Lee JH, Ko SH, Lee JM, et al. Clinical characteristics of the diabetic patients managed at the different medical institutions in Seoul and Gyeonggi province. Korean J Med. 2006; 71(2):173–181.10. Park J, Kwon S, Choi EK, Choi Y, Lee E, Choe W, et al. Validation of diagnostic codes of major clinical outcomes in a National Health Insurance database. Int J Arrhythmia. 2019; 20(1):5.
Article11. Park TH, Choi JC. Validation of stroke and thrombolytic therapy in Korean National Health Insurance claim data. J Clin Neurol. 2016; 12(1):42–48. PMID: 26365022.
Article12. Shin SY, Kim HS. Data pseudonymization in a range that does not affect data quality: correlation with the degree of participation of clinicians. J Korean Med Sci. 2021; 36(44):e299. PMID: 34783216.
Article13. Li D, Zou H, Yin P, Li W, He J, Wang S, et al. Durability of glycaemic control in type 2 diabetes: a systematic review and meta-analysis for its association with body weight changes. Diabetes Obes Metab. 2021; 23(1):208–217. PMID: 33016522.
Article14. Balkau B, Calvi-Gries F, Freemantle N, Vincent M, Pilorget V, Home PD. Predictors of HbA1c over 4 years in people with type 2 diabetes starting insulin therapies: the CREDIT study. Diabetes Res Clin Pract. 2015; 108(3):432–440. PMID: 25818885.
Article15. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008; 358(24):2560–2572. PMID: 18539916.
Article16. Zoungas S, Chalmers J, Neal B, Billot L, Li Q, Hirakawa Y, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med. 2014; 371(15):1392–1406. PMID: 25234206.17. Lenzen M, Ryden L, Ohrvik J, Bartnik M, Malmberg K, Scholte Op Reimer W, et al. Diabetes known or newly detected, but not impaired glucose regulation, has a negative influence on 1-year outcome in patients with coronary artery disease: a report from the Euro Heart Survey on diabetes and the heart. Eur Heart J. 2006; 27(24):2969–2974. PMID: 17090612.
Article18. Folz R, Laiteerapong N. The legacy effect in diabetes: are there long-term benefits? Diabetologia. 2021; 64(10):2131–2137. PMID: 34392398.
Article19. Murray P, Chune GW, Raghavan VA. Legacy effects from DCCT and UKPDS: what they mean and implications for future diabetes trials. Curr Atheroscler Rep. 2010; 12(6):432–439. PMID: 20652839.20. Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol. 2018; 6(2):130–142. PMID: 28970034.
Article21. Kim HS, Kim DJ, Yoon KH. Medical big data is not yet available: why we need realism rather than exaggeration. Endocrinol Metab (Seoul). 2019; 34(4):349–354. PMID: 31884734.
Article22. Kim HS, Kim JH. Proceed with caution when using real world data and real world evidence. J Korean Med Sci. 2019; 34(4):e28. PMID: 30686950.
Article23. Kyoung DS, Kim HS. Understanding and Utilizing Claim Data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) Database for Research. J Lipid Atheroscler. 2022; 11(2):103–110. PMID: 35656154.24. Kang DY, Kim H, Ko S, Kim H, Shinn J, Kang MG, et al. Sodium-glucose cotransporter-2 inhibitor-related diabetic ketoacidosis: accuracy verification of operational definition. J Korean Med Sci. 2022; 37(7):e53. PMID: 35191230.
Article25. Ko S, Kim H, Shinn J, Byeon SJ, Choi JH, Kim HS. Estimation of sodium-glucose cotransporter 2 inhibitor-related genital and urinary tract infections via electronic medical record-based common data model. J Clin Pharm Ther. 2021; 46(4):975–983. PMID: 33565150.
Article26. Kim HS, Lee S, Kim JH. Real-world evidence versus randomized controlled trial: clinical research based on electronic medical records. J Korean Med Sci. 2018; 33(34):e213. PMID: 30127705.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- HbA1c Variability and Micro- and Macrovascular Complications of Diabetes
- Glycemic control of type 2 diabetic patients after short-term zinc supplementation
- Time in Range from Continuous Glucose Monitoring: A Novel Metric for Glycemic Control
- A Survey of Blood Glucose Testing, Medication, Diet, and Exercise Adherence in Korean Patients with Type2 Diabetes
- Relationship between Food-frequency and Glycated Hemoglobin in Korean Diabetics: Using Data from the 4th Korea National Health and Nutrition Examination Survey