Anat Cell Biol.
2022 Sep;55(3):277-283. 10.5115/acb.22.001.
Computed tomographic assessment of the lacrimal sac fossa in southwest population of Iran
- Affiliations
-
- 1Department of Radiology, Faculty of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 2Department of Ophthalmology, Faculty of Medicine, Infectious Ophthalmic Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 3Department of Anatomical Sciences, Faculty of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran
- KMID: 2533351
- DOI: http://doi.org/10.5115/acb.22.001
Abstract
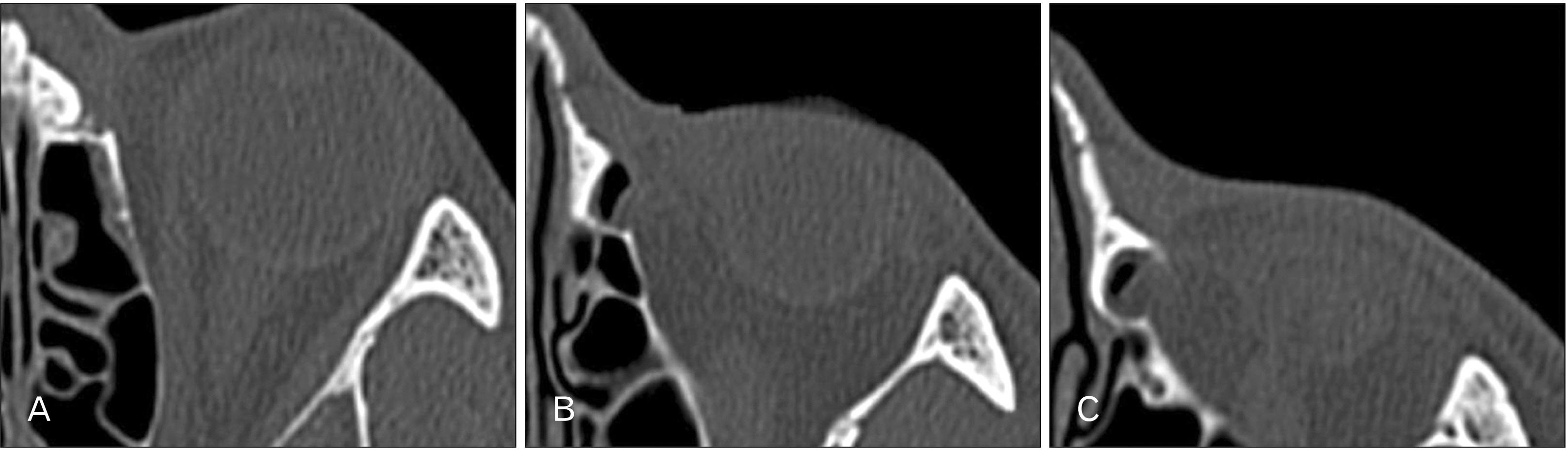
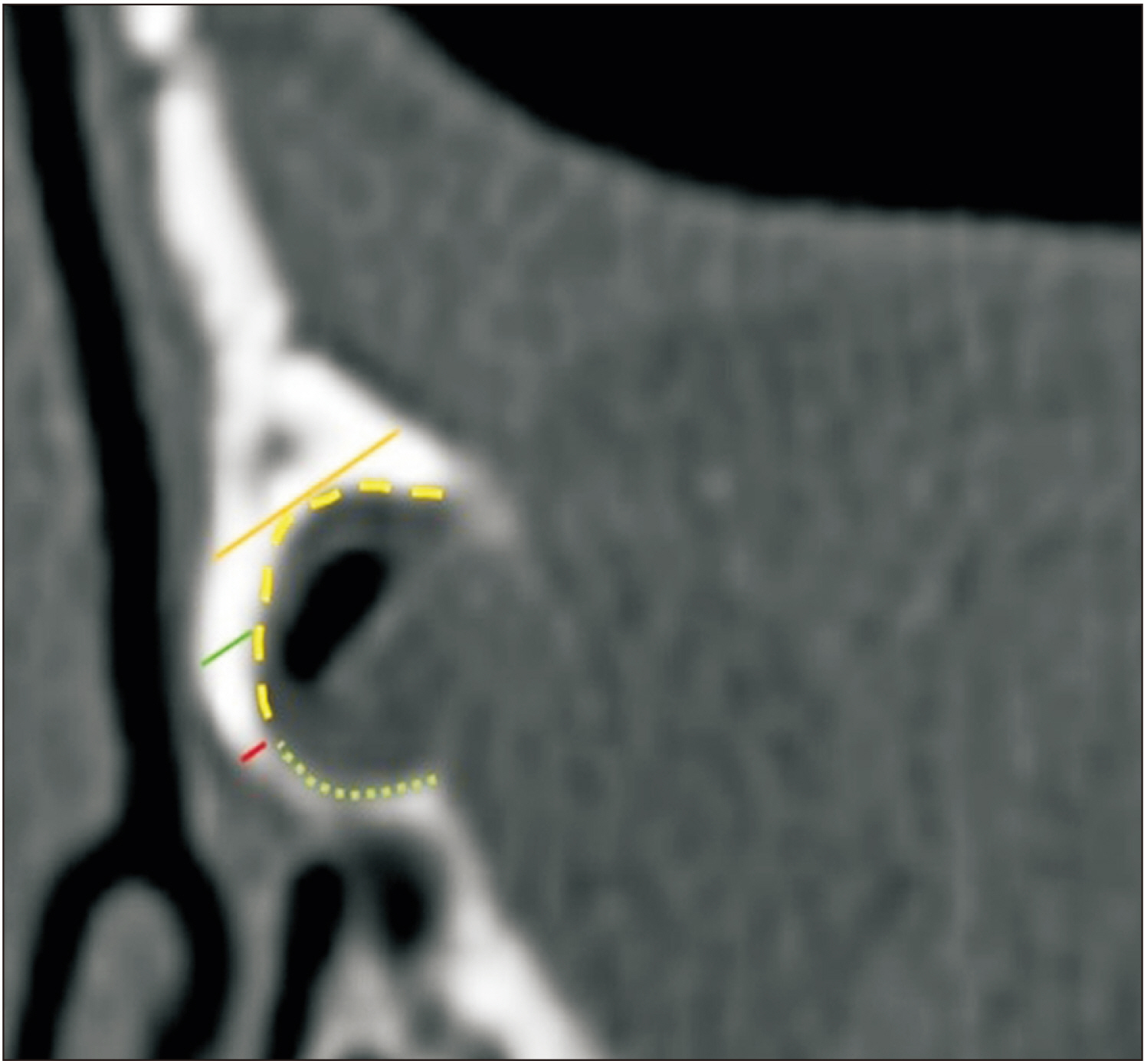
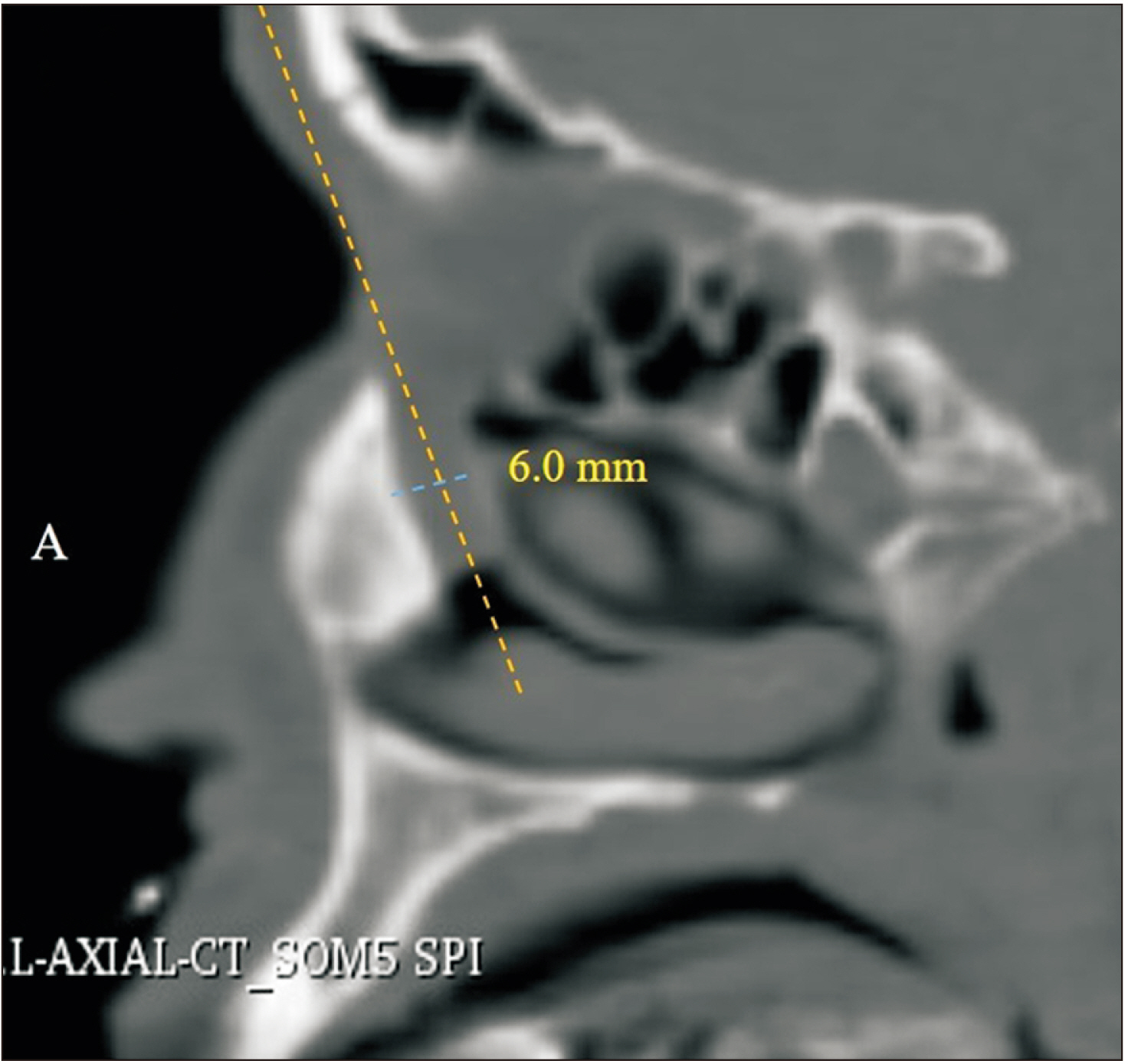
- To determine the morphology of the lacrimal sac fossa and bony nasolacrimal duct using computed tomography for obtaining detailed anatomical understanding of the drainage system and utilizing these measurements in planning for dacryocystorhinostomy (DCR) and nasolacrimal duct (NLD) obstruction in normal southwest (SW) population of Iran. One-hundred-sixty-five cases referred for the diagnosis of neuro-ophthalmic conditions were retrospectively studied. Measurements of lacrimal sac fossa were taken on three anatomical sections (upper, middle, and lower planes) utilizing a digital caliper/protractor instrument. Lacrimal thickness and two measurements of maxillary bone thickness were taken at each plane—namely, the “midpoint thickness” and the “maximum thickness.” The anterior extent of the nasal mucosa and NLD width was also evaluated. The mean maximum thickness of the maxillary bone at the three anatomical planes of the lacrimal sac fossa was 4.07 mm, 4.78 mm, and 5.60 mm, respectively. The midpoint thickness of the maxillary bone at each plane was 2.38 mm, 1.99 mm, and 1.68 mm, respectively, in both sexs. The lacrimal bone thickness at each level was 0.76 mm, 0.69 mm, and 0.67 mm, respectively. The proportion of the lacrimal sac fossa comprising the lacrimal bone at lower plane was 43.57% and showed a positive correlation with age (P=0.01). The mean anteroposterior bony nasolacrimal diameter was 5.94 mm with no significant difference between patient sex and age. According to the results, its indicate that performing an osteotomy during DCR could be easier in the Iranian SW population compared to other ethnics.
Figure
Reference
-
References
1. Hartikainen J, Aho HJ, Seppä H, Grenman R. 1996; Lacrimal bone thickness at the lacrimal sac fossa. Ophthalmic Surg Lasers. 27:679–84. DOI: 10.3928/1542-8877-19960801-07. PMID: 8858634.
Article2. Shams PN, Abed SF, Shen S, Adds PJ, Uddin JM. 2012; A cadaveric study of the morphometric relationships and bony composition of the caucasian nasolacrimal fossa. Orbit. 31:159–61. DOI: 10.3109/01676830.2011.648809. PMID: 22551366.
Article3. Valencia MRP, Takahashi Y, Naito M, Nakano T, Ikeda H, Kakizaki H. 2019; Lacrimal drainage anatomy in the Japanese population. Ann Anat. 223:90–9. DOI: 10.1016/j.aanat.2019.01.013. PMID: 30797973.
Article4. Rajak SN, Psaltis AJ. 2019; Anatomical considerations in endoscopic lacrimal surgery. Ann Anat. 224:28–32. DOI: 10.1016/j.aanat.2019.03.010. PMID: 30953809.
Article5. Yang JW, Oh HN. 2012; Success rate and complications of endonasal dacryocystorhinostomy with unciformectomy. Graefes Arch Clin Exp Ophthalmol. 250:1509–13. DOI: 10.1007/s00417-012-1992-x. PMID: 22623114. PMCID: PMC3460168.
Article6. Gupta N. Gupta N, editor. 2021. Complications of endoscopic dacryocystorhinostomy. Endoscopic Dacryocystorhinostomy. Springer;Singapore: p. 167–75. DOI: 10.1007/978-981-15-8112-0_12. PMCID: PMC9128314.
Article7. Sarbajna T, Takahashi Y, Valencia MRP, Ito M, Nishimura K, Kakizaki H. 2019; Computed tomographic assessment of the lacrimal sac fossa in the Japanese population. Ann Anat. 224:23–7. DOI: 10.1016/j.aanat.2019.03.008. PMID: 30953810.
Article8. Yong AM, Zhao DB, Siew SC, Goh PS, Liao J, Amrith S. 2014; Assessment of bony nasolacrimal parameters among Asians. Ophthalmic Plast Reconstr Surg. 30:322–7. DOI: 10.1097/IOP.0000000000000101. PMID: 25069069.
Article9. Lin Z, Kamath N, Malik A. 2021; Morphometric differences in normal bony nasolacrimal anatomy: comparison between four ethnic groups. Surg Radiol Anat. 43:179–85. DOI: 10.1007/s00276-020-02614-4. PMID: 33184673.
Article10. Gore SK, Naveed H, Hamilton J, Rene C, Rose GE, Davagnanam I. 2015; Radiological comparison of the lacrimal sac fossa anatomy between black Africans and Caucasians. Ophthalmic Plast Reconstr Surg. 31:328–31. DOI: 10.1097/IOP.0000000000000457. PMID: 26039331.
Article11. Woo KI, Maeng HS, Kim YD. 2011; Characteristics of intranasal structures for endonasal dacryocystorhinostomy in asians. Am J Ophthalmol. 152:491–8.e1. DOI: 10.1016/j.ajo.2011.02.019. PMID: 21669403.
Article12. Kang D, Park J, Na J, Lee H, Baek S. 2017; Measurement of lacrimal sac fossa using orbital computed tomography. J Craniofac Surg. 28:125–8. DOI: 10.1097/SCS.0000000000003262. PMID: 27930466.
Article13. Purevdorj B, Dugarsuren U, Tuvaan B, Jamiyanjav B. 2021; Anatomy of lacrimal sac fossa affecting success rate in endoscopic and external dacryocystorhinostomy surgery in Mongolians. Anat Cell Biol. 54:441–7. DOI: 10.5115/acb.21.081. PMID: 34620735. PMCID: PMC8693133.
Article14. Örge FH, Boente CS. 2014; The lacrimal system. Pediatr Clin North Am. 61:529–39. DOI: 10.1016/j.pcl.2014.03.002. PMID: 24852150.
Article15. Tao H, Ma ZZ, Wu HY, Wang P, Han C. 2014; Anatomic study of the lacrimal fossa and lacrimal pathway for bypass surgery with autogenous tissue grafting. Indian J Ophthalmol. 62:419–23. DOI: 10.4103/0301-4738.121137. PMID: 24817745. PMCID: PMC4064215.
Article16. Yung MW, Logan BM. 1999; The anatomy of the lacrimal bone at the lateral wall of the nose: its significance to the lacrimal surgeon. Clin Otolaryngol Allied Sci. 24:262–5. DOI: 10.1046/j.1365-2273.1999.00235.x. PMID: 10472456.
Article17. Agarwal M, Kumar V. 2012; Morphological study of fossa for lacrimal sac: contributions by lacrimal and maxilla. J Anat Soc India. 61:234–41. DOI: 10.1016/S0003-2778(12)80037-2.
Article18. Amanolahi S. 2005; A note on ethnicity and ethnic groups in Iran. Iran Cauc. 9:37–41. DOI: 10.1163/1573384054068105.
Article19. Janssen AG, Mansour K, Bos JJ, Castelijns JA. 2001; Diameter of the bony lacrimal canal: normal values and values related to nasolacrimal duct obstruction: assessment with CT. AJNR Am J Neuroradiol. 22:845–50. PMID: 11337326. PMCID: PMC8174956.20. Groessl SA, Sires BS, Lemke BN. 1997; An anatomical basis for primary acquired nasolacrimal duct obstruction. Arch Ophthalmol. 115:71–4. Erratum in: Arch Ophthalmol 1997;115:655. DOI: 10.1001/archopht.1997.01100150073012. PMID: 9006428.
Article21. Bulbul E, Yazici A, Yanik B, Yazici H, Demirpolat G. 2016; Morphometric evaluation of bony nasolacrimal canal in a caucasian population with primary acquired nasolacrimal duct obstruction: a multidetector computed tomography study. Korean J Radiol. 17:271–6. DOI: 10.3348/kjr.2016.17.2.271. PMID: 26957913. PMCID: PMC4781767.
Article22. Park JH, Huh JA, Piao JF, Lee H, Baek SH. 2019; Measuring nasolacrimal duct volume using computed tomography images in nasolacrimal duct obstruction patients in Korean. Int J Ophthalmol. 12:100–5. DOI: 10.18240/ijo.2019.01.16. PMID: 30662848. PMCID: PMC6326919.
Article23. McCormick A, Sloan B. 2009; The diameter of the nasolacrimal canal measured by computed tomography: gender and racial differences. Clin Exp Ophthalmol. 37:357–61. DOI: 10.1111/j.1442-9071.2009.02042.x. PMID: 19594561.
Article24. Ali MJ, Paulsen F. 2019; Etiopathogenesis of primary acquired nasolacrimal duct obstruction: what we know and what we need to know. Ophthalmic Plast Reconstr Surg. 35:426–33. DOI: 10.1097/IOP.0000000000001310. PMID: 30730434.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed tomographic assessment of the lacrimal sac fossa in southwest population of Iran
- Computed Tomographic Dacfyocystography using Rayvist(R)
- Anatomy of lacrimal sac fossa affecting success rate in endoscopic and external dacryocystorhinostomy surgery in Mongolians
- A Case of Primary Neurofibroma of Lacrimal Sac
- Rhabdomyosarcoma of The Lacrimal Sac in 32-year-old Man