J Korean Med Sci.
2022 Sep;37(36):e273. 10.3346/jkms.2022.37.e273.
Measurement and Control of Surgical Smoke to Enhance Surgical Team Safety
- Affiliations
-
- 1Department of Surgery, Myongji Hospital, Goyang, Korea
- KMID: 2533228
- DOI: http://doi.org/10.3346/jkms.2022.37.e273
Abstract
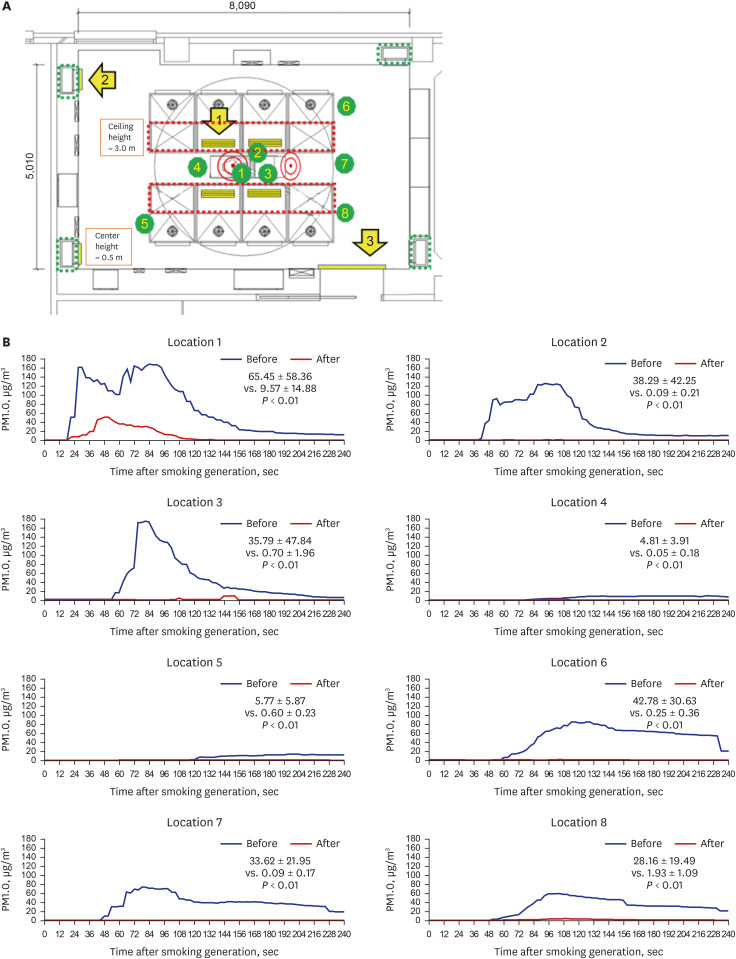
- Amid the coronavirus disease 2019 era, concern about the safety of surgical teams related to surgical smoke (SS) is rising. As simple ventilation improvement methods (SVIMs), we replaced 4 of the 8 supply diffusers with a direction-adjustable louver-type, closed 2 of the 4 exhaust grills, and strengthened the sealing of the doorway. Dynamic changes in the concentration of particulate matter (PM) with sizes of < 1.0 μm (PM1.0) were measured using low-cost PM meters (LCPMs) at eight locations in the operating room (OR). SS concentration up to 4 minutes at the location of the surgeon, first assistant, and scrub nurse before and after SVIMs application decreased from 65.4, 38.2, 35.7 µg/m 3 to 9.5, 0.1 and 0.7 µg/m 3 respectively. A similar decrease was observed in the other 5 locations. SVIMs could effectively control SS and the LCPM was also effective in measuring SS in the OR or other spaces of the hospital.
Figure
Reference
-
1. Gupta N, Agrawal H. COVID 19 and laparoscopic surgeons, the Indian scenario - Perspective. Int J Surg. 2020; 79:165–167. PMID: 32479915.
Article2. Sowerby LJ, Nichols AC, Gibson R, Sommer DD, Moore C, Fraser DD, et al. Assessing the risk of SARS-CoV-2 transmission via surgical electrocautery plume. JAMA Surg. 2021; 156(9):883–885. PMID: 34019099.
Article3. Bivolarova M, Ondráček J, Melikov A, Ždímal V. A comparison between tracer gas and aerosol particles distribution indoors: the impact of ventilation rate, interaction of airflows, and presence of objects. Indoor Air. 2017; 27(6):1201–1212. PMID: 28378912.
Article4. Mowbray NG, Ansell J, Horwood J, Cornish J, Rizkallah P, Parker A, et al. Safe management of surgical smoke in the age of COVID-19. Br J Surg. 2020; 107(11):1406–1413. PMID: 32363596.
Article5. Cho EM, Jeon HJ, Yoon DK, Park SH, Hong HJ, Choi KY, et al. Reliability of low-cost, sensor-based fine dust measurement devices for monitoring atmospheric particulate matter concentrations. Int J Environ Res Public Health. 2019; 16(8):1430.
Article6. Kai T, Ayagaki N, Setoguchi H. Influence of the arrangement of surgical light axes on the air environment in operating rooms. J Healthc Eng. 2019; 2019:4861273. PMID: 31049187.
Article7. Smyth ET, Humphreys H, Stacey A, Taylor EW, Hoffman P, Bannister G. Survey of operating theatre ventilation facilities for minimally invasive surgery in Great Britain and Northern Ireland: current practice and considerations for the future. J Hosp Infect. 2005; 61(2):112–122. PMID: 16240467.
Article8. World Health Organization. Global Guidelines on the Prevention of Surgical Site Infection. Geneva: World Health Organization;2016.9. Hofer V, Kriegel M. Exposure of operating room surgical staff to surgical smoke under different ventilation schemes. Indoor Air. 2021; 32(1):e12947. PMID: 34704629.
Article10. Chow TT, Kwan A, Lin Z, Bai W. A computer evaluation of ventilation performance in a negative-pressure operating theater. Anesth Analg. 2006; 103(4):913–918. PMID: 17000803.
Article11. Badura M, Batog P, Drzeniecka-Osiadacz A, Modzel P. Evaluation of low-cost sensors for ambient PM2.5 monitoring. J Sens. 2018; 2018:1–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New Concept of a Surgical Hospitalist: Early Experience of Managing the Admission, Critical Care, Trauma Surgery Team
- Experience of Communication for Patient Safety by Perioperative Nurses
- Patient Safety Education: Team Communication and Interprofessional Collaboration
- Prevention of wrong site, wrong procedure, wrong patient surgery and time-out
- Does surgical smoke matter?