J Korean Foot Ankle Soc.
2022 Sep;26(3):136-142. 10.14193/jkfas.2022.26.3.136.
Comparison between Surgical and Conservative Treatments in Isolated Lateral Compartment Syndrome of the Lower Leg: A Case Report
- Affiliations
-
- 1Busan Gunwoo Orthopedic Clinic, Busan, Korea
- 2Department of Orthopedic Surgery, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2533196
- DOI: http://doi.org/10.14193/jkfas.2022.26.3.136
Abstract
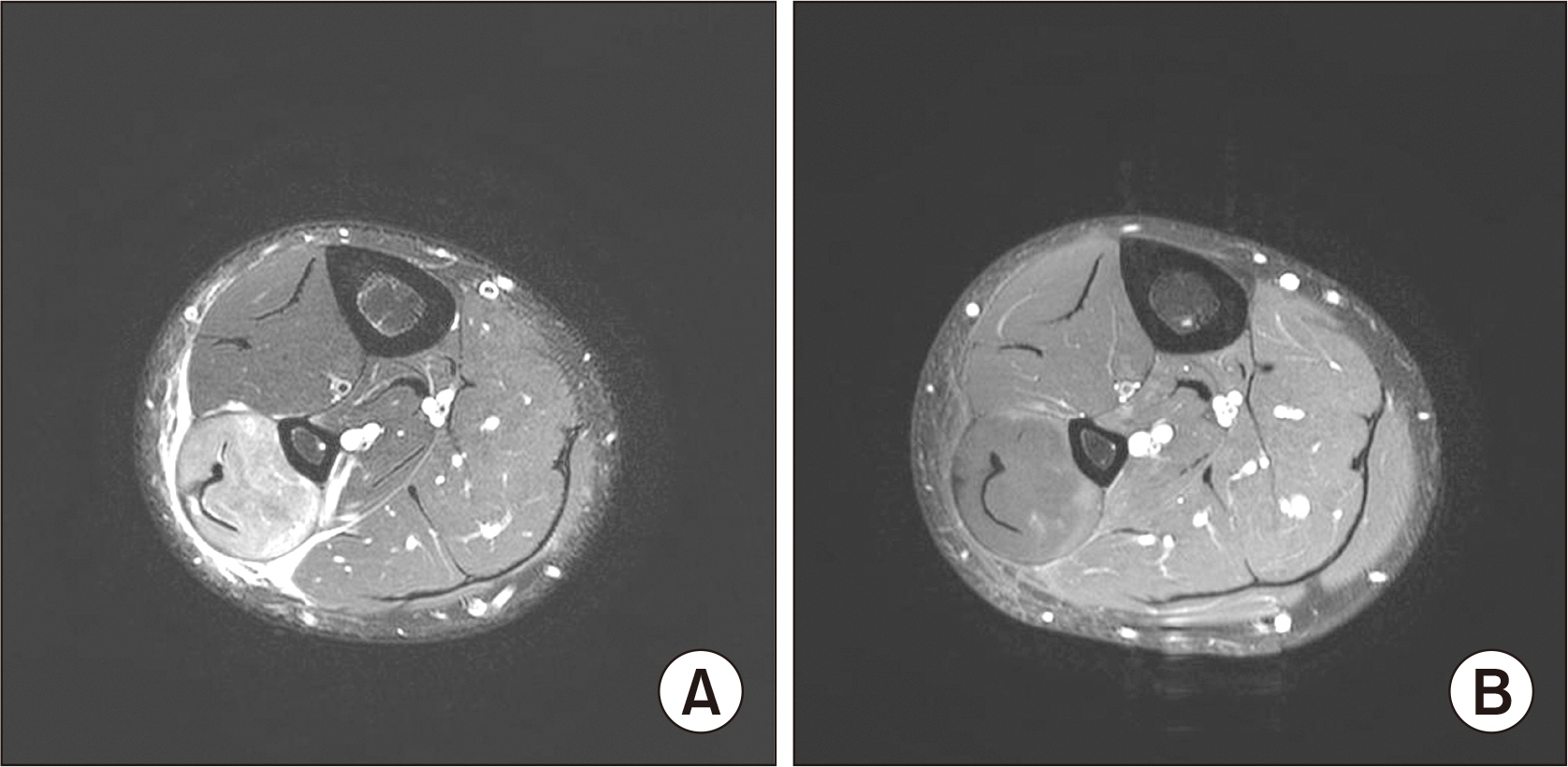
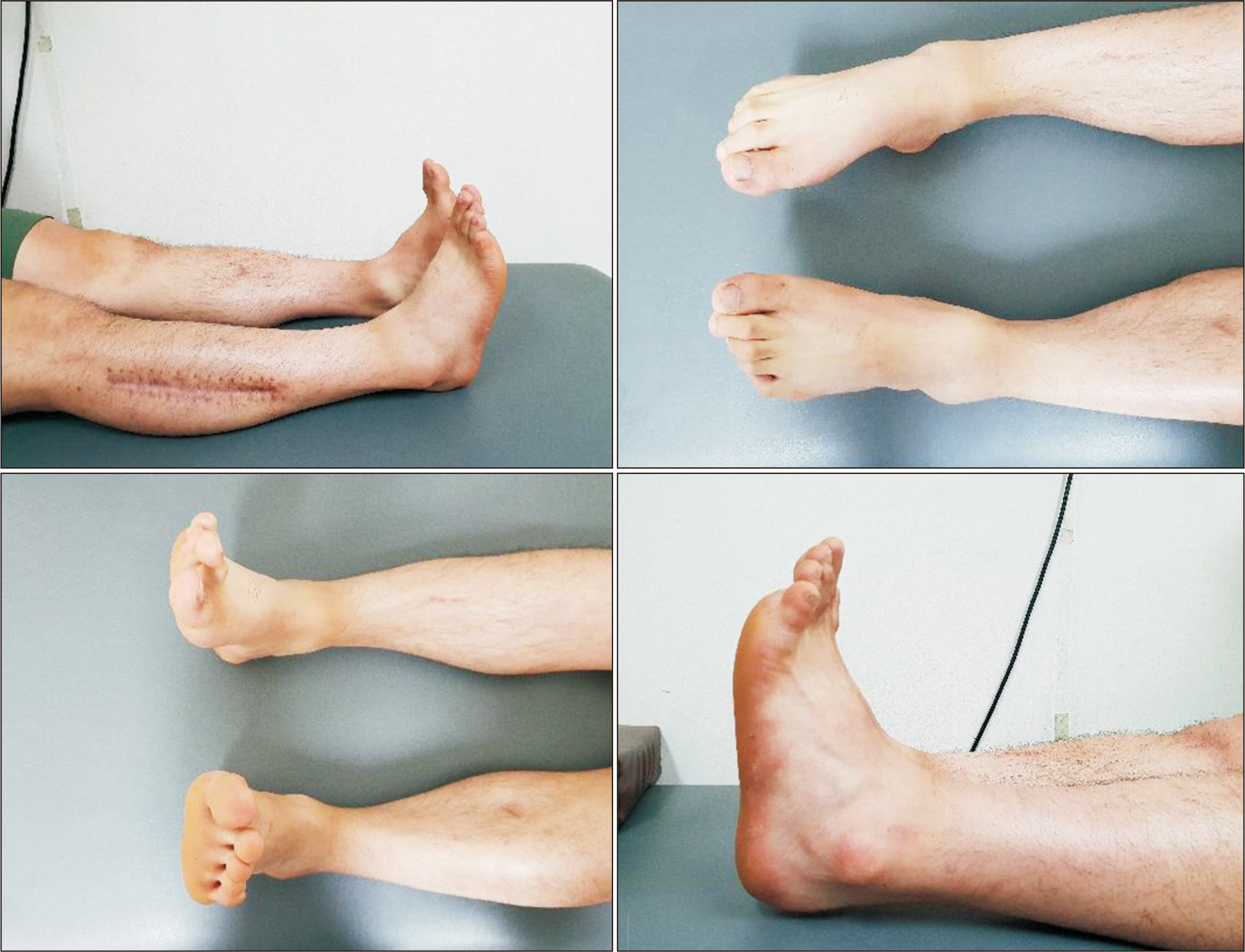
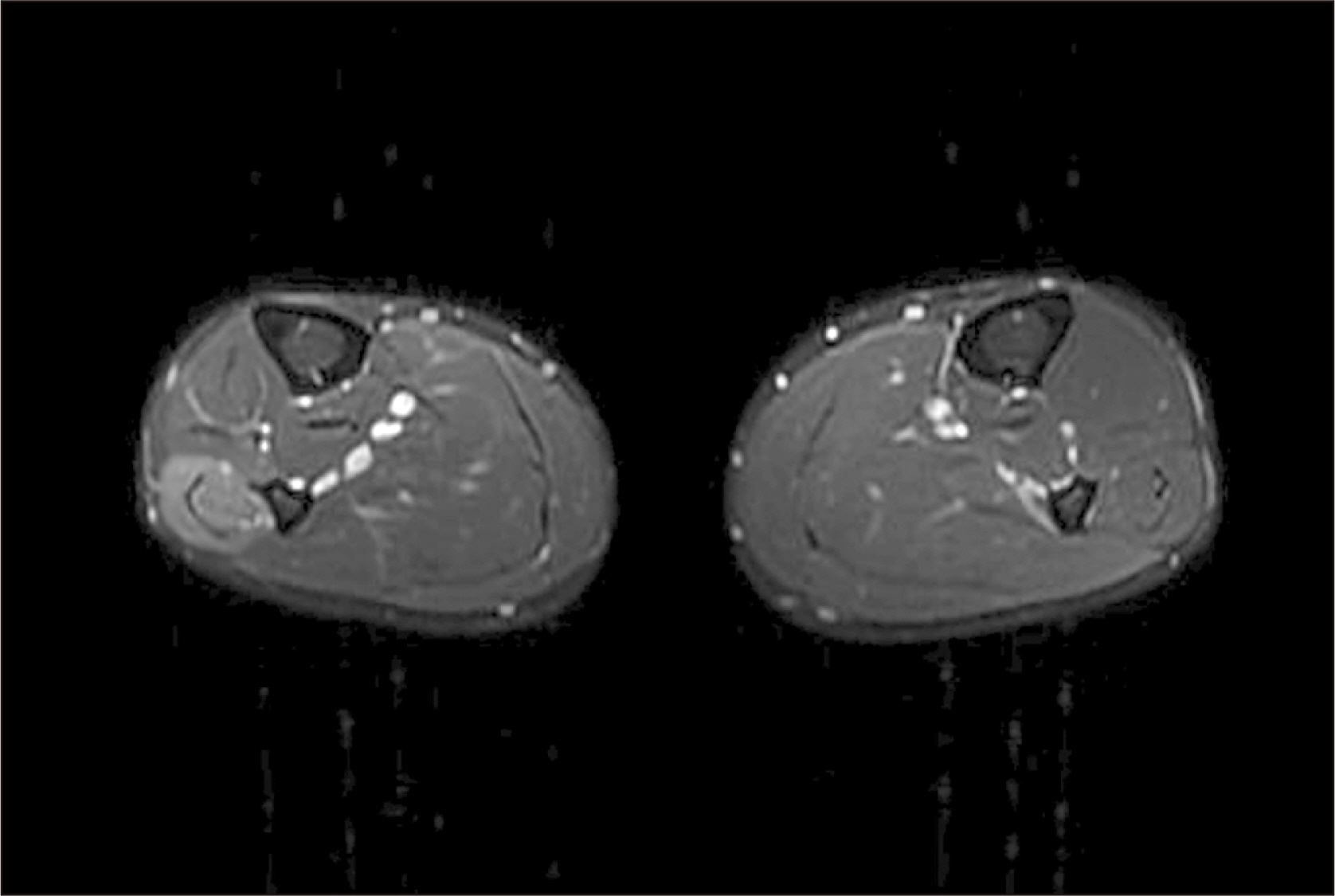
- Lateral compartment syndrome of the lower leg is rarely observed. Hence, there may be difficulty in diagnosis as its clinical patterns are different and more complicated than usual. We report two rare cases of a 20-year-old and a 28-year-old diagnosed with isolated lateral compartment syndrome who had either a surgical or conservative treatment. The comparison was done by analyzing the progression of neurological manifestation, electromyography, and nerve conduction study for two years. In the final follow-up, the patient who underwent the surgical treatment showed a shorter recovery time. However, both patients showed a full recovery from neurologic deficits.
Keyword
Figure
Reference
-
1. Mubarak SJ, Hargens AR, Owen CA, Garetto LP, Akeson WH. 1976; The wick catheter technique for measurement of intramuscular pressure. A new research and clinical tool. J Bone Joint Surg Am. 58:1016–20. DOI: 10.2106/00004623-197658070-00022. PMID: 977611.
Article2. Whitesides TE, Heckman MM. 1996; Acute compartment syndrome: update on diagnosis and treatment. J Am Acad Orthop Surg. 4:209–18. doi: 10.5435/00124635-199607000-00005. DOI: 10.5435/00124635-199607000-00005. PMID: 10795056.
Article3. Gabisan GG, Gentile DR. 2004; Acute peroneal compartment syndrome following ankle inversion injury: a case report. Am J Sports Med. 32:1059–61. doi: 10.1177/0363546503261726. DOI: 10.1177/0363546503261726. PMID: 15150059.4. Ebenezer S, Dust W. 2002; Missed acute isolated peroneal compartment syndrome. CJEM. 4:355–8. doi: 10.1017/S1481803500007776. DOI: 10.1017/S1481803500007776. PMID: 17608982.
Article5. Nicholson P, Devitt A, Stevens M, Mahalingum K. 1998; Acute exertional peroneal compartmental syndrome following prolonged horse riding. Injury. 29:643–4. doi: 10.1016/S0020-1383(98)00143-0. DOI: 10.1016/S0020-1383(98)00143-0.
Article6. Lee RY, Colville JM, Schuberth JM. 2009; Acute compartment syndrome of the leg with avulsion of the peroneus longus muscle: a case report. J Foot Ankle Surg. 48:365–7. doi: 10.1053/j.jfas.2009.01.009. DOI: 10.1053/j.jfas.2009.01.009. PMID: 19423039.
Article7. Naidu KS, Chin T, Harris C, Talbot S. 2009; Bilateral peroneal compartment syndrome after horse riding. Am J Emerg Med. 27:901.e3–5. doi: 10.1016/j.ajem.2008.11.009. DOI: 10.1016/j.ajem.2008.11.009. PMID: 19683135.
Article8. Davies JA. 1979; Peroneal compartment syndrome secondary to rupture of the peroneus longus. A case report. J Bone Joint Surg Am. 61:783–4. DOI: 10.2106/00004623-197961050-00027.
Article9. Gloobe H, Chain D. 1973; Fibular fibrous arch. Anatomical considerations in fibular tunnel syndrome. Acta Anat (Basel). 85:84–7. doi: 10.1159/000143983. DOI: 10.1159/000143983. PMID: 4713100.10. Ryan W, Mahony N, Delaney M, O'Brien M, Murray P. 2003; Relationship of the common peroneal nerve and its branches to the head and neck of the fibula. Clin Anat. 16:501–5. doi: 10.1002/ca.10155. DOI: 10.1002/ca.10155. PMID: 14566896.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Acute Isolated Lateral Compartment Syndrome of a Lower Leg: A Magnetic Resonance Imaging Case Report
- Acute Compartment Syndrome of the Lower Leg and Foot
- Acute Compartment Syndrome after Non-Contact Peroneus Longus Muscle Rupture
- Anterior Compartment Syndrome after Surgery of Bosworth Fracture-Dislocation of the Ankle: A Case Report
- Thenar Compartment syndrome: A Case Report