J Korean Neurosurg Soc.
2022 Sep;65(5):652-664. 10.3340/jkns.2022.0002.
The Kernohan-Woltman Notch Phenomenon : A Systematic Review of Clinical and Radiologic Presentation, Surgical Management, and Functional Prognosis
- Affiliations
-
- 1Department of Neurosurgery, Sainte-Anne Military Teaching Hospital, Toulon, France
- 2Ecole du Val-de-Grâce, French Military Health Service Academy, Paris, France
- 3Intensive Care Unit, Sainte-Anne Military Teaching Hospital, Toulon, France
- 4Department of Neurosurgery, North University Hospital, Aix-Marseille University, Marseille, France
- 5Department of Radiology, North University Hospital, Marseille, France
- 6Val-de-Grâce Military Academy, Paris, France
- KMID: 2533028
- DOI: http://doi.org/10.3340/jkns.2022.0002
Abstract
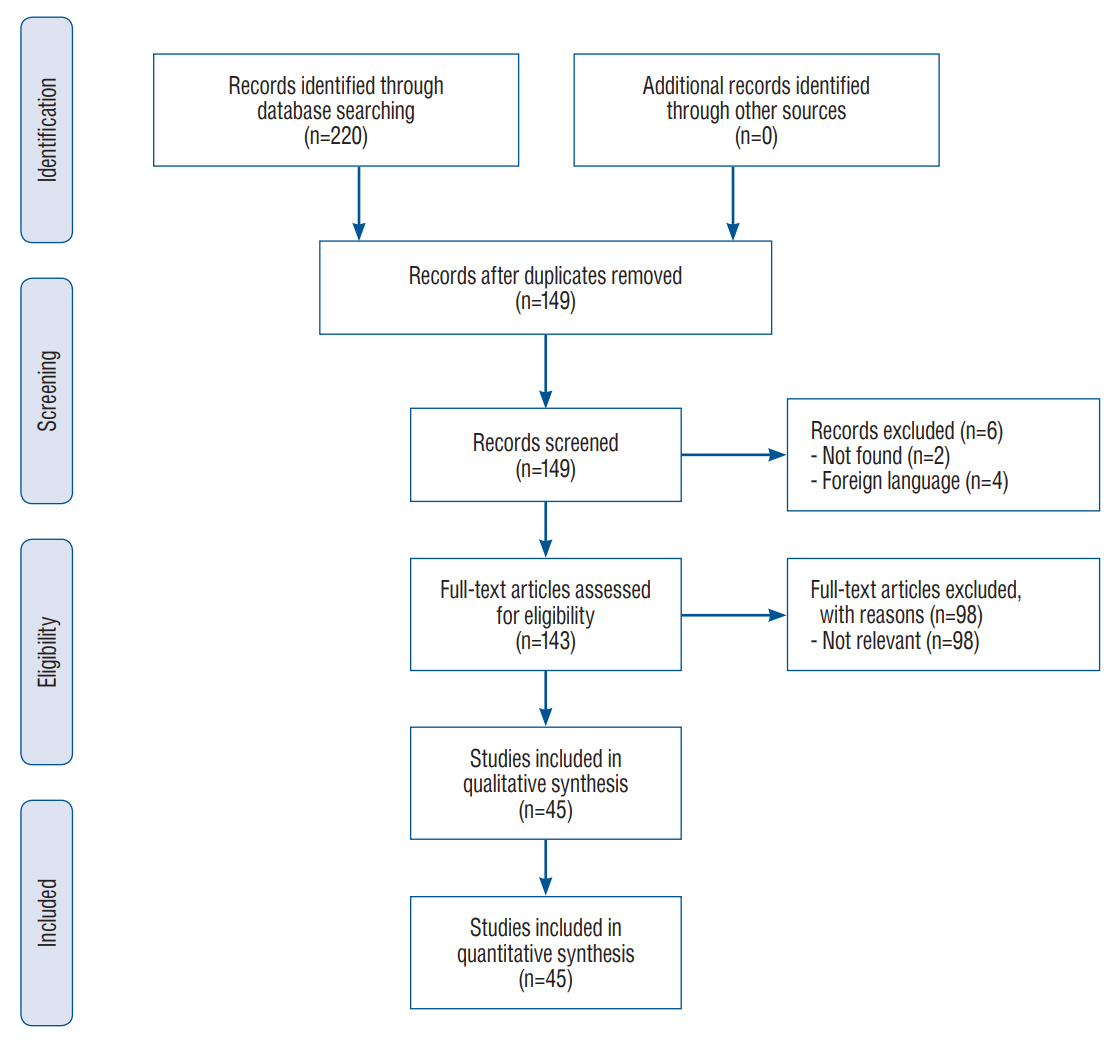
- The Kernohan-Woltman notch phenomenon (KWNP) refers to an intracranial lesion causing massive side-to-side mass effect which leads to compression of the contralateral cerebral peduncle against the free edge of the cerebellar tentorium. Diagnosis is based on “paradoxical” motor deficit ipsilateral to the lesion associated with radiologic evidence of damage to the contralateral cerebral peduncle. To date, there is scarce evidence regarding KWNP associated neuroimaging patterns and motor function prognostic factors. A systematic review was conducted on Medline database from inception to July 2021 looking for English-language articles concerning KWNP, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The research yielded 45 articles for a total of 51 patients. The mean age was 40.7 years-old and the male/female sex ratio was 2/1. 63% of the patients (32/51) suffered from head trauma with a majority of acute subdural hematomas (57%, 29/51). 57% (29/51) of the patients were in the coma upon admission and 47% (24/51) presented pupil anomalies. KWNP presented the neuroimaging features of compression ischemic stroke located in the contralateral cerebral peduncle, with edema in the surrounding structures and sometimes compression stroke of the cerebral arteries passing nearby. 45% of the patients (23/51) presented a good motor functional outcome; nevertheless, no predisposing factor was identified. A Glasgow coma scale (GCS) of more than 3 showed a trend (p=0.1065) toward a better motor functional outcome. The KWNP is a regional compression syndrome oftentimes caused by sudden and massive uncal herniation and leading to contralateral cerebral peduncle ischemia. Even though patients suffering from KWNP usually present a good overall recovery, patients with a GCS of 3 may present a worse motor functional outcome. In order to better understand this syndrome, future studies will have to focus on more personalized criteria such as individual variation of tentorial notch width.
Keyword
Figure
Reference
-
References
1. Adler DE, Milhorat TH. The tentorial notch: anatomical variation, morphometric analysis, and classification in 100 human autopsy cases. J Neurosurg. 96:1103–1112. 2002.2. Binder DK, Lyon R, Manley GT. Transcranial motor evoked potential recording in a case of Kernohan’s notch syndrome: case report. Neurosurgery. 54:999–1002. 2004.3. Çabalar M, Başkan F, Erdoğan HA, Bulut A, Yayla V. Kernohan-Woltman notch phenomenon secondary to a subdural hematoma in a young man. Clin Neuroradiol. 25:435–436. 2015.4. Carlstrom LP, Perry A, Puffer RC, Graffeo CS, Reuter PJ, Fogelson JL, et al. A puzzling exam: Kernohan’s notch reimaged. J Clin Neurosci. 80:336–337. 2020.5. Carrasco R, Pascual JM, Navas M, Martínez-Flórez P, Manzanares-Soler R, Sola RG. Kernohan-Woltman notch phenomenon caused by an acute subdural hematoma. J Clin Neurosci. 16:1628–1631. 2009.6. Carrasco-Moro R, Abreu-Calderón F, de Blas-Beorlegui G, Pascual JM, Ley-Urzaiz L. Kernohan-Woltman notch phenomenon. Rev Clin Esp (Barc). 214:e97–e99. 2014.7. Chang GY. Contusional Kernohan notch phenomenon. Neurol Clin Pract. 6:553–554. 2016.8. Clement VL, Sherer M. Neuropsychological findings in a patient with Kernohan’s notch. Appl Neuropsychol. 3:55–57. 1996.9. Codd PJ, Agarwalla PK, Berry-Candelario J, Nahed BV. Kernohan-Woltman notch phenomenon in acute subdural hematoma. JAMA Neurol. 70:1194–1195. 2013.10. Cohen AR, Wilson J. Magnetic resonance imaging of Kernohan’s notch. Neurosurgery. 27:205–207. 1990.11. Compston A. Aids to the investigation of peripheral nerve injuries. Brain. 133:2838–2844. 2010.12. Corsellis JA. Individual variation in the size of the tentorial opening. J Neurol Neurosurg Psychiatry. 21:279–283. 1958.13. Dibble CF, Wemhoff MP, Ibrahim T, Sasaki-Adams D, Solander S, Germanwala AV. Ruptured arteriovenous malformation presenting with Kernohan’s notch. Case Rep Neurol Med. 2015:921930. 2015.14. Eesa M, Bell K. Kernohan-Woltman notch phenomenon. J Trauma. 69:1634. 2010.15. Evans AH, Gacinovic S, Costa DC, Lees AJ. Parkinsonism due to Kernohan notch: clinical, structural, and functional imaging correlates. Neurology. 62:2333–2334. 2004.16. Evans LR, Jones J, Lee HQ, Gantner D, Jaison A, Matthew J, et al. Prognosis of acute subdural hematoma in the elderly: a systematic review. J Neurotrauma. 36:517–522. 2019.17. Fujimoto A, Sato H, Katayama W, Nakai K, Tsunoda T, Kobayashi E, et al. Kernohan’s phenomenon associated with left ruptured occipital arteriovenous malformation. J Clin Neurosci. 11:444–446. 2004.18. Georgakis MK, Duering M, Wardlaw JM, Dichgans M. WMH and long-term outcomes in ischemic stroke: a systematic review and meta-analysis. Neurology. 92:e1298–e1308. 2019.19. Gimarc K, Massagli TL. Kernohan-Woltman notch phenomenon in two patients with subdural hematoma and ipsilateral hemiparesis. Am J Phys Med Rehabil. 99:1195–1196. 2020.20. Giménez-Pando J, Cabezudo-Artero JM, Fernández-Portales I, Rodríguez-Sánchez JA, Gómez-Perals L, Lorenzana L, et al. Contralateral mesencephalic injury due to tentorial uncal herniation. magnetic resonance imaging of the Kernohan’s notch. Neurocirugia (Astur). 15:384–387. 2004.21. Gobert F, Baars JH, Ritzenthaler T, Afathi M, Boulogne S, André-Obadia N, et al. Diagnosing Kernohan-Woltman notch phenomenon by somatosensory evoked potentials in intensive care unit. Clin Neurophysiol. 129:254–257. 2018.22. Groeneveld A, Schaltenbrand G. Ein fall von duraendotheliom über der großhirnhemisphäre mit einer bemerkenswerten komplikation: läsion des gekrenzten pes pedunculi durch druck auf den rand des tentoriums. Deutsche Zeitschrift f Nervenheilkunde. 97:32–50. 1927.23. Hamada H, Kuwayama N, Endo S, Takaku A. Detection of Kernohan’s notch on magnetic resonance imaging in a patient with acute subdural haematoma. Br J Neurosurg. 14:498–499. 2000.24. Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Czosnyka M, Timothy J, et al. Trial of decompressive craniectomy for traumatic intracranial hypertension. N Engl J Med. 375:1119–1130. 2016.25. Ishizaka S, Shimizu T, Ryu N. Dramatic recovery after severe descending transtentorial herniation-induced duret haemorrhage: a case report and review of literature. Brain Inj. 28:374–377. 2014.26. Itoyama Y, Fujioka S, Ushio Y. Kernohan’s notch in chronic subdural hematoma: findings on magnetic resonance imaging. J Neurosurg. 82:645–646. 1995.27. Iwama T, Kuroda T, Sugimoto S, Miwa Y, Ohkuma A. MRI demonstration of Kernohan’s notch: case report. Neuroradiology. 34:225–226. 1992.28. Jang SG, Pyun SB. Diffusion tensor tractography in two cases of Kernohan-Woltman notch phenomenon. Ann Rehabil Med. 37:879–885. 2013.29. Jang SH, Chang CH, Jung YJ, Seo JP. Locked-in syndrome due to transtentorial herniation and Kernohan notch phenomenon. Am J Phys Med Rehabil. 96:e77. 2017.30. Jones KM, Seeger JF, Yoshino MT. Ipsilateral motor deficit resulting from a subdural hematoma and a Kernohan notch. AJNR Am J Neuroradiol. 12:1238–1239. 1991.31. Kernohan JW, Woltman HW. Incisura of the crus due to contralateral brain tumor. Arch NeurPsych. 21:274–287. 1929.32. Kim JS, Kim J. Pure midbrain infarction: clinical, radiologic, and pathophysiologic findings. Neurology. 64:1227–1232. 2005.33. Kole MK, Hysell SE. MRI correlate of Kernohan’s notch. Neurology. 55:1751. 2000.34. Leever JD. Unilateral cerebral herniation resulting in combined contralateral superior cerebellar artery territory infarction and mesencephalic injury: two cases of a severe unrecognized variant of Kernohan notch phenomenon? Radiol Case Rep. 15:250–253. 2020.35. Lim N, Lee G, Won KH, Kang JS, Lee S, Cho Y, et al. Usefulness of diffusion tensor imaging in unexplained ipsilateral hemiplegia. Korean J Neurotrauma. 17:61–66. 2021.36. Mastronardi L, Puzzilli F, Ruggeri A, Guiducci A. Magnetic resonance imaging findings of Kernohan-Woltman notch in acute subdural hematoma. Clin Neurol Neurosurg. 101:122–124. 1999.37. Mejía Kattah J, Vilá Barriuso E, García Bernedo C, Gallart Gallego L. Kernohan-Woltman notch phenomenon secondary to a cranial epidural hematoma. Rev Esp Anestesiol Reanim. 61:332–335. 2014.38. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:e1000097. 2009.39. Mohseni M, Habibi Z, Nejat F. Contralateral superior cerebellar artery syndrome: a consequence of brain herniation. J Korean Neurosurg Soc. 60:362–366. 2017.40. Moon KS, Lee JK, Joo SP, Kim TS, Jung S, Kim JH, et al. Kernohan’s notch phenomenon in chronic subdural hematoma: MRI findings. J Clin Neurosci. 14:989–992. 2007.41. Namura S, Kang Y, Matsuda I, Kamijyo Y. Magnetic resonance imaging of sequelae of temporal lobe herniation secondary to traumatic acute subdural hematoma: Kernohan’s notch and posterior cerebral artery territory infarctions contralateral to the supratentorial lesion--case report. Neurol Med Chir (Tokyo). 37:32–35. 1997.42. Ono M, Ono M, Rhoton AL Jr, Barry M. Microsurgical anatomy of the region of the tentorial incisura. J Neurosurg. 60:365–399. 1984.43. Openshaw H. Kernohan notch lesion after spinal tap. Neurology. 64:1631. 2005.44. Oster JM, Jones HR Jr, Hildenbrand P, Tronic B, Cosgrove GR. Reversible Kernohan notch. Neurology. 68:368. 2007.45. Ozturk S, Ozturk Y, Ocal O. The first case of Kernohan-Woltman notch phenomenon caused by epidural hematoma in a pediatric patient. Pediatr Neurosurg. 52:181–184. 2017.46. Panikkath R, Panikkath D, Lim SY, Nugent K. Kernohan’s notch: a forgotten cause of hemiplegia-CT scans are useful in this diagnosis. Case Rep Med. 2013:296874. 2013.47. Ritter AM, Muizelaar JP, Barnes T, Choi S, Fatouros P, Ward J, et al. Brain stem blood flow, pupillary response, and outcome in patients with severe head injuries. Neurosurgery. 44:941–948. 1999.48. Samii M, Carvalho GA, Tatagiba M, Matthies C, Vorkapic P. Meningiomas of the tentorial notch: surgical anatomy and management. J Neurosurg. 84:375–381. 1996.49. Schedler P, Geary S. Kernohan’s notch phenomenon: a case study. J Neurosci Nurs. 34:158–159. 2002.50. Simonin A, Levivier M, Nistor S, Diserens K. Kernohan’s notch and misdiagnosis of disorders of consciousness. BMJ Case Rep. 2014:bcr2013202094. 2014.51. Sunderland S. The tentorial notch and complications produced by herniations of the brain through that aperture. Br J Surg. 45:422–438. 1958.52. Ten Harmsen BL, De Kleermaeker FGCM, De Leeuw C, Van Dijk G. Neuro-images Kernohan-Woltman notch phenomenon in acute subdural hematoma. Acta Neurol Belg. 120:189–190. 2020.53. Ueda M, Tsunogae M, Saito H, Suzuki T, Ota T. Delayed hemiparkinsonism associated with Kernohan’s notch in a patient with a ruptured arteriovenous malformation. Intern Med. 60:309–313. 2021.54. Uesugi S, Suehiro E, Nakayama H, Suzuki M. Diffusion-weighted magnetic resonance imaging in a case of Kernohan’s notch phenomenon. Acta Neurochir (Wien). 152:1809–1810. 2010.55. Velasquez JL, Sanz ER, Lasaosa SS, Del Val JL. Kernohan’s notch. Pract Neurol. 15:221. 2015.56. Wijdicks EF. Uncal herniation in acute subdural hematoma: point of no return. Arch Neurol. 59:305. 2002.57. Wijdicks EF. Neurological picture. Acute brainstem displacement without uncal herniation and posterior cerebral artery injury. J Neurol Neurosurg Psychiatry. 79:744. 2008.58. Wijdicks EFM. Through the eyes of monkeys: questions about uncal herniation. Neurocrit Care. 35:573–576. 2021.59. Wolf RF, Ter Weeme CA, Krikke AP. Kernohan’s notch and misdiagnosis. Lancet. 345:259–260. 1995.60. Yogarajah M, Agu CC, Sivasambu B, Mittler MA. HbSC disease and spontaneous epidural hematoma with Kernohan’s notch phenomena. Case Rep Hematol. 2015:470873. 2015.61. Yoo WK, Kim DS, Kwon YH, Jang SH. Kernohan’s notch phenomenon demonstrated by diffusion tensor imaging and transcranial magnetic stimulation. J Neurol Neurosurg Psychiatry. 79:1295–1297. 2008.62. Zafonte RD, Lee CY. Kernohan-Woltman notch phenomenon: an unusual cause of ipsilateral motor deficit. Arch Phys Med Rehabil. 78:543–545. 1997.63. Zhang CH, DeSouza RM, Kho JS, Vundavalli S, Critchley G. KernohanWoltman notch phenomenon: a review article. Br J Neurosurg. 31:159–166. 2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Motor Symptoms in Brain Stem Lesion
- Diffusion Tensor Tractography in Two Cases of Kernohan-Woltman Notch Phenomenon
- Contralateral Superior Cerebellar Artery Syndrome: A Consequence of Brain Herniation
- The Prognostic Factors in the Oligodendrogliomas
- Asymmetric Parkinsonism With Progressive Nigrosomal Change Secondary to Kernohan’s Notch Phenomenon