Clin Exp Otorhinolaryngol.
2022 Aug;15(3):264-272. 10.21053/ceo.2021.02264.
Real-Time Light-Guided Vocal Fold Injection via the Cricothyroid Membrane in Unilateral Vocal Fold Paralysis: A Human Pilot Study
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2532990
- DOI: http://doi.org/10.21053/ceo.2021.02264
Abstract
Objectives
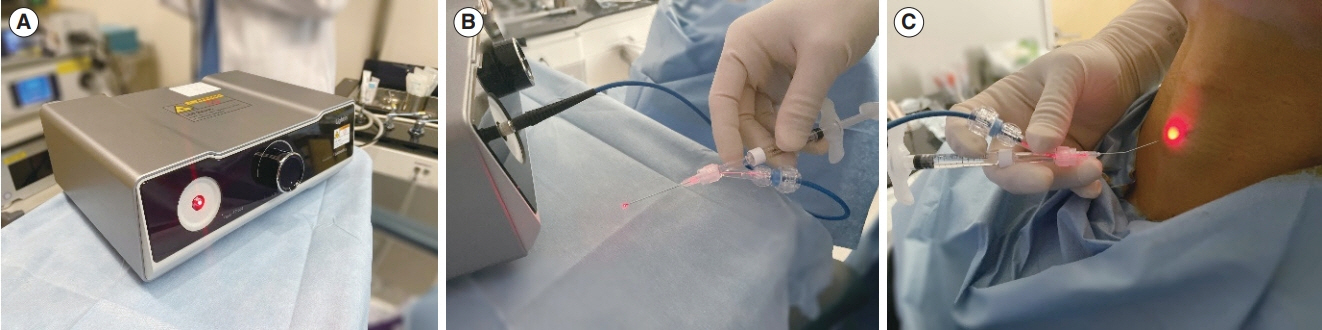
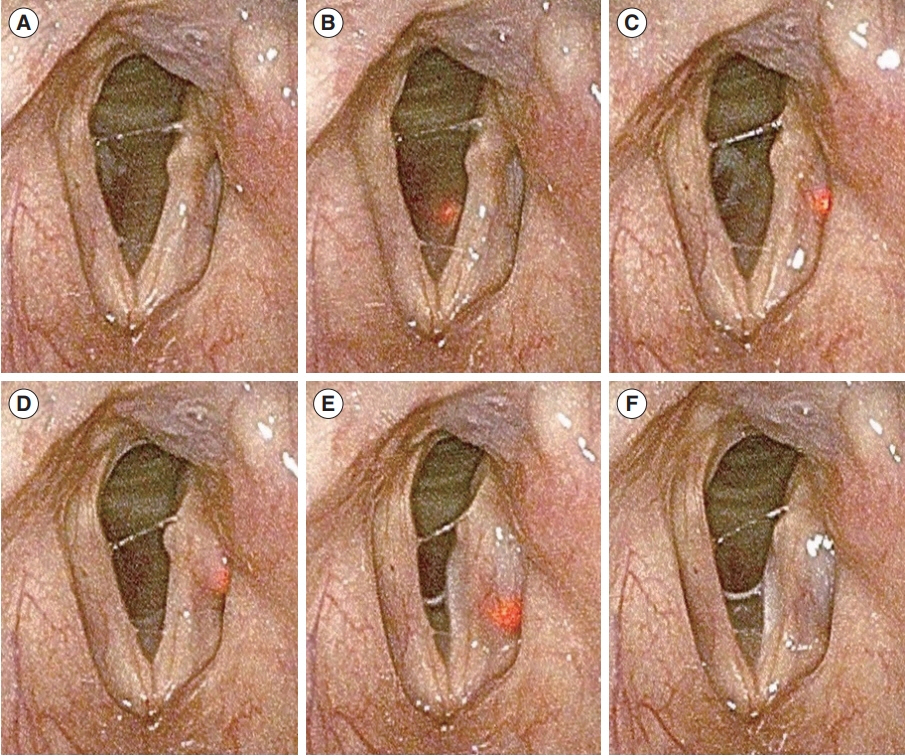
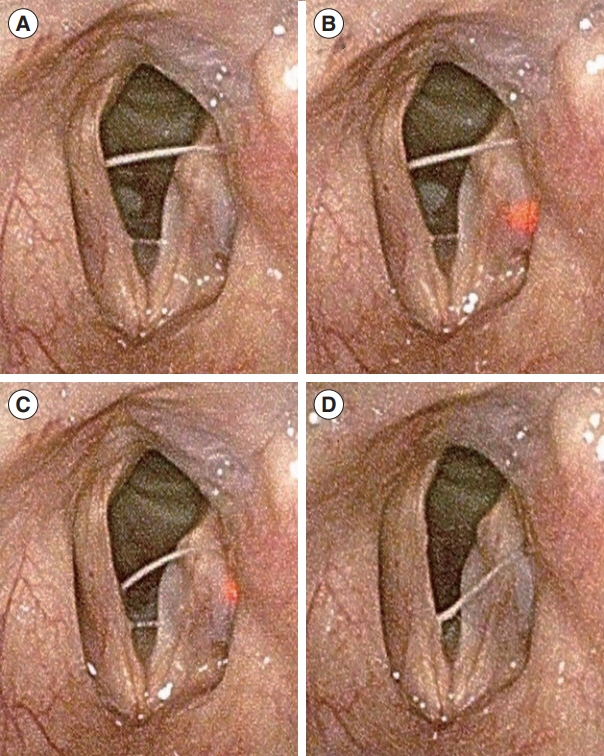
. Vocal fold injection (VFI) via the cricothyroid (CT) membrane is used to treat various diseases affecting the vocal folds. The technical challenges of this technique are mainly related to the invisibility of the needle. Real-time light-guided VFI (RL-VFI) was recently developed for injection under simultaneous light guidance in the CT approach. Herein, we present the first clinical trial of RL-VFI, in which we investigated the feasibility and safety of this new technique in unilateral vocal fold paralysis (VFP).
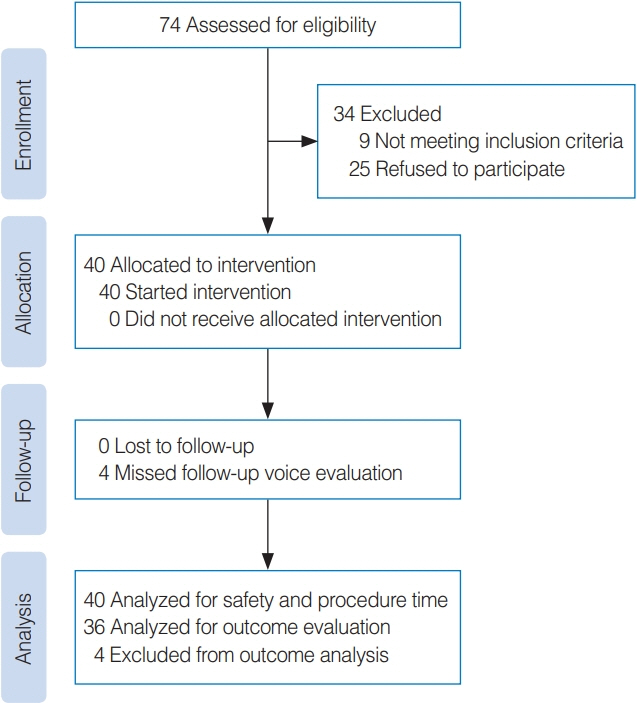
Methods
. This prospective pilot study enrolled 40 patients, who were treated with RL-VFI for unilateral VFP between September 2020 and August 2021. Adverse events were monitored during the procedure and for 4 weeks postoperatively. The Voice Handicap Index-10, the GRBAS (grade, roughness, breathiness, asthenia, and strain) scale, aerodynamic studies, and acoustic analyses were evaluated to compare the voice improvement after 4 weeks with the baseline values.
Results
. The needle tip was intuitively identified by the red light. The mean procedure time was 95.6±40.6 seconds for the initial injection, while the additional injection required 79.2±70.5 seconds. The injection was performed under light guidance without additional manipulation after the needle reached the intended point. No acute or delayed adverse events were reported. Among the 40 patients, 36 completed voice analyses after 4 weeks. Subjective and objective voice parameters, including the Voice Handicap Index-10, GRBAS scale, maximum phonation time, mean expiratory airflow, fundamental frequency, jitter, shimmer, and noise-to-harmonics ratio improved significantly after RL-VFI (P<0.05), while the expiratory volume was maintained.
Conclusion
. RL-VFI is feasible and safe for treating patients with unilateral VFP. This technique is anticipated to improve the precision and safety of the CT approach in the treatment of unilateral VFP. This study provides a rationale for further structured clinical studies.
Keyword
Figure
Cited by 1 articles
-
Complications of Injection Laryngoplasty
Dong-Hyun Kim, Wonjae Cha
Korean J Otorhinolaryngol-Head Neck Surg. 2024;67(5):263-269. doi: 10.3342/kjorl-hns.2023.01221.
Reference
-
1. Rosow DE. Trends in utilization of vocal fold injection procedures. Otolaryngol Head Neck Surg. 2015; Nov. 153(5):812–4.2. Kwon TK, Buckmire R. Injection laryngoplasty for management of unilateral vocal fold paralysis. Curr Opin Otolaryngol Head Neck Surg. 2004; Dec. 12(6):538–42.3. Mallur PS, Rosen CA. Vocal fold injection: review of indications, techniques, and materials for augmentation. Clin Exp Otorhinolaryngol. 2010; Dec. 3(4):177–82.4. Mortensen M, Woo P. Office steroid injections of the larynx. Laryngoscope. 2006; Oct. 116(10):1735–9.5. Hoffman HT, Dailey SH, Bock JM, Thibeault SL, McCulloch TM. Transillumination for needle localization in the larynx. Laryngoscope. 2015; Oct. 125(10):2341–8.6. Seifert A. Percutaneous paraffin injection to eliminate the effects of unilateral laryngeal paralysis. Z Laryngol Rhinol Otol Ihre Grenzgeb. 1916; 1916:233–5.7. Hirano M. Transcutaneous intrafold injection for vocal fold paralysis. Trans Am Broncho-Esophago Assoc. 1985; 115–7.8. Cha W, Ro JH, Wang SG, Jang JY, Cho JK, Kim GH, et al. Development of a device for real-time light-guided vocal fold injection: a preliminary report. Laryngoscope. 2016; Apr. 126(4):936–40.9. Cha W, Ro JH, Yang SC, Choi CJ, Yang I, Kang H, et al. Real-time light-guided vocal fold injection: ex vivo feasibility study in a canine model. Laryngoscope. 2019; Apr. 129(4):935–42.10. Chheda NN, Rosen CA, Belafsky PC, Simpson CB, Postma GN. Revision laryngeal surgery for the suboptimal injection of calcium hydroxylapatite. Laryngoscope. 2008; Dec. 118(12):2260–3.11. Hirano M, Tanaka S, Tanaka Y, Hibi S. Transcutaneous intrafold injection for unilateral vocal fold paralysis: functional results. Ann Otol Rhinol Laryngol. 1990; Aug. 99(8):598–604.12. Chhetri DK, Jamal N. Percutaneous injection laryngoplasty. Laryngoscope. 2014; Mar. 124(3):742–5.13. Pearson W, Hutchinson CT, Noordzij JP. Accessing the vocal folds by transcutaneous injection. Clin Anat. 2010; Apr. 23(3):270–6.14. Jin SM, Park CY, Lee JK, Ban JH, Lee SH, Lee KC. Transcutaneous injection laryngoplasty through the cricothyroid space in the sitting position: anatomical information and technique. Eur Arch Otorhinolaryngol. 2008; Mar. 265(3):313–9.15. Son HY, Kim S, Mohammad RT, Huh G, Kim H, Jeong WJ, et al. Real-time light-guided vocal fold injection: an in vivo feasibility study in a canine model. Clin Exp Otorhinolaryngol. 2021; Aug. 14(3):338–46.16. Won SJ, Woo SH. Calcium hydroxylapatite pulmonary embolism after percutaneous injection laryngoplasty. Yonsei Med J. 2017; Nov. 58(6):1245–8.17. Woo P. Hyaluronidase injection in the vocal folds for vocal hemorrhage, Reinke edema, and hyaluronic acid overinjection: a novel application in the larynx. J Voice. 2018; Jul. 32(4):492–8.18. Wang CC, Chang MH, Jiang RS, Lai HC, De Virgilio A, Wang CP, et al. Laryngeal electromyography-guided hyaluronic acid vocal fold injection for unilateral vocal fold paralysis: a prospective long-term follow-up outcome report. JAMA Otolaryngol Head Neck Surg. 2015; Mar. 141(3):264–71.19. Carrillo A, Garcia-Del-Salto L, Vaca M. Injection laryngoplasty under ultrasonographic control. Eur Arch Otorhinolaryngol. 2021; Jun. 278(6):2143–6.20. Lee SW, Kim JW, Koh YW, Shim SS, Son YI. Comparative analysis of efficiency of injection laryngoplasty technique for with or without neck treatment patients: a transcartilaginous approach versus the cricothyroid approach. Clin Exp Otorhinolaryngol. 2010; Mar. 3(1):37–41.21. Choi N, Jin H, Kim HJ, Son YI. Early injection laryngoplasty with a long-lasting material in patients with potentially recoverable unilateral vocal fold paralysis. Clin Exp Otorhinolaryngol. 2019; Nov. 12(4):427–32.22. Szkielkowska A, Miaskiewicz B, Remacle M, Krasnodebska P, Skarzynski H. Quality of the voice after injection of hyaluronic acid into the vocal fold. Med Sci Monit. 2013; Apr. 19:276–82.23. Birkent H, Sardesai M, Hu A, Merati AL. Prospective study of voice outcomes and patient tolerance of in-office percutaneous injection laryngoplasty. Laryngoscope. 2013; Jul. 123(7):1759–62.24. Hong YT, Minh PH, Hong KH. Which plosive consonant is more useful for the aerodynamic analysis of pathologic voice. Clin Exp Otorhinolaryngol. 2020; May. 13(2):179–85.25. Tanaka S, Gould WJ. Vocal efficiency and aerodynamic aspects in voice disorders. Ann Otol Rhinol Laryngol. 1985; Jan-Feb. 94(1 Pt 1):29–33.26. Kim J, Seo HS, Na HS, Son HY, Lee DK, Jeong WJ, et al. Real-time light-guided vocal fold injection as a simulation-based training tool. Auris Nasus Larynx. 2021; Feb. 48(1):124–30.27. Wang CC, Wu SH, Tu YK, Lin WJ, Liu SA. Hyaluronic acid injection laryngoplasty for unilateral vocal fold paralysis: a systematic review and meta-analysis. Cells. 2020; Nov. 9(11):2417.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vocal Fold Injection: Review of Indications, Techniques, and Materials for Augmentation
- Technical Review of How to Determine the Exact Location of Needle Tip During Office-Based Injection Augmentation of the Vocal Folds Via Cricothyroid Approach
- Development and Clinical Application of Real-Time Light-Guided Vocal Fold Injection
- The Vertical Level of the Paralyzed Vocal Fold in Unilateral Vocal Fold Paralysis
- Primary Thyroid Lymphoma with Vocal Fold Paralysis