Ann Surg Treat Res.
2022 Sep;103(3):176-182. 10.4174/astr.2022.103.3.176.
Association between microsatellite instability and tumor response to neoadjuvant chemoradiotherapy for rectal cancer
- Affiliations
-
- 1Department of Surgery, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea
- 2Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Pathology, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea
- KMID: 2532930
- DOI: http://doi.org/10.4174/astr.2022.103.3.176
Abstract
- Purpose
The relationship between microsatellite instability (MSI) and tumor response after neoadjuvant chemoradiotherapy (nCRT) in rectal cancer remains unclear. The present study aimed to evaluate the association between MSI and tumor response to nCRT in rectal cancer treatment.
Methods
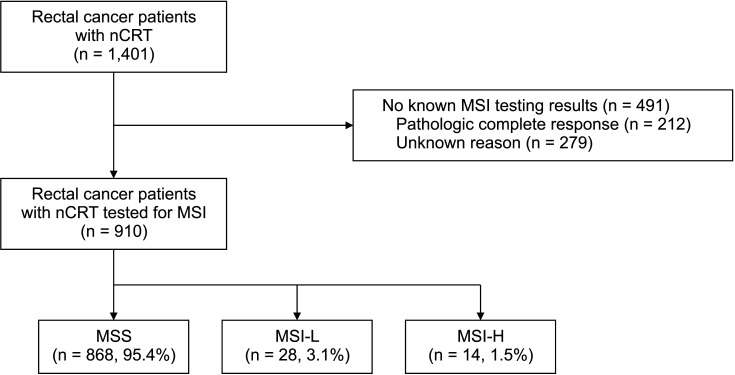
Patients with rectal cancer from 2 tertiary hospitals who underwent nCRT, followed by radical surgery, were included. The microsatellite status was determined using a PCR-based Bethesda panel. Tumors with a Dworak’s tumor regression grade of 3 or 4 were considered to have a good response. Predictive factors for a good response to nCRT were analyzed.
Results
Of the 1,401 patients included, 910 (65.0%) had MSI results and 1.5% (14 of 910) showed MSI-H. Among all the patients, 519 (37.0%) showed a good response to nCRT. A univariate analysis showed that MSI-H tended to be negatively associated with a good response to nCRT, but no statistical significance was observed (7.1% vs. 24.1%, P = 0.208). Multivariate analysis showed that well-differentiated tumors were the only predictive factor for good response to nCRT (odds ratio [OR], 2.241; 95% confidence interval [CI], 1.492–3.364; P < 0.001). MSI status tended to be associated with the response to nCRT (OR, 0.215; 95% CI, 0.027–1.681; P = 0.143).
Conclusion
MSI-H was not associated with response to nCRT in patients with rectal cancer.
Figure
Reference
-
1. National Comprehensive Cancer Network (NCCN). Rectal cancer clinical practice guidelines in oncology [Internet] . Plymouth Meeting, PA: NCCN;2022. cited 2022 Jun 1. Available at: http://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf.2. Pucciarelli S, Gagliardi G, Maretto I, Lonardi S, Friso ML, Urso E, et al. Long-term oncologic results and complications after preoperative chemoradiotherapy for rectal cancer: a single-institution experience after a median follow-up of 95 months. Ann Surg Oncol. 2009; 16:893–899. PMID: 19189187.
Article3. Iv AA, Koprowski MA, Nabavizadeh N, Tsikitis VL. The evolution of rectal cancer treatment: the journey to total neoadjuvant therapy and organ preservation. Ann Gastroenterol. 2022; 35:226–233. PMID: 35599927.4. Perez RO, Julião GP, Vailati BB. Transanal local excision of rectal cancer after neoadjuvant chemoradiation: is there a place for it or should be avoided at all costs? Clin Colon Rectal Surg. 2022; 35:122–128. PMID: 35237107.
Article5. Li M, Xiao Q, Venkatachalam N, Hofheinz RD, Veldwijk MR, Herskind C, et al. Predicting response to neoadjuvant chemoradiotherapy in rectal cancer: from biomarkers to tumor models. Ther Adv Med Oncol. 2022; 14:17588359221077972. PMID: 35222695.
Article6. Ryan JE, Warrier SK, Lynch AC, Ramsay RG, Phillips WA, Heriot AG. Predicting pathological complete response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer: a systematic review. Colorectal Dis. 2016; 18:234–246. PMID: 26531759.
Article7. Lee SY, Kim DW, Lee HS, Ihn MH, Oh HK, Min BS, et al. Low-level microsatellite instability as a potential prognostic factor in sporadic colorectal cancer. Medicine (Baltimore). 2015; 94:e2260. PMID: 26683947.
Article8. O’Connell E, Reynolds IS, McNamara DA, Prehn JH, Burke JP. Microsatellite instability and response to neoadjuvant chemoradiotherapy in rectal cancer: a systematic review and meta-analysis. Surg Oncol. 2020; 34:57–62. PMID: 32891354.
Article9. Dworak O, Keilholz L, Hoffmann A. Pathological features of rectal cancer after preoperative radiochemotherapy. Int J Colorectal Dis. 1997; 12:19–23. PMID: 9112145.
Article10. Rödel C, Martus P, Papadoupolos T, Füzesi L, Klimpfinger M, Fietkau R, et al. Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol. 2005; 23:8688–8696. PMID: 16246976.
Article11. Rizk NP, Venkatraman E, Bains MS, Park B, Flores R, Tang L, et al. American Joint Committee on Cancer staging system does not accurately predict survival in patients receiving multimodality therapy for esophageal adenocarcinoma. J Clin Oncol. 2007; 25:507–512. PMID: 17290058.
Article12. Oh JR, Kim DW, Lee HS, Lee HE, Lee SM, Jang JH, et al. Microsatellite instability testing in Korean patients with colorectal cancer. Fam Cancer. 2012; 11:459–466. PMID: 22669410.
Article13. Umar A, Boland CR, Terdiman JP, Syngal S, de la Chapelle A, Rüschoff J, et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004; 96:261–268. PMID: 14970275.
Article14. Du C, Zhao J, Xue W, Dou F, Gu J. Prognostic value of microsatel lite instability in sporadic locally advanced rectal cancer following neoadjuvant radiotherapy. Histopathology. 2013; 62:723–730. PMID: 23425253.
Article15. Meillan N, Vernerey D, Lefèvre JH, Manceau G, Svrcek M, Augustin J, et al. Mismatch repair system deficiency is associated with response to neoadjuvant chemoradiation in locally advanced rectal cancer. Int J Radiat Oncol Biol Phys. 2019; 105:824–833. PMID: 31404579.
Article16. de Rosa N, Rodriguez-Bigas MA, Chang GJ, Veerapong J, Borras E, Krishnan S, et al. DNA mismatch repair deficiency in rectal cancer: benchmarking its impact on prognosis, neoadjuvant response prediction, and clinical cancer genetics. J Clin Oncol. 2016; 34:3039–3046. PMID: 27432916.
Article17. Huh JW, Kim HC, Kim SH, Park YA, Cho YB, Yun SH, et al. Mismatch repair gene expression as a predictor of tumor responses in patients with rectal cancer treated with preoperative chemoradiation. Medicine (Baltimore). 2016; 95:e2582. PMID: 26817916.
Article18. Hasan S, Renz P, Wegner RE, Finley G, Raj M, Monga D, et al. Microsatellite instability (MSI) as an independent predictor of pathologic complete response (PCR) in locally advanced rectal cancer: a National Cancer Database (NCDB) analysis. Ann Surg. 2020; 271:716–723. PMID: 30216221.
Article19. Guinney J, Dienstmann R, Wang X, de Reyniès A, Schlicker A, Soneson C, et al. The consensus molecular subtypes of colorectal cancer. Nat Med. 2015; 21:1350–1356. PMID: 26457759.
Article20. Jiang D, Wang X, Wang Y, Philips D, Meng W, Xiong M, et al. Mutation in BRAF and SMAD4 associated with resistance to neoadjuvant chemoradiation therapy in locally advanced rectal cancer. Virchows Arch. 2019; 475:39–47. PMID: 31056731.
Article21. Samowitz WS, Curtin K, Wolff RK, Tripp SR, Caan BJ, Slattery ML. Microsatellite instability and survival in rectal cancer. Cancer Causes Control. 2009; 20:1763–1768. PMID: 19669908.
Article22. Ye SB, Cheng YK, Zhang L, Zou YF, Chen P, Deng YH, et al. Association of mismatch repair status with survival and response to neoadjuvant chemo(radio)therapy in rectal cancer. NPJ Precis Oncol. 2020; 4:26. PMID: 32964128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical characteristics of rectal cancer patients with neoadjuvant chemoradiotherapy: a nationwide population-based cohort study in South Korea
- Correlation between tumor regression grade and rectal volume in neoadjuvant concurrent chemoradiotherapy for rectal cancer
- Interpretation of Rectal MRI after Neoadjuvant Treatment in Patients with Rectal Cancer
- Long-term oncologic outcomes in pathologic tumor response after neoadjuvant chemoradiation for locally advanced rectal cancer
- Clinical Implication of Lateral Pelvic Lymph Node Metastasis in Rectal Cancer Treated with Neoadjuvant Chemoradiotherapy