Endocrinol Metab.
2022 Aug;37(4):608-616. 10.3803/EnM.2022.1546.
Advances in Pituitary Surgery
- Affiliations
-
- 1Pituitary Center, Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2532860
- DOI: http://doi.org/10.3803/EnM.2022.1546
Abstract
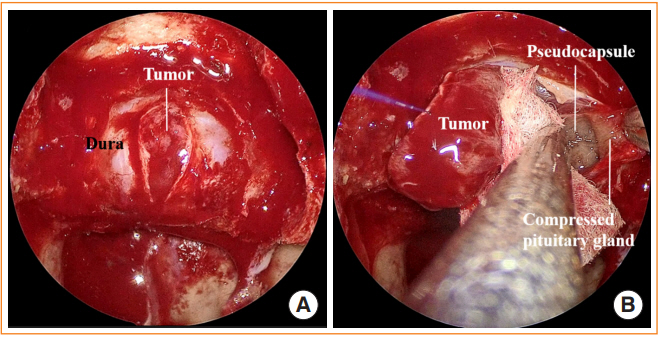
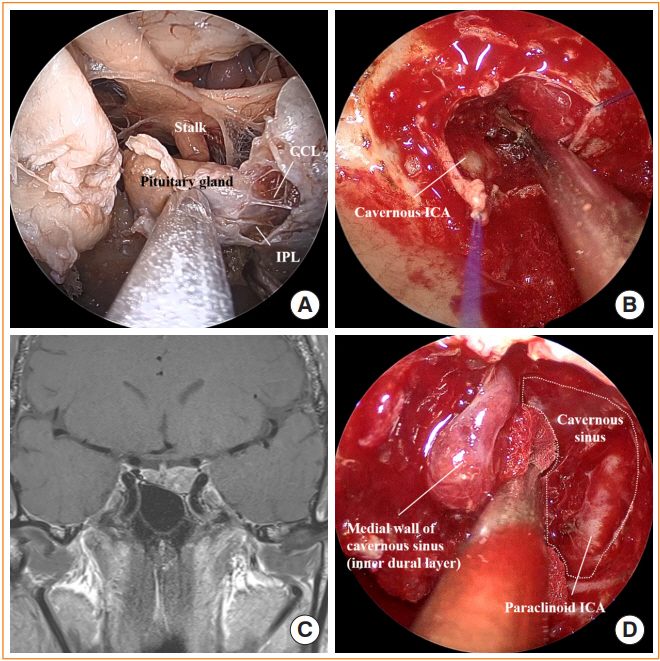
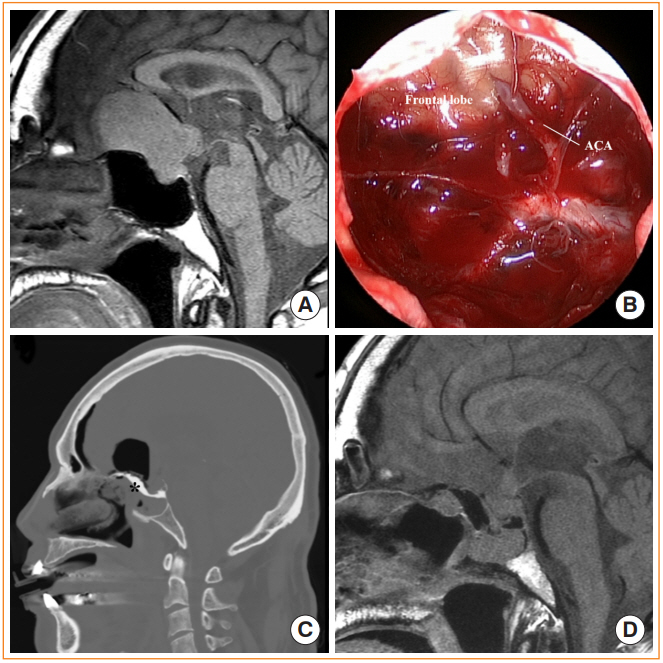
- Pituitary surgery has advanced considerably in recent years with the exploration and development of various endoscopic approaches and techniques. Different endoscopic skull base approaches are being applied to access sellar tumors in different locations. Moreover, extracapsular dissection and cavernous sinus exploration have enabled gross total resection of sellar tumors where it could not have been achieved in the past. Techniques for skull base reconstruction have also progressed, allowing surgeons to remove larger and more complicated tumors than before. This review article discusses different endoscopic skull base approaches, surgical techniques for removing pituitary adenomas, and reconstruction methods for repairing postoperative low-flow and high-flow cerebrospinal fluid leakage.
Figure
Cited by 1 articles
-
Obstructive Sleep Apnea Screening and Effects of Surgery in Acromegaly: A Prospective Study
Jaeyoung Cho, Jung Hee Kim, Yong Hwy Kim, Jinwoo Lee
Endocrinol Metab. 2024;39(4):641-652. doi: 10.3803/EnM.2024.1933.
Reference
-
1. Chanson P, Raverot G, Castinetti F, Cortet-Rudelli C, Galland F, Salenave S, et al. Management of clinically non-functioning pituitary adenoma. Ann Endocrinol (Paris). 2015; 76:239–47.
Article2. Molitch ME. Diagnosis and treatment of pituitary adenomas: a review. JAMA. 2017; 317:516–24.3. Jho HD. Endoscopic transsphenoidal surgery. J Neurooncol. 2001; 54:187–95.4. Frank G, Pasquini E, Farneti G, Mazzatenta D, Sciarretta V, Grasso V, et al. The endoscopic versus the traditional approach in pituitary surgery. Neuroendocrinology. 2006; 83:240–8.
Article5. Taniguchi M, Hosoda K, Akutsu N, Takahashi Y, Kohmura E. Endoscopic endonasal transsellar approach for laterally extended pituitary adenomas: volumetric analysis of cavernous sinus invasion. Pituitary. 2015; 18:518–24.
Article6. Qu X, Xu G, Qu Y, Song T. The pseudocapsule surrounding a pituitary adenoma and its clinical significance. J Neurooncol. 2011; 101:171–8.
Article7. Chamoun R, Takashima M, Yoshor D. Endoscopic extracapsular dissection for resection of pituitary macroadenomas: technical note. J Neurol Surg A Cent Eur Neurosurg. 2014; 75:48–52.
Article8. Oldfield EH, Vortmeyer AO. Development of a histological pseudocapsule and its use as a surgical capsule in the excision of pituitary tumors. J Neurosurg. 2006; 104:7–19.
Article9. Kinoshita Y, Tominaga A, Usui S, Arita K, Sakoguchi T, Sugiyama K, et al. The surgical side effects of pseudocapsular resection in nonfunctioning pituitary adenomas. World Neurosurg. 2016; 93:430–5.e1.
Article10. Jagannathan J, Smith R, DeVroom HL, Vortmeyer AO, Stratakis CA, Nieman LK, et al. Outcome of using the histological pseudocapsule as a surgical capsule in Cushing disease. J Neurosurg. 2009; 111:531–9.
Article11. Taylor DG, Jane JA, Oldfield EH. Resection of pituitary macroadenomas via the pseudocapsule along the posterior tumor margin: a cohort study and technical note. J Neurosurg. 2018; 128:422–8.
Article12. Zhang X, Wang YG, Tan J, Zhao G, Ma M, Chen J, et al. Comparison of outcomes between intracapsular resection and pseudocapsule-based extracapsular resection for pituitary adenoma: a systematic review and meta-analysis. BMC Neurol. 2022; 22:52.
Article13. Omar AT, Munoz DG, Goguen J, Lee JM, Rotondo F, Kovacs K, et al. Resection of the medial wall of the cavernous sinus in functioning pituitary adenomas: technical note and outcomes in a matched-cohort study. Clin Neurol Neurosurg. 2020; 106306.
Article14. Kim JH, Lee JH, Lee JH, Hong AR, Kim YJ, Kim YH. Endoscopic transsphenoidal surgery outcomes in 331 nonfunctioning pituitary adenoma cases after a single surgeon learning curve. World Neurosurg. 2018; 109:e409–16.
Article15. Dhandapani S, Singh H, Negm HM, Cohen S, Anand VK, Schwartz TH. Cavernous sinus invasion in pituitary adenomas: systematic review and pooled data meta-analysis of radiologic criteria and comparison of endoscopic and microscopic surgery. World Neurosurg. 2016; 96:36–46.
Article16. Rhoton AL Jr. The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery. 2002; 51(4 Suppl):S375–410.
Article17. Rutkowski M, Zada G. Management of pituitary adenomas invading the cavernous sinus. Neurosurg Clin N Am. 2019; 30:445–55.
Article18. Ferreli F, Turri-Zanoni M, Canevari FR, Battaglia P, Bignami M, Castelnuovo P, et al. Endoscopic endonasal management of non-functioning pituitary adenomas with cavernous sinus invasion: a 10-year experience. Rhinology. 2015; 53:308–16.19. Cohen-Cohen S, Gardner PA, Alves-Belo JT, Truong HQ, Snyderman CH, Wang EW, et al. The medial wall of the cavernous sinus. Part 2: Selective medial wall resection in 50 pituitary adenoma patients. J Neurosurg. 2018; 131:131–40.
Article20. Nishioka H, Fukuhara N, Horiguchi K, Yamada S. Aggressive transsphenoidal resection of tumors invading the cavernous sinus in patients with acromegaly: predictive factors, strategies, and outcomes. J Neurosurg. 2014; 121:505–10.
Article21. Juraschka K, Khan OH, Godoy BL, Monsalves E, Kilian A, Krischek B, et al. Endoscopic endonasal transsphenoidal approach to large and giant pituitary adenomas: institutional experience and predictors of extent of resection. J Neurosurg. 2014; 121:75–83.
Article22. Park HH, Kim EH, Ku CR, Lee EJ, Kim SH. Outcomes of aggressive surgical resection in growth hormone-secreting pituitary adenomas with cavernous sinus invasion. World Neurosurg. 2018; 117:e280–9.
Article23. Truong HQ, Lieber S, Najera E, Alves-Belo JT, Gardner PA, Fernandez-Miranda JC. The medial wall of the cavernous sinus. Part 1: Surgical anatomy, ligaments, and surgical technique for its mobilization and/or resection. J Neurosurg. 2018; 131:122–30.
Article24. Nagata Y, Takeuchi K, Yamamoto T, Ishikawa T, Kawabata T, Shimoyama Y, et al. Removal of the medial wall of the cavernous sinus for functional pituitary adenomas: a technical report and pathologic significance. World Neurosurg. 2019; 126:53–8.
Article25. Xu Y, Nunez MA, Mohyeldin A, Vigo V, Mao Y, Cohen-Gadol AA, et al. Microsurgical anatomy of the dorsal clinoidal space: implications for endoscopic endonasal parasellar surgery. J Neurosurg. 2022; Feb. 4. [Epub]. https://doi.org/10.3171/2021.12.JNS211974.
Article26. Yasargil MG, Abdulrauf SI. Surgery of intraventricular tumors. Neurosurgery. 2008; 62(6 Suppl 3):1029–40.
Article27. Dho YS, Kim YH, Se YB, Han DH, Kim JH, Park CK, et al. Endoscopic endonasal approach for craniopharyngioma: the importance of the relationship between pituitary stalk and tumor. J Neurosurg. 2018; 129:611–9.
Article28. Cavallo LM, Di Somma A, de Notaris M, Prats-Galino A, Aydin S, Catapano G, et al. Extended endoscopic endonasal approach to the third ventricle: multimodal anatomical study with surgical implications. World Neurosurg. 2015; 84:267–78.
Article29. Cavallo LM, Prevedello DM, Solari D, Gardner PA, Esposito F, Snyderman CH, et al. Extended endoscopic endonasal transsphenoidal approach for residual or recurrent craniopharyngiomas. J Neurosurg. 2009; 111:578–89.
Article30. Phi JH, Kim YH, Kim JH, Kim DG. Clinical and anatomic features of supraglandular pituitary adenomas. World Neurosurg. 2016; 92:241–8.
Article31. Seo Y, Kim YH, Kim JH, Kong DS, Dho YS, Kang H, et al. Outcomes of the endoscopic endonasal approach for tumors in the third ventricle or invading the third ventricle. J Clin Neurosci. 2021; 90:302–10.
Article32. de Divitiis E, Cavallo LM, Cappabianca P, Esposito F. Extended endoscopic endonasal transsphenoidal approach for the removal of suprasellar tumors: Part 2. Neurosurgery. 2007; 60:46–58.33. Barazi SA, Pasquini E, D’Urso PI, Zoli M, Mazzatenta D, Sciarretta V, et al. Extended endoscopic transplanum-transtuberculum approach for pituitary adenomas. Br J Neurosurg. 2013; 27:374–82.
Article34. Fomichev D, Kalinin P, Kutin M, Sharipov O. Extended transsphenoidal endoscopic endonasal surgery of suprasellar craniopharyngiomas. World Neurosurg. 2016; 94:181–7.
Article35. Kim YH, Jeon C, Se YB, Hong SD, Seol HJ, Lee JI, et al. Clinical outcomes of an endoscopic transclival and transpetrosal approach for primary skull base malignancies involving the clivus. J Neurosurg. 2018; 128:1454–62.
Article36. Karadag A, Senoglu M, Middlebrooks EH, Kinali B, Guvencer M, Icke C, et al. Endoscopic endonasal transclival approach to the ventral brainstem: radiologic, anatomic feasibility and nuances, surgical limitations and future directions. J Clin Neurosci. 2020; 73:264–79.
Article37. Essayed WI, Singh H, Lapadula G, Almodovar-Mercado GJ, Anand VK, Schwartz TH. Endoscopic endonasal approach to the ventral brainstem: anatomical feasibility and surgical limitations. J Neurosurg. 2017; 127:1139–46.
Article38. Fortes FS, Sennes LU, Carrau RL, Brito R, Ribas GC, Yasuda A, et al. Endoscopic anatomy of the pterygopalatine fossa and the transpterygoid approach: development of a surgical instruction model. Laryngoscope. 2008; 118:44–9.
Article39. Karci B, Midilli R, Erdogan U, Turhal G, Gode S. Endoscopic endonasal approach to the Vidian nerve and its relation to the surrounding structures: an anatomic cadaver study. Eur Arch Otorhinolaryngol. 2018; 275:2473–9.
Article40. DelGaudio JM. Endoscopic transnasal approach to the pterygopalatine fossa. Arch Otolaryngol Head Neck Surg. 2003; 129:441–6.
Article41. Hofstetter CP, Singh A, Anand VK, Kacker A, Schwartz TH. The endoscopic, endonasal, transmaxillary transpterygoid approach to the pterygopalatine fossa, infratemporal fossa, petrous apex, and the Meckel cave. J Neurosurg. 2010; 113:967–74.
Article42. Luginbuhl AJ, Campbell PG, Evans J, Rosen M. Endoscopic repair of high-flow cranial base defects using a bilayer button. Laryngoscope. 2010; 120:876–80.
Article43. Keshri A, Jain R, Manogaran RS, Behari S, Khatri D, Mathialagan A. Management of spontaneous CSF rhinorrhea: an institutional experience. J Neurol Surg B Skull Base. 2019; 80:493–9.
Article44. Chaskes MB, Fastenberg JH, Vimawala S, Nyquist GF, Rabinowitz MR, Chitguppi C, et al. A simple onlay sellar reconstruction does not increase the risk of postoperative cerebrospinal fluid leak in well-selected patients. J Neurol Surg B Skull Base. 2021; 82(Suppl 3):e231–5.
Article45. Wood J, Densky J, Boughter J, Sebelik M, Shires C. Anterior skull base reconstruction: does fat preparation matter? J Neurol Surg Rep. 2018; 79:e31–5.
Article46. Jeon C, Hong SD, Seol HJ, Lee JI, Nam DH, Hwang YJ, et al. Reconstructive outcome of intraoperative cerebrospinal fluid leak after endoscopic endonasal surgery for tumors involving skull base. J Clin Neurosci. 2017; 45:227–31.
Article47. Conger A, Zhao F, Wang X, Eisenberg A, Griffiths C, Esposito F, et al. Evolution of the graded repair of CSF leaks and skull base defects in endonasal endoscopic tumor surgery: trends in repair failure and meningitis rates in 509 patients. J Neurosurg. 2018; 130:861–75.
Article48. Soudry E, Turner JH, Nayak JV, Hwang PH. Endoscopic reconstruction of surgically created skull base defects: a systematic review. Otolaryngol Head Neck Surg. 2014; 150:730–8.
Article49. Karnezis TT, Baker AB, Soler ZM, Wise SK, Rereddy SK, Patel ZM, et al. Factors impacting cerebrospinal fluid leak rates in endoscopic sellar surgery. Int Forum Allergy Rhinol. 2016; 6:1117–25.
Article50. Harvey RJ, Parmar P, Sacks R, Zanation AM. Endoscopic skull base reconstruction of large dural defects: a systematic review of published evidence. Laryngoscope. 2012; 122:452–9.
Article51. Ahmed OH, Marcus S, Tauber JR, Wang B, Fang Y, Lebowitz RA. Efficacy of perioperative lumbar drainage following endonasal endoscopic cerebrospinal fluid leak repair. Otolaryngol Head Neck Surg. 2017; 156:52–60.
Article52. D’Anza B, Tien D, Stokken JK, Recinos PF, Woodard TR, Sindwani R. Role of lumbar drains in contemporary endonasal skull base surgery: meta-analysis and systematic review. Am J Rhinol Allergy. 2016; 30:430–5.
Article53. Kim YH, Kang H, Dho YS, Hwang K, Joo JD, Kim YH. Multi-layer onlay graft using hydroxyapatite cement placement without cerebrospinal fluid diversion for endoscopic skull base reconstruction. J Korean Neurosurg Soc. 2021; 64:619–30.
Article54. Lee SH, Ha CM, Hong SD, Choi JW, Seol HJ, Nam DH, et al. Clinical impact of hydroxyapatite on the outcome of skull base reconstruction for intraoperative high-flow CSF leak: a propensity score matching analysis. Front Oncol. 2022; 12:906162.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pituitary Apoplexy due to Pituitary Adenoma Infarction
- Surgical Management of Pituitary Tumors
- Two Cases of Pituitary Hyperplasia Secondary to Primary Hypothyroidism Mimicking Pituitary Tumor
- Computed tomography of pituitary apoplexy: report of 2 cases
- Best Achievements in Pituitary and Adrenal Diseases in 2020