J Korean Med Sci.
2022 Aug;37(34):e263. 10.3346/jkms.2022.37.e263.
Serial Long-Term Growth and Neurodevelopment of Very-Low-BirthWeight Infants: 2022 Update on the Korean Neonatal Network
- Affiliations
-
- 1Department of Pediatrics, Inha University Hospital, Inha University College of Medicine, Incheon, Korea
- 2Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea
- 3Department of Pharmacology, Inje University College of Medicine, Busan, Korea
- 4Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences & Technology (SAIHST), Samsung Medical Center, Seoul, Korea
- KMID: 2532757
- DOI: http://doi.org/10.3346/jkms.2022.37.e263
Abstract
- Background
We aimed to evaluate the long-term growth and neurodevelopmental outcomes of very-low-birth-weight infants (VLBWIs, birth weight < 1,500 g) born between 2013, the establishment of the Korean Neonatal Network (KNN), and 2018, both at 18–24 months of corrected age and three years of age, using a nationwide large cohort, and to evaluate whether these outcomes have improved over time since 2013.
Methods
This study used data from the annual reports of the KNN for 18–24 months of corrected age (follow-up 1) and three years of age (follow-up 2). Follow-up 1 data were collected from 10,065 eligible VLBWIs born between January 1, 2013, and December 31, 2018. Follow-up 2 data were collected from 8,156 eligible VLBWIs born between January 1, 2013, and December 31, 2017.
Results
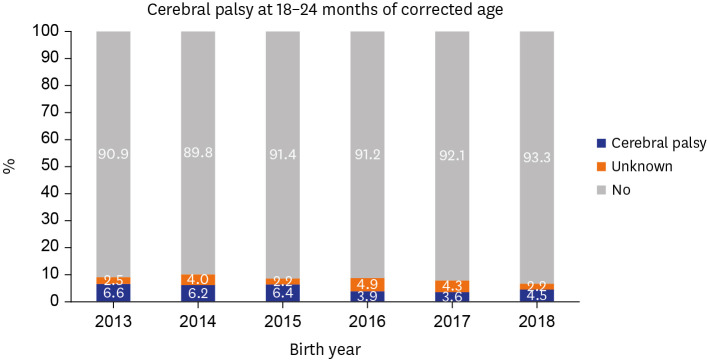
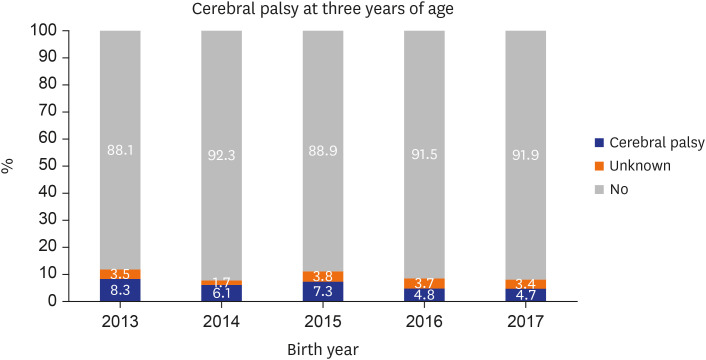
The overall follow-up rates of VLBWIs at follow-ups 1 and 2 were 74.6% (7,512/10,065) and 57.7% (4,702/8,156), respectively. The overall mortality rate between discharge from the neonatal intensive care unit and follow-up 1 was 1% (104/10,065). The overall mortality rate between follow-ups 1 and 2 was 0.049% (4/8,156). Growth restrictions decreased over time, especially weight growth restrictions, which significantly decreased according to era (17% in infants born in 2013–2014 and 13% in infants born in 2017–2018). Fewer infants were rehospitalized and required rehabilitative support according to era at follow-up 1. More infants had language developmental delays and required language support according to era, both at follow-ups 1 and 2. The incidence of cerebral palsy has significantly decreased over time, from 6% in infants born in 2013–2014 to 4% in infants born in 2017–2018 at follow-up 1, and from 8% in infants born in 2013–2014 to 5% in infants born in 2017 at follow-up 2.
Conclusion
Long-term outcomes of VLBWIs regarding weight growth and cerebral palsy, the most common motor disability in childhood, have improved serially according to era since 2013. However, the rate of infants with language delays requiring language support has increased according to era. Further studies are required on the increased trends of language delay and language support while improving motor outcomes.
Keyword
Figure
Cited by 2 articles
-
Fibrinolytic (Thrombolytic) Therapy for Post Intraventricular Hemorrhagic Hydrocephalus in Preterm Infants
Young Soo Park
J Korean Neurosurg Soc. 2023;66(3):263-273. doi: 10.3340/jkns.2022.0258.Antenatal Magnesium Sulfate Is Not Associated With Improved Long-Term Neurodevelopment and Growth in Very Low Birth Weight Infants
Ga Won Jeon, So Yoon Ahn, Su Min Kim, Misun Yang, Se In Sung, Ji-Hee Sung, Soo-young Oh, Cheong-Rae Roh, Suk-Joo Choi, Yun Sil Chang
J Korean Med Sci. 2023;38(44):e350. doi: 10.3346/jkms.2023.38.e350.
Reference
-
1. Fortmann I, Mertens L, Boeckel H, Grüttner B, Humberg A, Astiz M, et al. A timely administration of antenatal steroids is highly protective against intraventricular hemorrhage: an observational multicenter cohort study of very low birth weight infants. Front Pediatr. 2022; 10:721355. PMID: 35372176.
Article2. Jeon GW. Surfactant preparations for preterm infants with respiratory distress syndrome: past, present, and future. Korean J Pediatr. 2019; 62(5):155–161. PMID: 30744318.
Article3. Oskoui M, Joseph L, Dagenais L, Shevell M. Prevalence of cerebral palsy in Quebec: alternative approaches. Neuroepidemiology. 2013; 40(4):264–268. PMID: 23363886.
Article4. Spittle AJ, Morgan C, Olsen JE, Novak I, Cheong JL. Early diagnosis and treatment of cerebral palsy in children with a history of preterm birth. Clin Perinatol. 2018; 45(3):409–420. PMID: 30144846.
Article5. Hafström M, Källén K, Serenius F, Maršál K, Rehn E, Drake H, et al. Cerebral palsy in extremely preterm infants. Pediatrics. 2018; 141(1):e20171433. PMID: 29222398.
Article6. The Executive Committee of Korean Neonatal Network. 2015 Korean Neonatal Network Annual Report. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2016.7. The Executive Committee of Korean Neonatal Network. 2016 Korean Neonatal Network Annual Report. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2017.8. Cristobal R, Oghalai JS. Hearing loss in children with very low birth weight: current review of epidemiology and pathophysiology. Arch Dis Child Fetal Neonatal Ed. 2008; 93(6):F462–F468. PMID: 18941031.
Article9. Prakalapakorn SG, Greenberg L, Edwards EM, Ehret DE. Trends in retinopathy of prematurity screening and treatment: 2008–2018. Pediatrics. 2021; 147(6):e2020039966. PMID: 33975923.
Article10. Horbar JD, Ehrenkranz RA, Badger GJ, Edwards EM, Morrow KA, Soll RF, et al. Weight growth velocity and postnatal growth failure in infants 501 to 1500 grams: 2000–2013. Pediatrics. 2015; 136(1):e84–e92. PMID: 26101360.
Article11. The Executive Committee of Korean Neonatal Network. 2020 Korean Neonatal Network Annual Report. Cheongju, Korea: Korea National Institute of Health;2021.12. The Executive Committee of Korean Neonatal Network. 2017 Korean Neonatal Network Annual Report. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2018.13. The Executive Committee of Korean Neonatal Network. 2018 Korean Neonatal Network Annual Report. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2019.14. The Executive Committee of Korean Neonatal Network. 2019 Korean Neonatal Network Annual Report. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2020.15. Pierrat V, Marchand-Martin L, Marret S, Arnaud C, Benhammou V, Cambonie G, et al. Neurodevelopmental outcomes at age 5 among children born preterm: EPIPAGE-2 cohort study. BMJ. 2021; 373(741):n741. PMID: 33910920.
Article16. Kim CY, Jung E, Lee BS, Kim KS, Kim EA. Validity of the Korean Developmental Screening Test for very-low-birth-weight infants. Korean J Pediatr. 2019; 62(5):187–192. PMID: 30999730.
Article17. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006; 450:76–85. PMID: 16817681.18. The Evidence from NRNJ database for VLBW (2003-2012)-Vol 1-(2021 revision). Updated 2021. Accessed June 9, 2022. https://plaza.umin.ac.jp/nrndata/indexe.htm .19. Kono Y. Neonatal Research Network of Japan. Neurodevelopmental outcomes of very low birth weight infants in the Neonatal Research Network of Japan: importance of neonatal intensive care unit graduate follow-up. Clin Exp Pediatr. 2021; 64(7):313–321. PMID: 33171036.20. Pascal A, Govaert P, Oostra A, Naulaers G, Ortibus E, Van den Broeck C. Neurodevelopmental outcome in very preterm and very-low-birthweight infants born over the past decade: a meta-analytic review. Dev Med Child Neurol. 2018; 60(4):342–355. PMID: 29350401.
Article21. Chow SS, Creighton P, Chambers GM, Lui K. Report of the Australian and New Zealand Neonatal Network 2019. Sydney, Australia: Australian and New Zealand Neonatal Network;2021.22. Touyama M, Touyama J, Toyokawa S, Kobayashi Y. Trends in the prevalence of cerebral palsy in children born between 1988 and 2007 in Okinawa, Japan. Brain Dev. 2016; 38(9):792–799. PMID: 27072917.
Article23. Sellier E, Platt MJ, Andersen GL, Krägeloh-Mann I, De La Cruz J, Cans C, et al. Decreasing prevalence in cerebral palsy: a multi-site European population-based study, 1980 to 2003. Dev Med Child Neurol. 2016; 58(1):85–92. PMID: 26330098.
Article24. Arnaud C, Ehlinger V, Delobel-Ayoub M, Klapouszczak D, Perra O, Hensey O, et al. Trends in prevalence and severity of pre/perinatal cerebral palsy among children born preterm from 2004 to 2010: a SCPE collaboration study. Front Neurol. 2021; 12:624884. PMID: 34093391.
Article25. Stolt S, Matomaki J, Lind A, Lapinleimu H, Haataja L, Lehtonen L. The prevalence and predictive value of weak language skills in children with very low birth weight--a longitudinal study. Acta Paediatr. 2014; 103(6):651–658. PMID: 24926485.
Article26. Vandormael C, Schoenhals L, Hüppi PS, Filippa M, Borradori Tolsa C. Language in preterm born children: atypical development and effects of early interventions on neuroplasticity. Neural Plast. 2019; 2019:6873270. PMID: 30930944.
Article27. Monset-Couchard M, de Bethmann O. Catch-up growth in 166 small-for- gestational age premature infants weighing less than 1,000 g at birth. Biol Neonate. 2000; 78(3):161–167. PMID: 11044763.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neonatal outcomes of very low birthweight infants from spontaneous and indicated preterm delivery
- Nutritional Support in Premature Infants
- Neonatal Research Network of Japan and Neonatal Database
- Growth Pattern With Morbidities From Birth to 5 Years of Age in Very Low Birth Weight Infants: Comparison of the Korean National Network and National Health Insurance Service
- Short- and long-term outcomes of very low birth weight infants in Korea: Korean Neonatal Network update in 2019