Arch Hand Microsurg.
2022 Sep;27(3):274-278. 10.12790/ahm.22.0033.
Persistent retrograde venous-lymphatic reflux in side-to-end lymphaticovenous anastomosis in a lower extremity with lymphedema: a case report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2532746
- DOI: http://doi.org/10.12790/ahm.22.0033
Abstract
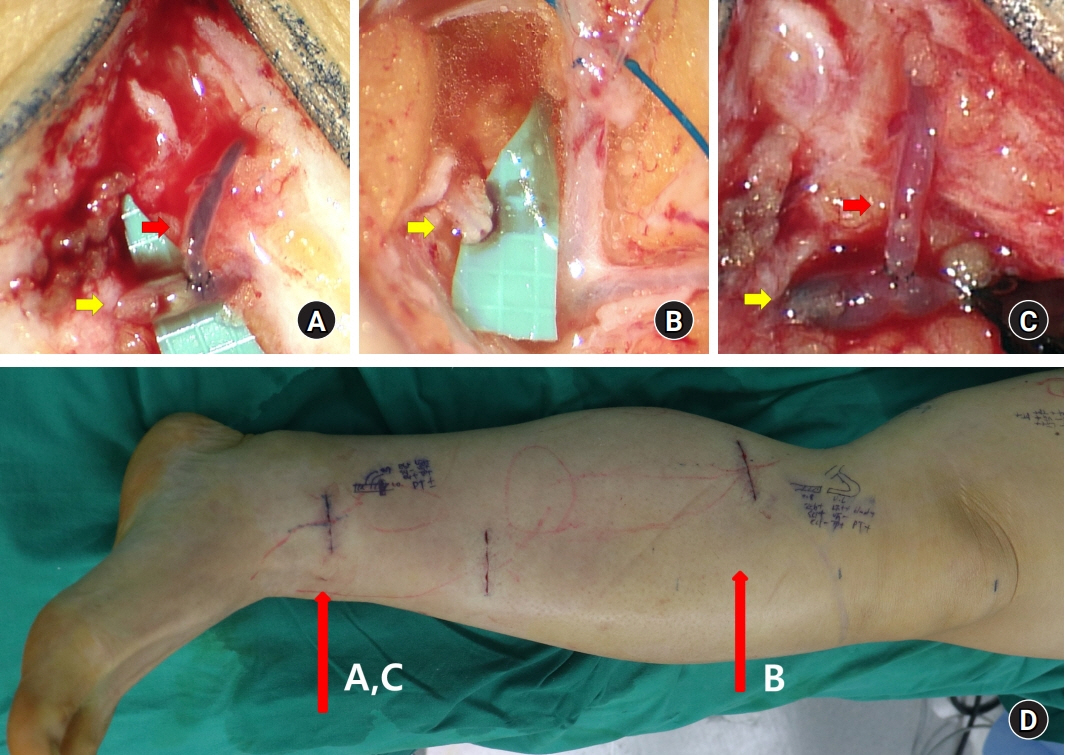
- End-to-end (ETE) and side-to-end (STE) anastomosis are two common configurations of lymphaticovenous anastomosis (LVA); however, it remains inconclusive which method is better. A 62-year-old man with lower extremity lymphedema underwent LVA with the STE method on the ankle. When the lymphatic vessel was cut for additional LVA at the proximal lower leg, blood drained out from the cut end of a lymphatic vessel, which suggested venous-lymphatic reflux at the STE anastomosis at the ankle. Because the reflux continued until 1 hour after the previous LVA at the ankle, the STE anastomosis at the ankle was re-explored and converted to ETE by ligation of the proximal lymphatic vessel. Reverse venous-lymphatic reflux was corrected, and a lymphovenous shunt was created immediately after the ligation. The current case suggests that STE anastomosis can be inferior to ETE anastomosis for creating a lymphovenous shunt when venous backflow exists.
Figure
Reference
-
References
1. Koshima I, Inagawa K, Urushibara K, Moriguchi T. Supermicrosurgical lymphaticovenular anastomosis for the treatment of lymphedema in the upper extremities. J Reconstr Microsurg. 2000; 16:437–42.2. Visconti G, Salgarello M, Hayashi A. The recipient venule in supermicrosurgical lymphaticovenular anastomosis: flow dynamic classification and correlation with surgical outcomes. J Reconstr Microsurg. 2018; 34:581–9.3. Yang JC, Wu SC, Chiang MH, Lin WC. Targeting reflux-free veins with a vein visualizer to identify the ideal recipient vein preoperatively for optimal lymphaticovenous anastomosis in treating lymphedema. Plast Reconstr Surg. 2018; 141:793–7.4. Akita S, Yamaji Y, Tokumoto H, et al. Prevention of venous reflux with full utilization of venoplasty in lymphaticovenular anastomosis. J Plast Reconstr Aesthet Surg. 2020; 73:537–43.5. AlJindan FK, Lin CY, Cheng MH. Comparison of outcomes between side-to-end and end-to-end lymphovenous anastomoses for early-grade extremity Lymphedema. Plast Reconstr Surg. 2019; 144:486–96.6. Yamamoto T, Narushima M, Kikuchi K, et al. Lambda-shaped anastomosis with intravascular stenting method for safe and effective lymphaticovenular anastomosis. Plast Reconstr Surg. 2011; 127:1987–92.7. Suzuki Y, Sakuma H, Ihara J, Shimizu Y. Proximal ligation after the side-to-end anastomosis recovery technique for lymphaticovenous anastomosis. Arch Plast Surg. 2019; 46:344–9.8. Yang JC, Wu SC, Lin WC, Chiang MH, Hsieh CH. Reversing venous-lymphatic reflux following side-to-end lymphaticovenous anastomosis with ligation of the proximal lymphatic vessel. J Plast Reconstr Aesthet Surg. 2021; 74:407–47.9. Dean SM, Valenti E, Hock K, Leffler J, Compston A, Abraham WT. The clinical characteristics of lower extremity lymphedema in 440 patients. J Vasc Surg Venous Lymphat Disord. 2020; 8:851–9.10. Seki Y, Kajikawa A, Yamamoto T, Takeuchi T, Terashima T, Kurogi N. The dynamic-lymphaticovenular anastomosis method for breast cancer treatment-related lymphedema: Creation of functional lymphaticovenular anastomoses with use of preoperative dynamic ultrasonography. J Plast Reconstr Aesthet Surg. 2019; 72:62–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lymphaticovenous Anastomosis in Lower Extremity Lymphedema: A Case Report
- Proximal ligation after the side-to-end anastomosis recovery technique for lymphaticovenous anastomosis
- Surgical treatment of lymphedema
- Acute Lymphedema after Coronary Angiography: A Case Report
- Efficacy and patient satisfaction regarding lymphovenous bypass with sleeve-in anastomosis for extremity lymphedema