Arch Hand Microsurg.
2022 Sep;27(3):258-264. 10.12790/ahm.22.0015.
Effect of renal dysfunction in free flap transfer for chronic wounds of the lower extremities
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Ajou University School of Medicine, Suwon, Korea
- KMID: 2532743
- DOI: http://doi.org/10.12790/ahm.22.0015
Abstract
- Purpose
Free flaps play an important role in the reconstruction of chronic wounds in the lower extremities. Nonetheless, the use of free flaps for chronic wound reconstruction tends to be challenging. A considerable number of patients with chronic wounds have noteworthy medical histories, such as chronic kidney disease or end-stage renal disease (ESRD). This study aimed to determine the relationship between the success rate and complications of free flap surgery according to the degree of kidney disease from normal renal function to ESRD.
Methods
A retrospective study of all patients who underwent free tissue transfer procedures due to chronic wounds in the lower-extremity area over a 9-year period, between October 2011 and February 2020, was conducted. The primary outcome was flap failure, and major complications were set as the secondary outcome.
Results
Sixty-seven consecutive free flaps were used for chronic wounds of the lower extremities at our institution. Flap failure occurred in six patients (9.0%), resulting in a total flap survival rate of 91.0%. Sixteen patients (23.9%) experienced major complications. Flap failure was correlated with the presence of ESRD and renal transplantation.
Conclusion
There are several limiting factors for the reconstruction of chronic wounds in the lower extremity. In particular, ESRD and renal transplantation were significantly correlated with flap failure.
Keyword
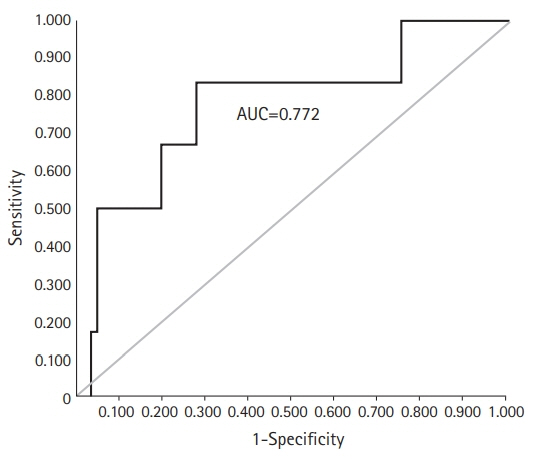
Figure
Reference
-
References
1. Pu LL. A Comprehensive approach to lower extremity free-tissue transfer. Plast Reconstr Surg Glob Open. 2017; 5:e1228.2. Song JY, Kim KS, Kim HD, Park IS. Free tissue transfer in the treatment of infected diabetic foot ulcers. Arch Reconstr Microsurg. 2001; 10:154–62.3. Cooley BC, Hanel DP, Anderson RB, Foster MD, Gould JS. The influence of diabetes on free flap transfer: I. Flap survival and microvascular healing. Ann Plast Surg. 1992; 29:58–64.4. Oh TS, Lee HS, Hong JP. Diabetic foot reconstruction using free flaps increases 5-year-survival rate. J Plast Reconstr Aesthet Surg. 2013; 66:243–50.5. Ou CY, Wu MS, Lin MC, Chang CM. Short-term and long-term outcomes of free flap reconstruction versus amputation for diabetic foot reconstruction in patients with end-stage renal disease. J Plast Reconstr Aesthet Surg. 2022; 75:2511–9.6. Moran SL, Salgado CJ, Serletti JM. Free tissue transfer in patients with renal disease. Plast Reconstr Surg. 2004; 113:2006–11.7. Moran SL, Illig KA, Green RM, Serletti JM. Free-tissue transfer in patients with peripheral vascular disease: a 10-year experience. Plast Reconstr Surg. 2002; 109:999–1006.8. Illig KA, Moran S, Serletti J, et al. Combined free tissue transfer and infrainguinal bypass graft: an alternative to major amputation in selected patients. J Vasc Surg. 2001; 33:17–23.9. Attinger CE, Ducic I, Neville RF, Abbruzzese MR, Gomes M, Sidawy AN. The relative roles of aggressive wound care versus revascularization in salvage of the threatened lower extremity in the renal failure diabetic patient. Plast Reconstr Surg. 2002; 109:1281–92.10. Quiñones-Baldrich WJ, Kashyap VS, Taw MB, et al. Combined revascularization and microvascular free tissue transfer for limb salvage: a six-year experience. Ann Vasc Surg. 2000; 14:99–104.11. Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006; 145:247–54.12. Janhofer DE, Lakhiani C, Kim PJ, et al. The utility of preoperative arteriography for free flap planning in patients with chronic lower extremity wounds. Plast Reconstr Surg. 2019; 143:604–13.13. Chien SH, Huang CC, Hsu H, Chiu CM, Lin CM, Tsai JP. Free tissue transfers for limb salvage in patients with end-stage renal disease on dialysis. Plast Reconstr Surg. 2011; 127:1222–8.14. Haag-Weber M, Hörl WH. Uremia and infection: mechanisms of impaired cellular host defense. Nephron. 1993; 63:125–31.15. Lewis SL, Van Epps DE. Neutrophil and monocyte alterations in chronic dialysis patients. Am J Kidney Dis. 1987; 9:381–95.16. Mahmoodi BK, ten Kate MK, Waanders F, et al. High absolute risks and predictors of venous and arterial thromboembolic events in patients with nephrotic syndrome: results from a large retrospective cohort study. Circulation. 2008; 117:224–30.17. Yue DK, McLennan S, Marsh M, et al. Effects of experimental diabetes, uremia, and malnutrition on wound healing. Diabetes. 1987; 36:295–9.18. Kim B, Yoon J, Lim S, Han YS, Eo S. Anterolateral thigh free flap to cover diabetic foot defect by using reverse flow of severely calcified dorsalis pedis artery. Arch Hand Microsurg. 2021; 26:293–7.19. Sbitany H, Xu X, Hansen SL, Young DM, Hoffman WY. The effects of immunosuppressive medications on outcomes in microvascular free tissue transfer. Plast Reconstr Surg. 2014; 133:552e–558e.20. Lee AB, Dupin CL, Colen L, Jones NF, May JW, Chiu ES. Microvascular free tissue transfer in organ transplantation patients: is it safe? Plast Reconstr Surg. 2008; 121:1986–92.21. Åberg F, Isoniemi H, Höckerstedt K. Long-term results of liver transplantation. Scand J Surg. 2011; 100:14–21.22. D'Marco L, Bellasi A, Mazzaferro S, Raggi P. Vascular calcification, bone and mineral metabolism after kidney transplantation. World J Transplant. 2015; 5:222–30.23. Davies MR, Hruska KA. Pathophysiological mechanisms of vascular calcification in end-stage renal disease. Kidney Int. 2001; 60:472–9.24. Bandyk DF. The diabetic foot: pathophysiology, evaluation, and treatment. Semin Vasc Surg. 2018; 31:43–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Stduy of Vascularized Lateral Thigh Free Flap
- Reconstruction of the Tissue Defects of Extremities with Anterolateral Thigh Free Flap
- Lower Extremity Reconstruction of Soft Tissue Defects with Perforator Island Flap
- The Fascial Radial Flap Transfer: Case Report
- Reconstruction of Soft - Tissue Defects in the Lower Extremities Using Local or Free Muscle Flaps