Healthc Inform Res.
2022 Jul;28(3):256-266. 10.4258/hir.2022.28.3.256.
Unsupervised Machine Learning to Identify Depressive Subtypes
- Affiliations
-
- 1Carbon Health, San Mateo, CA, USA
- 2Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
- 3NIHR Maudsley BRC, London, UK
- 4South London and Maudsley NHS Foundation Trust, Beckenham, UK
- KMID: 2532453
- DOI: http://doi.org/10.4258/hir.2022.28.3.256
Abstract
Objectives
This study evaluated an unsupervised machine learning method, latent Dirichlet allocation (LDA), as a method for identifying subtypes of depression within symptom data.
Methods
Data from 18,314 depressed patients were used to create LDA models. The outcomes included future emergency presentations, crisis events, and behavioral problems. One model was chosen for further analysis based upon its potential as a clinically meaningful construct. The associations between patient groups created with the final LDA model and outcomes were tested. These steps were repeated with a commonly-used latent variable model to provide additional context to the LDA results.
Results
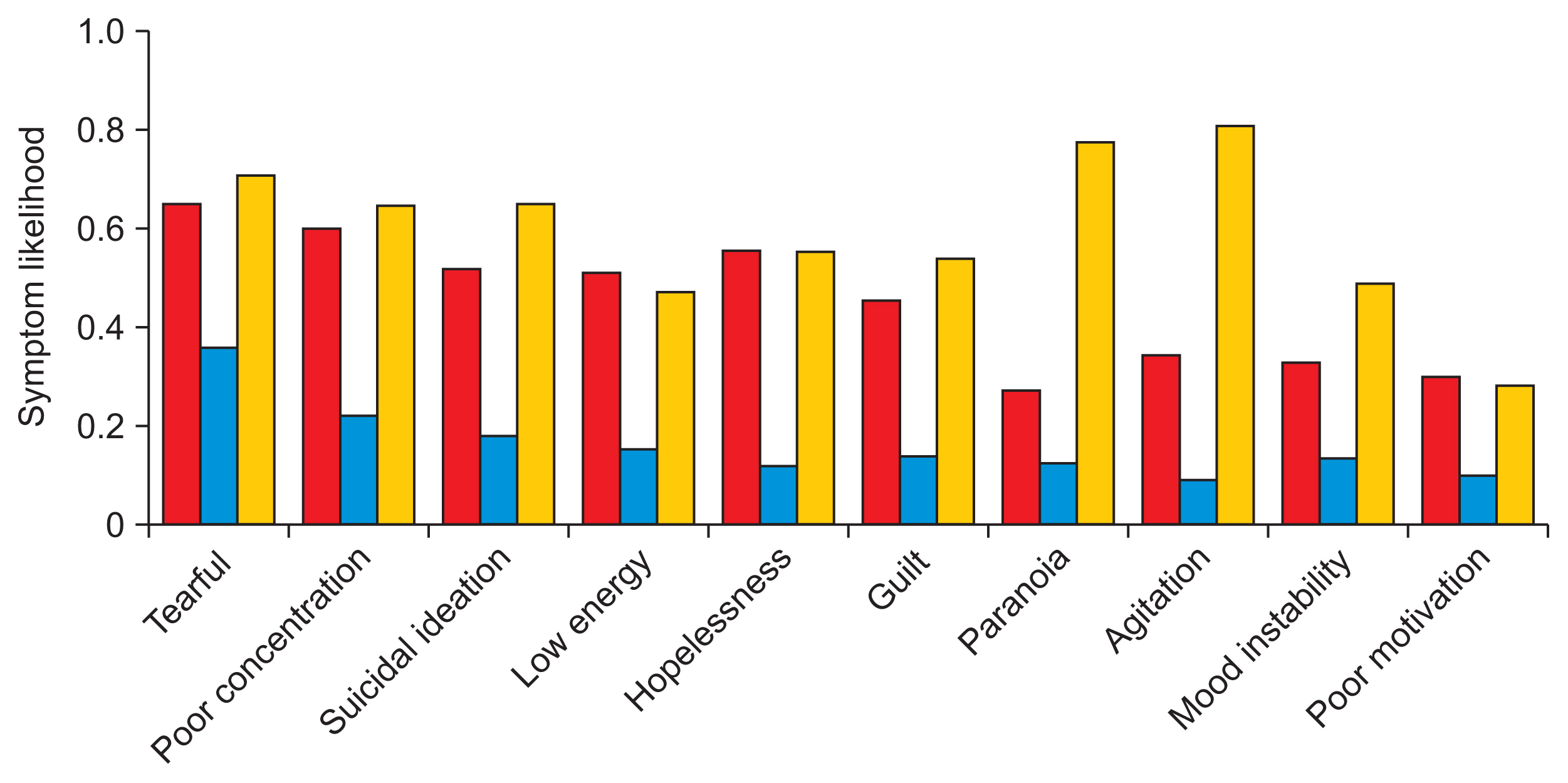
Five subtypes were identified using the final LDA model. Prior to the outcome analysis, the subtypes were labeled based upon the symptom distributions they produced: psychotic, severe, mild, agitated, and anergic-apathetic. The patient groups largely aligned with the outcome data. For example, the psychotic and severe subgroups were more likely to have emergency presentations (odds ratio [OR] = 1.29; 95% confidence interval [CI], 1.17–1.43 and OR = 1.16; 95% CI, 1.05–1.29, respectively), whereas these outcomes were less likely in the mild subgroup (OR = 0.86; 95% CI, 0.78–0.94). We found that the LDA subtypes were characterized by clusters of unique symptoms. This contrasted with the latent variable model subtypes, which were largely stratified by severity.
Conclusions
This study suggests that LDA can surface clinically meaningful, qualitative subtypes. Future work could be incorporated into studies concerning the biological bases of depression, thereby contributing to the development of new psychiatric therapeutics.
Figure
Reference
-
References
1. World Health Organization. Depression and other common mental disorders: global health estimates. Geneva, Switzerland: World Health Organization;2017.2. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018; 392(10159):1789–858. https://doi.org/10.1016/s0140-6736(18)32279-7.3. Warden D, Rush AJ, Trivedi MH, Fava M, Wisniewski SR. The STAR*D Project results: a comprehensive review of findings. Curr Psychiatry Rep. 2007; 9(6):449–59. https://doi.org/10.1007/s11920-007-0061-3.
Article4. Kern DM, Cepeda MS, Defalco F, Etropolski M. Treatment patterns and sequences of pharmacotherapy for patients diagnosed with depression in the United States: 2014 through 2019. BMC Psychiatry. 2020; 20(1):4. https://doi.org/10.1186/s12888-019-2418-7.
Article5. Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010; 167(7):748–51. https://doi.org/10.1176/appi.ajp.2010.09091379.
Article6. Hasler G, Drevets WC, Manji HK, Charney DS. Discovering endophenotypes for major depression. Neuropsychopharmacology. 2004; 29(10):1765–81. https://doi.org/10.1038/sj.npp.1300506.
Article7. Rush AJ. The varied clinical presentations of major depressive disorder. J Clin Psychiatry. 2007; 68(Suppl 8):4–10.8. van Loo HM, de Jonge P, Romeijn JW, Kessler RC, Schoevers RA. Data-driven subtypes of major depressive disorder: a systematic review. BMC Med. 2012; 10:156. https://doi.org/10.1186/1741-7015-10-156.
Article9. Ulbricht CM, Chrysanthopoulou SA, Levin L, Lapane KL. The use of latent class analysis for identifying subtypes of depression: a systematic review. Psychiatry Res. 2018; 266:228–46. https://doi.org/10.1016/j.psychres.2018.03.003.
Article10. Marquand AF, Wolfers T, Mennes M, Buitelaar J, Beckmann CF. Beyond lumping and splitting: a review of computational approaches for stratifying psychiatric disorders. Biol Psychiatry Cogn Neurosci Neuroimaging. 2016; 1(5):433–47. https://doi.org/10.1016/j.bpsc.2016.04.002.
Article11. Fernandes BS, Williams LM, Steiner J, Leboyer M, Carvalho AF, Berk M. The new field of 'precision psychiatry'. BMC Med. 2017; 15(1):80. https://doi.org/10.1186/s12916-017-0849-x.
Article12. Horwitz T, Lam K, Chen Y, Xia Y, Liu C. A decade in psychiatric GWAS research. Mol Psychiatry. 2019; 24(3):378–89. https://doi.org/10.1038/s41380-018-0055-z.
Article13. Fried EI, Nesse RM. Depression is not a consistent syndrome: An investigation of unique symptom patterns in the STAR*D study. J Affect Disord. 2015; 172:96–102. https://doi.org/10.1016/j.jad.2014.10.010.
Article14. Blei DM, Ng AY, Jordan MI. Latent Dirichlet allocation. J Mach Learn Res. 2003; 3:993–1022.15. Mori M, Krumholz HM, Allore HG. Using latent class analysis to identify hidden clinical phenotypes. JAMA. 2020; 324(7):700–1. https://doi.org/10.1001/jama.2020.2278.
Article16. Lamers F, de Jonge P, Nolen WA, Smit JH, Zitman FG, Beekman AT, et al. Identifying depressive subtypes in a large cohort study: results from the Netherlands Study of Depression and Anxiety (NESDA). J Clin Psychiatry. 2010; 71(12):1582–9. https://doi.org/10.4088/jcp.09m05398blu.
Article17. Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the national comorbidity survey. Am J Psychiatry. 1998; 155(10):1398–406. https://doi.org/10.1176/ajp.155.10.1398.
Article18. Perera G, Broadbent M, Callard F, Chang CK, Downs J, Dutta R, et al. Cohort profile of the South London and Maudsley NHS foundation trust Biomedical Research Centre (SLaM BRC) case register: current status and recent enhancement of an Electronic Mental Health Record-derived data resource. BMJ Open. 2016; 6(3):e008721. https://doi.org/10.1136/bmjopen-2015-008721.
Article19. Fernandes AC, Cloete D, Broadbent MT, Hayes RD, Chang CK, Jackson RG, et al. Development and evaluation of a de-identification procedure for a case register sourced from mental health electronic records. BMC Med Inform Decis Mak. 2013; 13:71. https://doi.org/10.1186/1472-6947-13-71.
Article20. CRIS NLP Service. Library of production-ready applications [Internet]. London, UK: NIHR Maudsley Biomedical Research Centre;2020. [cited at 2022 Jul 25]. Available from: https://maudsleybrc.nihr.ac.uk/media/313772/applications-library-v12.pdf.21. Delaffon V, Anwar Z, Noushad F, Ahmed AS, Brugha TS. Use of Health of the Nation Outcome Scales in psychiatry. Adv Psychiatr Treat. 2012; 18(3):173–9. https://doi.org/10.1192/apt.bp.110.008029.
Article22. Linzer DA, Lewis JB. poLCA: an R package for polytomous variable latent class analysis. J Stat Softw. 2011; 42(10):1–29. https://doi.org/10.18637/jss.v042.i10.
Article23. Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, et al. Scikit-learn: machine learning in Python. J Mach Learn Res. 2011; 12:2825–2830.24. Tolentino JC, Schmidt SL. DSM-5 criteria and depression severity: implications for clinical practice. Front Psychiatry. 2018; 9:450. https://doi.org/10.3389/fpsyt.2018.00450.
Article25. Lowe B, Spitzer RL, Grafe K, Kroenke K, Quenter A, Zipfel S, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians' diagnoses. J Affect Disord. 2004; 78(2):131–40. https://doi.org/10.1016/s0165-0327(02)00237-9.
Article26. van Loo HM, Wanders RB, Wardenaar KJ, Fried EI. Problems with latent class analysis to detect data-driven subtypes of depression. Mol Psychiatry. 2018; 23(3):495–6. https://doi.org/10.1038/mp.2016.202.
Article27. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Article28. Liu CH, Stevens C, Wong SH, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress Anxiety. 2019; 36(1):8–17. https://doi.org/10.1002/da.22830.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparative Study of Unsupervised Deep Learning Methods for MRI Reconstruction
- Simultaneous Utilization of Mood Disorder Questionnaire and Bipolar Spectrum Diagnostic Scale for Machine Learning-Based Classification of Patients With Bipolar Disorders and Depressive Disorders
- Artificial Intelligence for Clinical Research in Voice Disease
- Application of Deep Learning System into the Development of Communication Device for Quadriplegic Patient
- Non-invasive biomarkers for liver inflammation in non-alcoholic fatty liver disease: present and future