J Korean Med Sci.
2022 Aug;37(32):e248. 10.3346/jkms.2022.37.e248.
The Association Between Antihypertensive Drug Use and Hospitalization for Pneumonia in the General Population: A Case-Crossover Study Using the National Health Insurance Database of Korea
- Affiliations
-
- 1Department of Rehabilitation Medicine, Pohang Stroke and Spine Hospital, Pohang, Korea
- 2Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Research and Analysis Team, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 4National Traffic Injury Rehabilitation Hospital, Yangpyeong, Korea
- 5Institute on Aging, Seoul National University, Seoul, Korea
- 6Department of Physical Medicine and Rehabilitation, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2532322
- DOI: http://doi.org/10.3346/jkms.2022.37.e248
Abstract
- Background
Previous studies have reported an association between pneumonia risk and the use of certain drugs. We investigated the relationship between antihypertensive drugs and pneumonia in the general population.
Methods
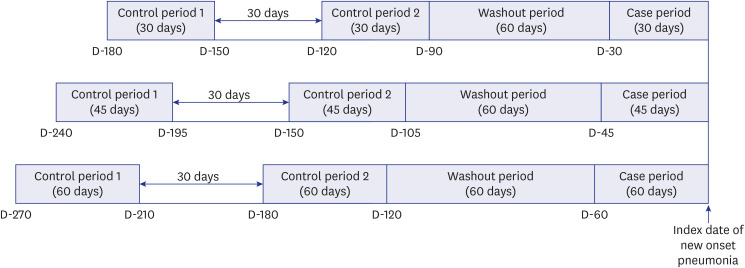
This case-crossover study utilized the nationwide data of South Korea. We included participants who were hospitalized for pneumonia. A single case period was defined as 30 days before pneumonia onset, and two control periods were established (90–120 and 150–180 days before pneumonia onset). Further, we performed sensitivity and subgroup analyses (according to the presence of diabetes, documented disability, and whether participants were aged ≥ 70 years). We used conditional logistic regression models adjusted for covariates, such as angiotensin-converting-enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), other antihypertensives, statins, antipsychotics, benzodiazepine, and the number of outpatient visits.
Results
In total, 15,463 subjects were included in this study. ACE inhibitors (adjusted odds ratio [aOR], 0.660; 95% confidence interval [CI], 0.558–0.781), ARBs (aOR, 0.702; 95% CI, 0.640–0.770), and other antihypertensive drugs (aOR, 0.737; 95% CI, 0.665–0.816) were significantly associated with reduced pneumonia risk. Subgroup analyses according to the presence of diabetes mellitus, documented disability, and whether participants were aged ≥ 70 years consistently showed the association of antihypertensives with a reduced risk of hospitalization for pneumonia.
Conclusion
All antihypertensive drug types were related to a lower risk of hospitalization for pneumonia in the general population. Our results implied that frequent medical service usage and protective immunity were primarily related to a reduced risk of pneumonia in the general population of South Korea.
Keyword
Figure
Reference
-
1. Buzzo AR, Roberts C, Mollinedo LG, Quevedo JM, Casas GL, Soldevilla JM. Morbidity and mortality of pneumonia in adults in six Latin American countries. Int J Infect Dis. 2013; 17(9):e673–e677. PMID: 23558317.
Article2. Statistics Korea. 2020 cause of death statistics. Updated 2021. Accessed February 24, 2022. http://kosis.kr .3. Schmedt N, Heuer OD, Häckl D, Sato R, Theilacker C. Burden of community-acquired pneumonia, predisposing factors and health-care related costs in patients with cancer. BMC Health Serv Res. 2019; 19(1):30. PMID: 30642312.
Article4. Lim WS. Pneumonia—overview. Janes SM, editor. Encyclopedia of Respiratory Medicine. Amsterdam, Netherlands: Elsevier;2022. p. 185–197.5. Huang KH, Kuo WY, Kuan YH, Chang YC, Tsai TH, Lee CY. Risk of pneumonia is associated with antipsychotic drug use among older patients with Parkinson’s disease: a case-control study. Int J Med Sci. 2021; 18(15):3565–3573. PMID: 34522183.
Article6. Liapikou A, Cilloniz C, Torres A. Drugs that increase the risk of community-acquired pneumonia: a narrative review. Expert Opin Drug Saf. 2018; 17(10):991–1003. PMID: 30196729.
Article7. Restrepo MI, Mortensen EM, Anzueto A. Common medications that increase the risk for developing community-acquired pneumonia. Curr Opin Infect Dis. 2010; 23(2):145–151. PMID: 20075727.
Article8. van de Garde EM, Souverein PC, van den Bosch JM, Deneer VH, Leufkens HG. Angiotensin-converting enzyme inhibitor use and pneumonia risk in a general population. Eur Respir J. 2006; 27(6):1217–1222. PMID: 16455828.
Article9. Liu CL, Shau WY, Wu CS, Lai MS. Angiotensin-converting enzyme inhibitor/angiotensin II receptor blockers and pneumonia risk among stroke patients. J Hypertens. 2012; 30(11):2223–2229. PMID: 22929610.
Article10. van de Garde EM, Souverein PC, Hak E, Deneer VH, van den Bosch JM, Leufkens HG. Angiotensin-converting enzyme inhibitor use and protection against pneumonia in patients with diabetes. J Hypertens. 2007; 25(1):235–239. PMID: 17143196.
Article11. Caldeira D, Alarcão J, Vaz-Carneiro A, Costa J. Risk of pneumonia associated with use of angiotensin converting enzyme inhibitors and angiotensin receptor blockers: systematic review and meta-analysis. BMJ. 2012; 345:e4260. PMID: 22786934.
Article12. Yun JH, Rhee SY, Chun S, Kim HS, Oh BM. Association between antihypertensive use and hospitalized pneumonia in patients with stroke: a Korean nationwide population-based cohort study. J Korean Med Sci. 2022; 37(15):e112. PMID: 35437963.
Article13. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.
Article14. Lee JS, Chui PY, Ma HM, Auyeung TW, Kng C, Law T, et al. Does low dose angiotensin converting enzyme inhibitor prevent pneumonia in older people with neurologic dysphagia--a randomized placebo-controlled trial. J Am Med Dir Assoc. 2015; 16(8):702–707. PMID: 26123256.
Article15. Ohkubo T, Chapman N, Neal B, Woodward M, Omae T, Chalmers J, et al. Effects of an angiotensin-converting enzyme inhibitor-based regimen on pneumonia risk. Am J Respir Crit Care Med. 2004; 169(9):1041–1045. PMID: 14990394.
Article16. Sekizawa K, Matsui T, Nakagawa T, Nakayama K, Sasaki H. ACE inhibitors and pneumonia. Lancet. 1998; 352(9133):1069.
Article17. Wang HC, Lin CC, Lau CI, Chang A, Kao CH. Angiotensin-converting enzyme inhibitors and bacterial pneumonia in patients with Parkinson disease. Mov Disord. 2015; 30(4):593–596. PMID: 25641619.
Article18. Shinohara Y, Origasa H. Post-stroke pneumonia prevention by angiotensin-converting enzyme inhibitors: results of a meta-analysis of five studies in Asians. Adv Ther. 2012; 29(10):900–912. PMID: 22983755.
Article19. Williams VR, Scholey JW. Angiotensin-converting enzyme 2 and renal disease. Curr Opin Nephrol Hypertens. 2018; 27(1):35–41. PMID: 29045335.
Article20. Paul M, Poyan Mehr A, Kreutz R. Physiology of local renin-angiotensin systems. Physiol Rev. 2006; 86(3):747–803. PMID: 16816138.
Article21. Just PM. The positive association of cough with angiotensin-converting enzyme inhibitors. Pharmacotherapy. 1989; 9(2):82–87. PMID: 2657676.
Article22. Tomaki M, Ichinose M, Miura M, Hirayama Y, Kageyama N, Yamauchi H, et al. Angiotensin converting enzyme (ACE) inhibitor-induced cough and substance P. Thorax. 1996; 51(2):199–201. PMID: 8711657.
Article23. El Solh AA, Saliba R. Pharmacologic prevention of aspiration pneumonia: a systematic review. Am J Geriatr Pharmacother. 2007; 5(4):352–362. PMID: 18179994.
Article24. Ikeda J, Kojima N, Saeki K, Ishihara M, Takayama M. Perindopril increases the swallowing reflex by inhibiting substance P degradation and tyrosine hydroxylase activation in a rat model of dysphagia. Eur J Pharmacol. 2015; 746:126–131. PMID: 25445054.
Article25. Arai T, Yasuda Y, Takaya T, Toshima S, Kashiki Y, Yoshimi N, et al. ACE inhibitors and symptomless dysphagia. Lancet. 1998; 352(9122):115–116. PMID: 9672283.
Article26. El-Hashim AZ, Amine SA. The role of substance P and bradykinin in the cough reflex and bronchoconstriction in guinea-pigs. Eur J Pharmacol. 2005; 513(1-2):125–133. PMID: 15878717.
Article27. Nataraj C, Oliverio MI, Mannon RB, Mannon PJ, Audoly LP, Amuchastegui CS, et al. Angiotensin II regulates cellular immune responses through a calcineurin-dependent pathway. J Clin Invest. 1999; 104(12):1693–1701. PMID: 10606623.
Article28. Di Raimondo D, Tuttolomondo A, Buttà C, Miceli S, Licata G, Pinto A. Effects of ACE-inhibitors and angiotensin receptor blockers on inflammation. Curr Pharm Des. 2012; 18(28):4385–4413. PMID: 22283779.
Article29. Shrikrishna D, Astin R, Kemp PR, Hopkinson NS. Renin-angiotensin system blockade: a novel therapeutic approach in chronic obstructive pulmonary disease. Clin Sci (Lond). 2012; 123(8):487–498. PMID: 22757959.
Article30. Dublin S, Walker RL, Jackson ML, Nelson JC, Weiss NS, Jackson LA. Angiotensin-converting enzyme inhibitor use and pneumonia risk in community-dwelling older adults: results from a population-based case-control study. Pharmacoepidemiol Drug Saf. 2012; 21(11):1173–1182. PMID: 22949094.
Article31. Liu CL, Shau WY, Chang CH, Wu CS, Lai MS. Pneumonia risk and use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers. J Epidemiol. 2013; 23(5):344–350. PMID: 23912052.
Article32. Gillespie SH, Balakrishnan I. Pathogenesis of pneumococcal infection. J Med Microbiol. 2000; 49(12):1057–1067. PMID: 11129716.
Article33. DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care. 2015; 30(1):40–48. PMID: 25129577.
Article34. Lansbury L, Lim B, McKeever TM, Lawrence H, Lim WS. Non-invasive pneumococcal pneumonia due to vaccine serotypes: a systematic review and meta-analysis. eClinicalMedicine. 2022; 44:101271. PMID: 35112072.
Article35. Said MA, Johnson HL, Nonyane BA, Deloria-Knoll M, O’Brien KL, Andreo F, et al. Estimating the burden of pneumococcal pneumonia among adults: a systematic review and meta-analysis of diagnostic techniques. PLoS One. 2013; 8(4):e60273. PMID: 23565216.
Article36. Imamura Y, Miyazaki T, Watanabe A, Tsukada H, Nagai H, Hasegawa Y, et al. Prospective multicenter survey for Nursing and Healthcare-associated Pneumonia in Japan. J Infect Chemother. 2022; 28(8):1125–1130. PMID: 35414437.
Article37. Andersen CT, Langendorf C, Garba S, Sayinzonga-Makombe N, Mambula C, Mouniaman I, et al. Risk of community- and hospital-acquired bacteremia and profile of antibiotic resistance in children hospitalized with severe acute malnutrition in Niger. Int J Infect Dis. 2022; 119:163–171. PMID: 35346836.
Article38. Jaradeh S. Neurophysiology of swallowing in the aged. Dysphagia. 1994; 9(4):218–220. PMID: 7805419.
Article39. Tracy JF, Logemann JA, Kahrilas PJ, Jacob P, Kobara M, Krugler C. Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia. 1989; 4(2):90–94. PMID: 2640185.
Article40. Ren J, Shaker R, Kusano M, Podvrsan B, Metwally N, Dua KS, et al. Effect of aging on the secondary esophageal peristalsis: presbyesophagus revisited. Am J Physiol. 1995; 268(5 Pt 1):G772–G779. PMID: 7762661.
Article41. Nilsson H, Ekberg O, Olsson R, Hindfelt B. Quantitative aspects of swallowing in an elderly nondysphagic population. Dysphagia. 1996; 11(3):180–184. PMID: 8755461.
Article42. Benfield T, Jensen JS, Nordestgaard BG. Influence of diabetes and hyperglycaemia on infectious disease hospitalisation and outcome. Diabetologia. 2007; 50(3):549–554. PMID: 17187246.
Article43. Jensen AV, Faurholt-Jepsen D, Egelund GB, Andersen SB, Petersen PT, Benfield T, et al. Undiagnosed diabetes mellitus in community-acquired pneumonia: a prospective cohort study. Clin Infect Dis. 2017; 65(12):2091–2098. PMID: 29095981.44. Pratt N, Roughead EE, Ramsay E, Salter A, Ryan P. Risk of hospitalization for hip fracture and pneumonia associated with antipsychotic prescribing in the elderly: a self-controlled case-series analysis in an Australian health care claims database. Drug Saf. 2011; 34(7):567–575. PMID: 21663332.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association Between Antihypertensive Use and Hospitalized Pneumonia in Patients With Stroke: A Korean Nationwide Population-Based Cohort Study
- Trends in the Quality of Primary Care and Acute Care in Korea From 2008 to 2020: A Cross-sectional Study
- Letter: Increased Risk of Hospitalization for Heart Failure with Newly Prescribed Dipeptidyl Peptidase-4 Inhibitors and Pioglitazone Using the Korean Health Insurance Claims Database (Diabetes Metab J 2015;39:247-52)
- Clinical Study Using Healthcare Claims Database
- Introducing big data analysis using data from National Health Insurance Service