J Korean Med Sci.
2022 Aug;37(30):e236. 10.3346/jkms.2022.37.e236.
Phenotype of Asthma-COPD Overlap in COPD and Severe Asthma Cohorts
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea
- 4Department of Statistics and Data Science, Korea National Open University, Seoul, Korea
- 5Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- 6Department of Allergy and Clinical Immunology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 7Department of Pulmonary, Allergy and Critical Care Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- 8Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2532230
- DOI: http://doi.org/10.3346/jkms.2022.37.e236
Abstract
- Background
Asthma and chronic obstructive pulmonary disease (COPD) are airway diseases with similar clinical manifestations, despite differences in pathophysiology. AsthmaCOPD overlap (ACO) is a condition characterized by overlapping clinical features of both diseases. There have been few reports regarding the prevalence of ACO in COPD and severe asthma cohorts. ACO is heterogeneous; patients can be classified on the basis of phenotype differences. This study was performed to analyze the prevalence of ACO in COPD and severe asthma cohorts. In addition, this study compared baseline characteristics among ACO patients according to phenotype.
Methods
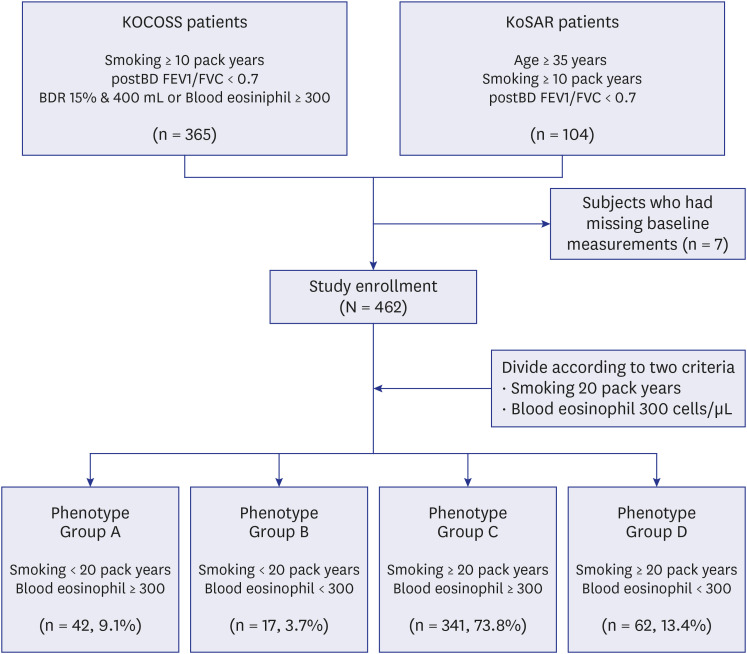
Patients with COPD were prospectively enrolled into the Korean COPD subgroup study (KOCOSS) cohort. Patients with severe asthma were prospectively enrolled into the Korean Severe Asthma Registry (KoSAR). ACO was defined in accordance with the updated Spanish criteria. In the COPD cohort, ACO was defined as bronchodilator response (BDR) ≥ 15% and ≥ 400 mL from baseline or blood eosinophil count (BEC) ≥ 300 cells/μL. In the severe asthma cohort, ACO was defined as age ≥ 35 years, smoking ≥ 10 pack-years, and postbronchodilator forced expiratory volume in 1 s/forced vital capacity < 0.7. Patients with ACO were divided into four groups according to smoking history (threshold: 20 pack-years) and BEC (threshold: 300 cells/μL).
Results
The prevalence of ACO significantly differed between the COPD and severe asthma cohorts (19.8% [365/1,839] vs. 12.5% [104/832], respectively; P < 0.001). The percentage of patients in each group was as follows: group A (light smoker with high BEC) – 9.1%; group B (light smoker with low BEC) – 3.7%; group C (moderate to heavy smoker with high BEC) – 73.8%; and group D (moderate to heavy smoker with low BEC) – 13.4%. Moderate to heavy smoker with high BEC group was oldest, and showed weak BDR response. Age, sex, BDR, comorbidities, and medications significantly differed among the four groups.
Conclusion
The prevalence of ACO differed between COPD and severe asthma cohorts. ACO patients can be classified into four phenotype groups, such that each phenotype exhibits distinct characteristics.
Figure
Cited by 1 articles
-
Asthma-COPD Overlap in Two Comprehensive Cohorts in Korea: Time to Move to Treatable Traits
Kyoung-Hee Sohn
J Korean Med Sci. 2022;37(30):e247. doi: 10.3346/jkms.2022.37.e247.
Reference
-
1. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. Updated 2021. Accessed April 15, 2017. www.ginasthma.org .2. Lainez S, Court-Fortune I, Vercherin P, Falchero L, Didi T, Beynel P, et al. Clinical ACO phenotypes: description of a heterogeneous entity. Respir Med Case Rep. 2019; 28:100929. PMID: 31516821.
Article3. Miravitlles M, Soriano JB, Ancochea J, Muñoz L, Duran-Tauleria E, Sánchez G, et al. Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med. 2013; 107(7):1053–1060. PMID: 23597591.
Article4. Miravitlles M, Huerta A, Fernández-Villar JA, Alcázar B, Villa G, Forné C, et al. Generic utilities in COPD patients stratified according to different staging systems. Health Qual Life Outcomes. 2014; 12:120. PMID: 25189786.5. Golpe R, Sanjuán López P, Cano Jiménez E, Castro Añón O, Pérez de Llano LA. Distribution of clinical phenotypes in patients with chronic obstructive pulmonary disease caused by biomass and tobacco smoke. Arch Bronconeumol. 2014; 50(8):318–324. PMID: 24576449.
Article6. Vaz Fragoso CA, Murphy TE, Agogo GO, Allore HG, McAvay GJ. Asthma-COPD overlap syndrome in the US: a prospective population-based analysis of patient-reported outcomes and health care utilization. Int J Chron Obstruct Pulmon Dis. 2017; 12:517–527. PMID: 28223792.7. Alshabanat A, Zafari Z, Albanyan O, Dairi M, FitzGerald JM. Asthma and COPD overlap syndrome (ACOS): a systematic review and meta analysis. PLoS One. 2015; 10(9):e0136065. PMID: 26336076.
Article8. Barrecheguren M, Esquinas C, Miravitlles M. The asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): opportunities and challenges. Curr Opin Pulm Med. 2015; 21(1):74–79. PMID: 25405671.9. Bonten TN, Kasteleyn MJ, de Mutsert R, Hiemstra PS, Rosendaal FR, Chavannes NH, et al. Defining asthma-COPD overlap syndrome: a population-based study. Eur Respir J. 2017; 49(5):1602008. PMID: 28461292.
Article10. Joo H, Han D, Lee JH, Rhee CK. Heterogeneity of asthma-COPD overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2017; 12:697–703. PMID: 28260876.11. Kim MH, Rhee CK, Kim K, Kim SH, Lee JY, Kim YH, et al. Heterogeneity of asthma and COPD overlap. Int J Chron Obstruct Pulmon Dis. 2018; 13:1251–1260. PMID: 29713158.
Article12. Rhee CK. Phenotype of asthma-chronic obstructive pulmonary disease overlap syndrome. Korean J Intern Med. 2015; 30(4):443–449. PMID: 26161009.
Article13. Kim MH, Kim SH, Park SY, Ban GY, Kim JH, Jung JW, et al. Characteristics of adult severe refractory asthma in Korea analyzed from the severe asthma registry. Allergy Asthma Immunol Res. 2019; 11(1):43–54. PMID: 30479076.
Article14. Lee H, Kim SH, Kim BK, Lee Y, Lee HY, Ban GY, et al. Characteristics of specialist-diagnosed asthma-COPD overlap in severe asthma: observations from the Korean Severe Asthma Registry (KoSAR). Allergy. 2021; 76(1):223–232. PMID: 33411398.
Article15. Plaza V, Álvarez F, Calle M, Casanova C, Cosío BG, López-Viña A, et al. Consensus on the asthma-COPD overlap syndrome (ACOS) between the Spanish COPD Guidelines (GesEPOC) and the Spanish Guidelines on the Management of Asthma (GEMA). Arch Bronconeumol. 2017; 53(8):443–449. PMID: 28495077.
Article16. Neumann T, Rasmussen M, Heitmann BL, Tønnesen H. Gold standard program for heavy smokers in a real-life setting. Int J Environ Res Public Health. 2013; 10(9):4186–4199. PMID: 24022655.
Article17. Lee YH, Shin MH, Kweon SS, Choi JS, Rhee JA, Ahn HR, et al. Cumulative smoking exposure, duration of smoking cessation, and peripheral arterial disease in middle-aged and older Korean men. BMC Public Health. 2011; 11(1):94. PMID: 21310081.
Article18. Singh D, Kolsum U, Brightling CE, Locantore N, Agusti A, Tal-Singer R, et al. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014; 44(6):1697–1700. PMID: 25323230.
Article19. Bafadhel M, Pavord ID, Russell RE. Eosinophils in COPD: just another biomarker? Lancet Respir Med. 2017; 5(9):747–759. PMID: 28601554.
Article20. Vedel-Krogh S, Nielsen SF, Lange P, Vestbo J, Nordestgaard BG. Blood eosinophils and exacerbations in chronic obstructive pulmonary disease. the Copenhagen General Population Study. Am J Respir Crit Care Med. 2016; 193(9):965–974. PMID: 26641631.
Article21. Yun JH, Lamb A, Chase R, Singh D, Parker MM, Saferali A, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018; 141(6):2037–2047.e10. PMID: 29709670.22. Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009; 64(8):728–735. PMID: 19638566.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overlap Between Asthma and COPD: Where the Two Diseases Converge
- Status of Studies Investigating Asthma–Chronic Obstructive Pulmonary Disease Overlap in Korea: A Review
- Systemic Inflammation in Older Adults With Asthma-COPD Overlap Syndrome
- The Relationship of Chronic Obstructive Pulmonary Disease (COPD) to Asthma
- Comparison of Endothelin Release in Bronchial Asthma, Chronic Obstructive Pulmonary Disease and Healthy Controls