J Rhinol.
2022 Jul;29(2):118-121. 10.18787/jr.2022.00404.
A Case With Herpes Zoster Ophthalmicus Mimicking Delayed Complication of Rhinoplasty
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Republic of Korea
- KMID: 2532015
- DOI: http://doi.org/10.18787/jr.2022.00404
Abstract
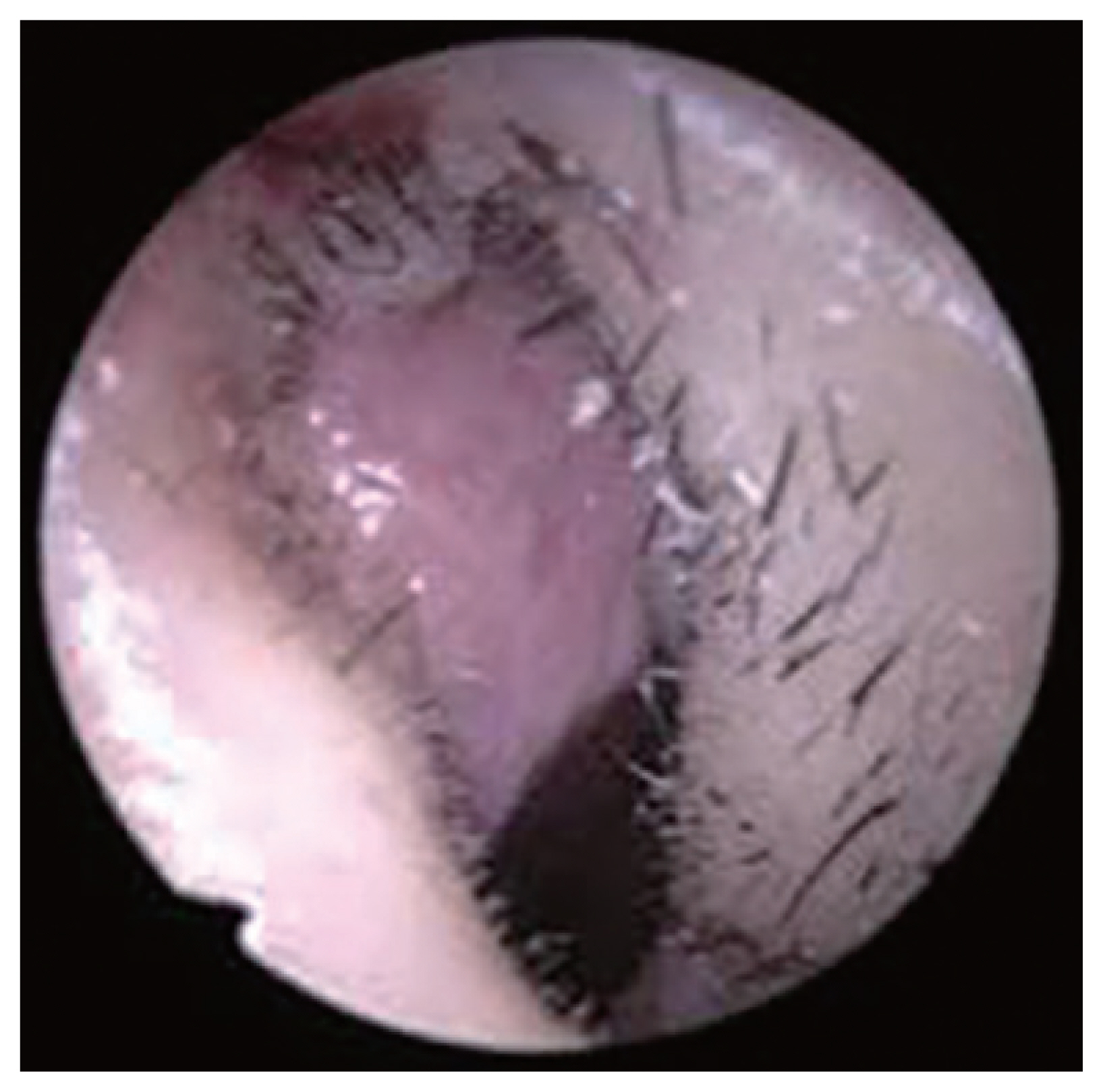
- Herpes zoster ophthalmicus (HZO) occurs due to reactivation of dormant varicella zoster virus infection in the ophthalmic division of the trigeminal nerve. Hutchinson’s sign, a herpetic skin lesion in the nasal tip, is a predictor of ocular complications, as the nasal tip area and ocular structure are innervated by the same nasociliary nerve. Patients who present with Hutchinson’s sign should be referred to an ophthalmologist due to possibility of ocular complications. Here, we present a case of a 44-year-old man with HZO that was confused with delayed rhinoplasty complication. The patient presented with nasal tip skin lesions 17 years after undergoing augmentation rhinoplasty. A graft-related infection was suspected due to operation history and skin lesions. However, surgical exploration disclosed no infection or inflammation, and serological tests revealed positive varicella zoster virus immunoglobulin M, and immunoglobulin G, antibodies. Based on these findings, the patient was diagnosed with HZO. Further, the patient received antiviral treatment with famciclovir. The lesions gradually improved with conservative treatment and became almost unrecognizable. Therefore, HZO should be considered when there is an unexplained skin lesion at the nasal tip in patients with history of rhinoplasty.
Keyword
Figure
Reference
-
1. Insinga RP, Itzler RF, Pellissier JM, Saddier P, Nikas AA. The incidence of herpes zoster in a United States administrative database. J Gen Intern Med. 2005; 20(8):748–53.2. Li A, Tandon A, Dinkin M, Oliveira C. The use of systemic steroids in the treatment of herpes zoster ophthalmicus-related ophthalmoplegia: case report and case meta-analysis. Am J Ophthalmol. 2021; (223):241–5.3. Frary J, Petersen PT, Pareek M. Hutchinson’s sign of ophthalmic zoster. Clin Case Rep. 2020; 8(1):219–20.4. Ragozzino MW, Melton LJ 3rd, Kurland LT, Chu CP, Perry HO. Population-based study of herpes zoster and its sequelae. Medicine (Baltimore). 1982; 61(5):310–6.5. Liesegang TJ. Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology. 2008; 115(2 Suppl):S3–12.6. Gershon AA, Steinberg SP, Borkowsky W, Lennette D, Lennette E. IgM to varicella-zoster virus: demonstration in patients with and without clinical zoster. Pediatr Infect Dis. 1982; 1(3):164–7.7. Davis AR, Sheppard J. Herpes zoster ophthalmicus review and prevention. Eye Contact Lens. 2019; 45(5):286–91.8. Keyhan SO, Ramezanzade S, Yazdi RG, Valipour MA, Fallahi HR, Shakiba M, et al. Prevalence of complications associated with polymer-based alloplastic materials in nasal dorsal augmentation: a systematic review and meta-analysis. Maxillofac Plast Reconstr Surg. 2022; 44(1):17.9. Marsh RJ, Cooper M. Oral acyclovir in acute herpes zoster. Br Med J (Clin Res Ed). 1987; 294(6573):704.10. Balfour HH Jr. Varicella zoster virus infections in immunocompromised hosts. A review of the natural history and management. Am J Med. 1988; 85(2A):68–73.11. Johnson JL, Amzat R, Martin N. Herpes zoster ophthalmicus. Prim Care. 2015; 42(3):285–303.12. Vrcek I, Choudhury E, Durairaj V. Herpes zoster ophthalmicus: a review for the internist. Am J Med. 2017; 130(1):21–6.13. Yawn BP, Wollan PC, St Sauver JL, Butterfield LC. Herpes zoster eye complications: rates and trends. Mayo Clin Proc. 2013; 88(6):562–70.14. Shrestha M, Chen A. Modalities in managing postherpetic neuralgia. Korean J Pain. 2018; 31(4):235–43.15. Kalogeropoulos CD, Bassukas ID, Moschos MM, Tabbara KF. Eye and periocular skin involvement in herpes zoster infection. Med Hypothesis Discov Innov Ophthalmol. 2015; 4(4):142–56.