Intest Res.
2022 Jul;20(3):350-360. 10.5217/ir.2021.00049.
Clinical outcomes and predictors of response for adalimumab in patients with moderately to severely active ulcerative colitis: a KASID prospective multicenter cohort study
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine and Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Gastroenterology, Kyung Hee University Hospital, Seoul, Korea
- 5Department of Gastroenterology, The Catholic University of Korea St. Vincent’s Hospital, Suwon, Korea
- 6Department of Gastroenterology, SMG-SNU Boramae Medical Center, Seoul, Korea
- 7Department of Gastroenterology, Ewha Womans University College of Medicine, Seoul, Korea
- 8Department of Internal Medicine, Chosun University College of Medicine, Gwangju, Korea
- 9Department of Internal Medicine, Daejeon St. Mary’s Hospital, The Catholic University of Korea College of Medicine, Daejeon, Korea
- 10Department of Gastroenterology, Ajou University School of Medicine, Suwon, Korea
- 11Department of Gastroenterology, Korea University Anam Hospital, Seoul, Korea
- 12Department of Gastroenterology, Inje University Seoul Paik Hospital, Seoul, Korea
- 13Department of Gastroenterology, Inje University Haeundae Paik Hospital, Busan, Korea
- 14Department of Gastroenterology, Chonnam National University Hospital, Gwangju, Korea
- 15Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 16Department of Gastroenterology, Inha University Hospital, Incheon, Korea
- 17Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 18Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 19AbbVie Ltd., Seoul, Korea
- 20AbbVie Pte. Ltd., Singapore
- 21Department of Microbiology, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2531989
- DOI: http://doi.org/10.5217/ir.2021.00049
Abstract
- Background/Aims
This study assessed the efficacy and safety of adalimumab (ADA) and explored predictors of response in Korean patients with ulcerative colitis (UC).
Methods
A prospective, observational, multicenter study was conducted over 56 weeks in adult patients with moderately to severely active UC who received ADA. Clinical response, remission, and mucosal healing were assessed using the Mayo score.
Results
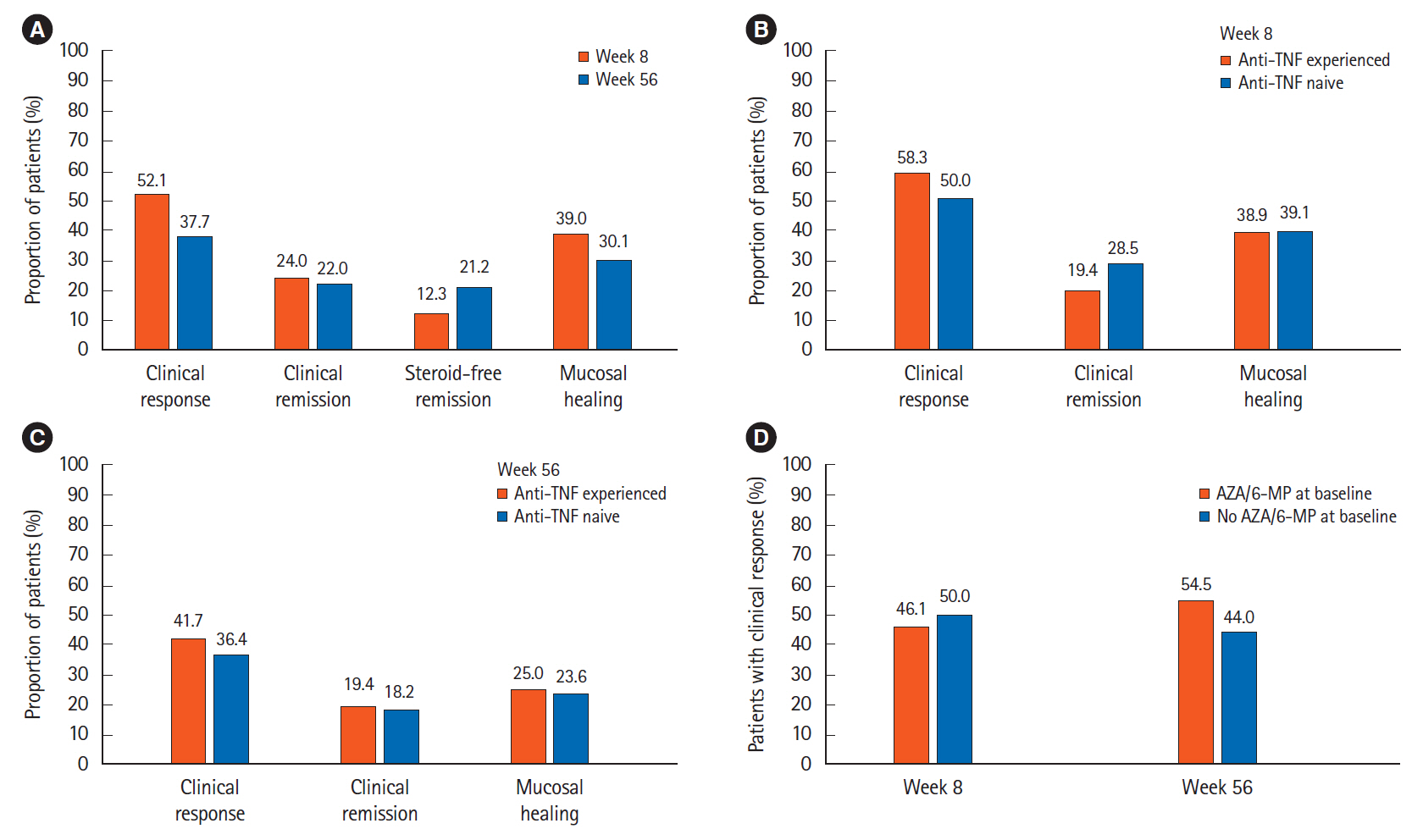
A total of 146 patients were enrolled from 17 academic hospitals. Clinical response rates were 52.1% and 37.7% and clinical remission rates were 24.0% and 22.0% at weeks 8 and 56, respectively. Mucosal healing rates were 39.0% and 30.1% at weeks 8 and 56, respectively. Prior use of anti-tumor necrosis factor-α (anti-TNF-α) did not affect clinical and endoscopic responses. The ADA drug level was significantly higher in patients with better outcomes at week 8 (P<0.05). In patients with lower endoscopic activity, higher body mass index, and higher serum albumin levels at baseline, the clinical response rate was higher at week 8. In patients with lower Mayo scores and C-reactive protein levels, clinical responses, and mucosal healing at week 8, the clinical response rate was higher at week 56. Serious adverse drug reactions were identified in 2.8% of patients.
Conclusions
ADA is effective and safe for induction and maintenance in Korean patients with UC, regardless of prior anti-TNF-α therapy. The ADA drug level is associated with the efficacy of induction therapy. Patients with better short-term outcomes were predictive of those with an improved long-term response.
Figure
Cited by 2 articles
-
Korean clinical practice guidelines on biologics and small molecules for moderate-to-severe ulcerative colitis
Soo-Young Na, Chang Hwan Choi, Eun Mi Song, Ki Bae Bang, Sang Hyoung Park, Eun Soo Kim, Jae Jun Park, Bora Keum, Chang Kyun Lee, Bo-In Lee, Seung-Bum Ryoo, Seong-Joon Koh, Miyoung Choi, Joo Sung Kim
Intest Res. 2023;21(1):61-87. doi: 10.5217/ir.2022.00007.Reviewing not Homer’s
Iliad , but “Kai Bao Ben Cao ”: indigo dye—the past, present, and future
Yusuke Yoshimatsu, Tomohisa Sujino, Takanori Kanai
Intest Res. 2023;21(2):174-176. doi: 10.5217/ir.2022.00018.
Reference
-
1. Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011; 365:1713–1725.
Article2. Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011; 140:1785–1794.
Article3. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.
Article4. Loftus CG, Loftus EV Jr, Harmsen WS, et al. Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940-2000. Inflamm Bowel Dis. 2007; 13:254–261.
Article5. Yang SK, Loftus EV Jr, Sandborn WJ. Epidemiology of inflammatory bowel disease in Asia. Inflamm Bowel Dis. 2001; 7:260–270.
Article6. Lakatos PL. Recent trends in the epidemiology of inflammatory bowel diseases: up or down? World J Gastroenterol. 2006; 12:6102–6108.
Article7. Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016; 14:111–119.
Article8. Yen HH, Weng MT, Tung CC, et al. Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study. Intest Res. 2019; 17:54–62.
Article9. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280.
Article10. Jung YS, Han M, Kim WH, Park S, Cheon JH. Incidence and clinical outcomes of inflammatory bowel disease in South Korea, 2011-2014: a nationwide population-based study. Dig Dis Sci. 2017; 62:2102–2112.
Article11. Park SH, Kim YJ, Rhee KH, et al. A 30-year trend analysis in the epidemiology of inflammatory bowel disease in the Songpa-Kangdong district of Seoul, Korea in 1986-2015. J Crohns Colitis. 2019; 13:1410–1417.
Article12. Lee JH, Cheon JH, Kim ES, et al. The prevalence and clinical significance of perinuclear anti-neutrophil cytoplasmic antibody in Korean patients with ulcerative colitis. Dig Dis Sci. 2010; 55:1406–1412.
Article13. Park SH, Kim YM, Yang SK, et al. Clinical features and natural history of ulcerative colitis in Korea. Inflamm Bowel Dis. 2007; 13:278–283.
Article14. Sandborn WJ, van Assche G, Reinisch W, et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2012; 142:257–265.
Article15. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629.
Article16. Reinisch W, Sandborn WJ, Hommes DW, et al. Adalimumab for induction of clinical remission in moderately to severely active ulcerative colitis: results of a randomised controlled trial. Gut. 2011; 60:780–787.
Article17. Suzuki Y, Motoya S, Hanai H, et al. Efficacy and safety of adalimumab in Japanese patients with moderately to severely active ulcerative colitis. J Gastroenterol. 2014; 49:283–294.
Article18. Muñoz-Villafranca C, Ortiz de Zarate J, Arreba P, et al. Adalimumab treatment of anti-TNF-naïve patients with ulcerative colitis: deep remission and response factors. Dig Liver Dis. 2018; 50:812–819.
Article19. Bálint A, Farkas K, Palatka K, et al. Efficacy and safety of adalimumab in ulcerative colitis refractory to conventional therapy in routine clinical practice. J Crohns Colitis. 2016; 10:26–30.
Article20. Dulai PS, Siegel CA, Colombel JF, Sandborn WJ, Peyrin-Biroulet L. Systematic review: monotherapy with antitumour necrosis factor α agents versus combination therapy with an immunosuppressive for IBD. Gut. 2014; 63:1843–1853.
Article21. Taxonera C, Iglesias E, Muñoz F, et al. Adalimumab maintenance treatment in ulcerative colitis: outcomes by prior antiTNF use and efficacy of dose escalation. Dig Dis Sci. 2017; 62:481–490.
Article22. Hussey M, Mc Garrigle R, Kennedy U, et al. Long-term assessment of clinical response to adalimumab therapy in refractory ulcerative colitis. Eur J Gastroenterol Hepatol. 2016; 28:217–221.
Article23. Colombel JF, Jharap B, Sandborn WJ, et al. Effects of concomitant immunomodulators on the pharmacokinetics, efficacy and safety of adalimumab in patients with Crohn’s disease or ulcerative colitis who had failed conventional therapy. Aliment Pharmacol Ther. 2017; 45:50–62.
Article24. Matsumoto T, Motoya S, Watanabe K, et al. Adalimumab monotherapy and a combination with azathioprine for Crohn’s disease: a prospective, randomized trial. J Crohns Colitis. 2016; 10:1259–1266.
Article25. Harper JW, Sinanan MN, Zisman TL. Increased body mass index is associated with earlier time to loss of response to infliximab in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013; 19:2118–2124.
Article26. Dahiya DS, Kichloo A, Wani F, Singh J, Solanki D, Shaka H. A nationwide analysis on the influence of obesity in inflammatory bowel disease hospitalizations. Intest Res. 20:342–349.
Article27. Henriksen M, Jahnsen J, Lygren I, et al. C-reactive protein: a predictive factor and marker of inflammation in inflammatory bowel disease: results from a prospective population-based study. Gut. 2008; 57:1518–1523.
Article28. Iwasa R, Yamada A, Sono K, Furukawa R, Takeuchi K, Suzuki Y. C-reactive protein level at 2 weeks following initiation of infliximab induction therapy predicts outcomes in patients with ulcerative colitis: a 3 year follow-up study. BMC Gastroenterol. 2015; 15:103.
Article29. Con D, Andrew B, Nicolaides S, van Langenberg DR, Vasudevan A. Biomarker dynamics during infliximab salvage for acute severe ulcerative colitis: C-reactive protein (CRP)-lymphocyte ratio and CRP-albumin ratio are useful in predicting colectomy. Intest Res. 2022; 20:101–113.
Article30. Ardizzone S, Cassinotti A, Duca P, et al. Mucosal healing predicts late outcomes after the first course of corticosteroids for newly diagnosed ulcerative colitis. Clin Gastroenterol Hepatol. 2011; 9:483–489.
Article31. Lee KM, Jeen YT, Cho JY, et al. Efficacy, safety, and predictors of response to infliximab therapy for ulcerative colitis: a Korean multicenter retrospective study. J Gastroenterol Hepatol. 2013; 28:1829–1833.
Article32. Italian Group for the Study of Inflammatory Bowel Disease, Armuzzi A, Biancone L, et al. Adalimumab in active ulcerative colitis: a “real-life” observational study. Dig Liver Dis. 2013; 45:738–743.
Article33. Taxonera C, Estellés J, Fernández-Blanco I, et al. Adalimumab induction and maintenance therapy for patients with ulcerative colitis previously treated with infliximab. Aliment Pharmacol Ther. 2011; 33:340–348.
Article34. Van de Vondel S, Baert F, Reenaers C, et al. Incidence and predictors of success of adalimumab dose escalation and de-escalation in ulcerative colitis: a real-world Belgian cohort study. Inflamm Bowel Dis. 2018; 24:1099–1105.
Article35. Wolf D, D’Haens G, Sandborn WJ, et al. Escalation to weekly dosing recaptures response in adalimumab-treated patients with moderately to severely active ulcerative colitis. Aliment Pharmacol Ther. 2014; 40:486–497.
Article36. Lin WC, Wong JM, Tung CC, et al. Fecal calprotectin correlated with endoscopic remission for Asian inflammatory bowel disease patients. World J Gastroenterol. 2015; 21:13566–13573.
Article37. Lee SH, Kim MJ, Chang K, et al. Fecal calprotectin predicts complete mucosal healing and better correlates with the ulcerative colitis endoscopic index of severity than with the Mayo endoscopic subscore in patients with ulcerative colitis. BMC Gastroenterol. 2017; 17:110.38. Kristensen V, Røseth A, Ahmad T, Skar V, Moum B. Fecal calprotectin: a reliable predictor of mucosal healing after treatment for active ulcerative colitis. Gastroenterol Res Pract. 2017; 2017:2098293.
Article39. Yarur AJ, Jain A, Hauenstein SI, et al. Higher adalimumab levels are associated with histologic and endoscopic remission in patients with Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis. 2016; 22:409–415.
Article40. Bodini G, Giannini EG, Savarino V, et al. Adalimumab trough serum levels and anti-adalimumab antibodies in the long-term clinical outcome of patients with Crohn’s disease. Scand J Gastroenterol. 2016; 51:1081–1086.
Article41. Paul S, Moreau AC, Del Tedesco E, et al. Pharmacokinetics of adalimumab in inflammatory bowel diseases: a systematic review and meta-analysis. Inflamm Bowel Dis. 2014; 20:1288–1295.42. Papamichael K, Baert F, Tops S, et al. Post-induction adalimumab concentration is associated with short-term mucosal healing in patients with ulcerative colitis. J Crohns Colitis. 2017; 11:53–59.
Article43. Ogata H, Hagiwara T, Kawaberi T, Kobayashi M, Hibi T. Safety and effectiveness of adalimumab in the treatment of ulcerative colitis: results from a large-scale, prospective, multicenter, observational study. Intest Res. 2021; 19:419–429.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Understanding the Role of Adalimumab in the Treatment of Moderately to Severely Active Ulcerative Colitis
- Reversible Corpus Callosal Lesions Associated with the Use of Adalimumab for Ulcerative Colitis
- Efficacy and Safety of Adalimumab in Moderately to Severely Active Cases of Ulcerative Colitis: A Meta-Analysis of Published Placebo-Controlled Trials
- Long-term Outcomes of Adalimumab Therapy in Korean Patients with Ulcerative Colitis: A Hospital-Based Cohort Study
- Biologics for the treatment of pyoderma gangrenosum in ulcerative colitis