Child Kidney Dis.
2022 Jun;26(1):52-57. 10.3339/ckd.22.019.
Predictors of renal scars in infants with recurrent febrile urinary tract infection: a retrospective, single-center study
- Affiliations
-
- 1Department of Pediatrics, CHA Bundang Medical Center, CHA University, Seongnam, Republic of Korea
- KMID: 2531935
- DOI: http://doi.org/10.3339/ckd.22.019
Abstract
- Purpose
To determine predictive factors for detecting renal parenchymal damages (RPDs) in infants with recurrent febrile urinary tract infection (fUTI).
Methods
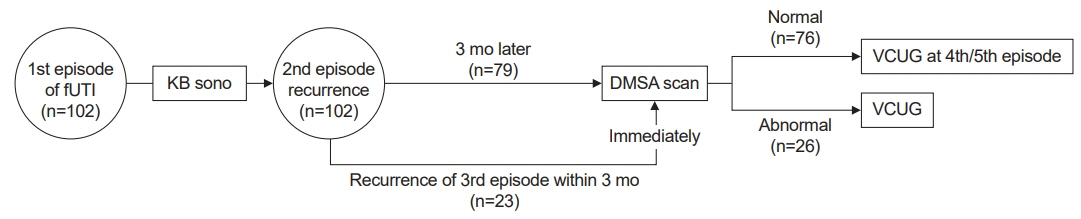
From January 2015 to December 2021, 102 infants with recurrent fUTI and who underwent 99mTc-dimercaptosuccinic acid (DMSA) renal scan in our hospital were included in this study. Controls included infants with normal DMSA results performed 3 months apart from the 2nd episode of fUTI. DMSA-positive group included infants with positive DMSA results performed 3 months apart from the 2nd episode of fUTI or at the 3rd episode of fUTI. The recurrence rate, causative bacteria, renal size discrepancy of both kidneys, and laboratory findings including C-reactive protein (CRP) and spot urine sodium-to-potassium ratio (uNa/K) were compared between both groups.
Results
Only 3.8% of 79 infants with a 2nd episode of fUTI showed positive DMSA results. fUTI recurred more frequently within 12 months of follow-up in the DMSA-positive group than in the control group (69% vs. 13%, P=0.00). CRP values were significantly higher in the DMSA-positive group than in the control group (7.3 mg/dL vs. 3.7 mg/dL, P=0.00). Spot uNa/K were significantly lower in the DMSA-positive group than in the control group (0.6 vs. 1.1, P=0.00).
Conclusions
Congenital renal scar and RPDs on the DMSA scan were more frequently found in infants with recurrent fUTI than those in the control group. High CRP values and low spot uNa/K in acute infections were helpful in predicting the presence of RPD in infants with recurrent fUTI.
Keyword
Figure
Reference
-
References
1. Chang SL, Shortliffe LD. Pediatric urinary tract infections. Pediatr Clin North Am. 2006; 53:379–400.
Article2. Scott Wang HH, Cahill D, Panagides J, Logvinenko T, Nelson C. Top-down versus bottom-up approach in children presenting with urinary tract infection: comparative effectiveness analysis using RIVUR and CUTIE data. J Urol. 2021; 206:1284–90.
Article3. O'Reilly SE, Plyku D, Sgouros G, Fahey FH, Ted Treves S, Frey EC, et al. A risk index for pediatric patients undergoing diagnostic imaging with (99m)Tc-dimercaptosuccinic acid that accounts for body habitus. Phys Med Biol. 2016; 61:2319–32.4. Subcommittee on Urinary Tract Infection; Steering Committee on Quality Improvement and Management, Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011; 128:595–610.
Article5. Cain JE, Di Giovanni V, Smeeton J, Rosenblum ND. Genetics of renal hypoplasia: insights into the mechanisms controlling nephron endowment. Pediatr Res. 2010; 68:91–8.
Article6. Bonsib SM. Renal hypoplasia, from grossly insufficient to not quite enough: consideration for expanded concepts based upon the author's perspective with historical review. Adv Anat Pathol. 2020; 27:311–30.
Article7. Abdelhalim A, Khoury AE. Critical appraisal of the top-down approach for vesicoureteral reflux. Investig Clin Urol. 2017; 58(Suppl 1):S14–22.
Article8. Al Qahtani W, Sarhan O, Al Otay A, El Helaly A, Al Kawai F. Primary bilateral high-grade vesicoureteral reflux in children: management perspective. Cureus. 2020; 12:e12266.
Article9. Lee JH, Rhie S. Reconsideration of urine culture for the diagnosis of acute pyelonephritis in children: a new challenging method for diagnosing acute pyelonephritis. Korean J Pediatr. 2019; 62:433–7.
Article10. Park YS. Renal scar formation after urinary tract infection in children. Korean J Pediatr. 2012; 55:367–70.
Article11. Leroy S, Fernandez-Lopez A, Nikfar R, Romanello C, Bouissou F, Gervaix A, et al. Association of procalcitonin with acute pyelonephritis and renal scars in pediatric UTI. Pediatrics. 2013; 131:870–9.
Article12. Soylu A, Demir BK, Turkmen M, Bekem O, Saygi M, Cakmakci H, et al. Predictors of renal scar in children with urinary infection and vesicoureteral reflux. Pediatr Nephrol. 2008; 23:2227–32.
Article13. Becerir T, Yuksel S, Evrengul H, Ergin A, Enli Y. Urinary excretion of pentraxin-3 correlates with the presence of renal scar following acute pyelonephritis in children. Int Urol Nephrol. 2019; 51:571–7.
Article14. Lee JH, Yim HE, Yoo KH. Associations of plasma neutrophil gelatinase-associated lipocalin, anemia, and renal scarring in children with febrile urinary tract infections. J Korean Med Sci. 2020; 35:e65.
Article15. Gokce I, Alpay H, Biyikli N, Unluguzel G, Dede F, Topuzoglu A. Urinary levels of interleukin-6 and interleukin-8 in patients with vesicoureteral reflux and renal parenchymal scar. Pediatr Nephrol. 2010; 25:905–12.
Article16. Jung SJ, Lee JH. Prediction of cortical defect using C-reactive protein and urine sodium to potassium ratio in infants with febrile urinary tract infection. Yonsei Med J. 2016; 57:103–10.
Article17. Lee JH. Discrimination of culture negative pyelonephritis in children with suspected febrile urinary tract infection and negative urine culture results. J Microbiol Immunol Infect. 2019; 52:598–603.
Article18. Lee JH, Jang SJ, Rhie S. Antinatriuretic phenomena seen in children with acute pyelonephritis may be related to the activation of intrarenal RAAS. Medicine (Baltimore). 2018; 97:e12152.
Article19. Kosmeri C, Kalaitzidis R, Siomou E. An update on renal scarring after urinary tract infection in children: what are the risk factors? J Pediatr Urol. 2019; 15:598–603.
Article20. Shaikh N, Craig JC, Rovers MM, Da Dalt L, Gardikis S, Hoberman A, et al. Identification of children and adolescents at risk for renal scarring after a first urinary tract infection: a meta-analysis with individual patient data. JAMA Pediatr. 2014; 168:893–900.
Article21. Rodriguez LM, Robles B, Marugan JM, Suarez A, Garcia Ruiz de Morales JM. Do serum C-reactive protein and interleukin-6 predict kidney scarring after urinary tract infection? Indian J Pediatr. 2013; 80:1002–6.
Article22. Bressan S, Andreola B, Zucchetta P, Montini G, Burei M, Perilongo G, et al. Procalcitonin as a predictor of renal scarring in infants and young children. Pediatr Nephrol. 2009; 24:1199–204.
Article23. Warady BA, Chadha V. Chronic kidney disease in children: the global perspective. Pediatr Nephrol. 2007; 22:1999–2009.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Febrile Urinary Tract Infection in Infants Less than Two Months of Age : Characteristics and Factors Related to the Recurrence
- Factors associated with Renal Scarring in Children with a First Episode of Febrile Urinary Tract Infection
- The Relationship between Thymic Size and Vesicoureteral Reflux in Infants with Febrile Urinary Tract Infection
- Urinary Tract Infection in Febrile Infants
- Clinical Experiences with Febrile Infants, Younger than Three Months, with Urinary Tract Infection in a Single Center for Four Years: Incidence, Pathogens and Viral Co-infections