Arch Hand Microsurg.
2022 Jun;27(2):105-118. 10.12790/ahm.21.0149.
Ulnar impaction syndrome: how to diagnose and treat?
- Affiliations
-
- 1Department of Orthopedic Surgery, Armed Forces Yangju Hospital, Yangju, Korea
- 2Department of Orthopedic Surgery, Korea University, Anam Hospital, Seoul, Korea
- 3Department of Orthopedic Surgery, Korea University, Ansan Hospital, Ansan, Korea
- KMID: 2531916
- DOI: http://doi.org/10.12790/ahm.21.0149
Abstract
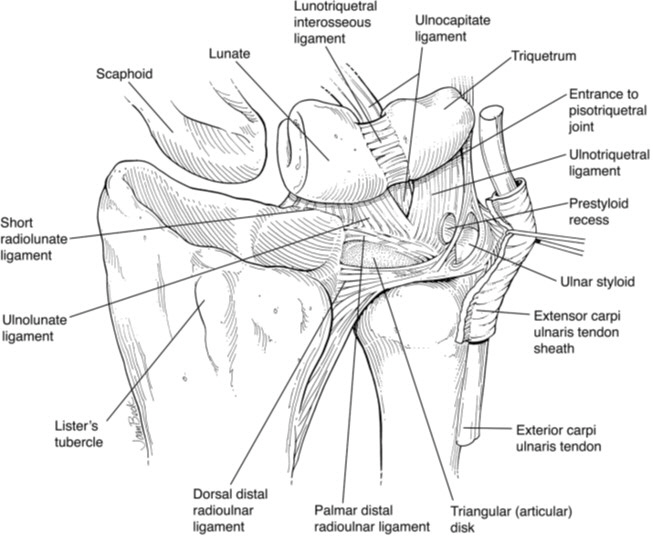
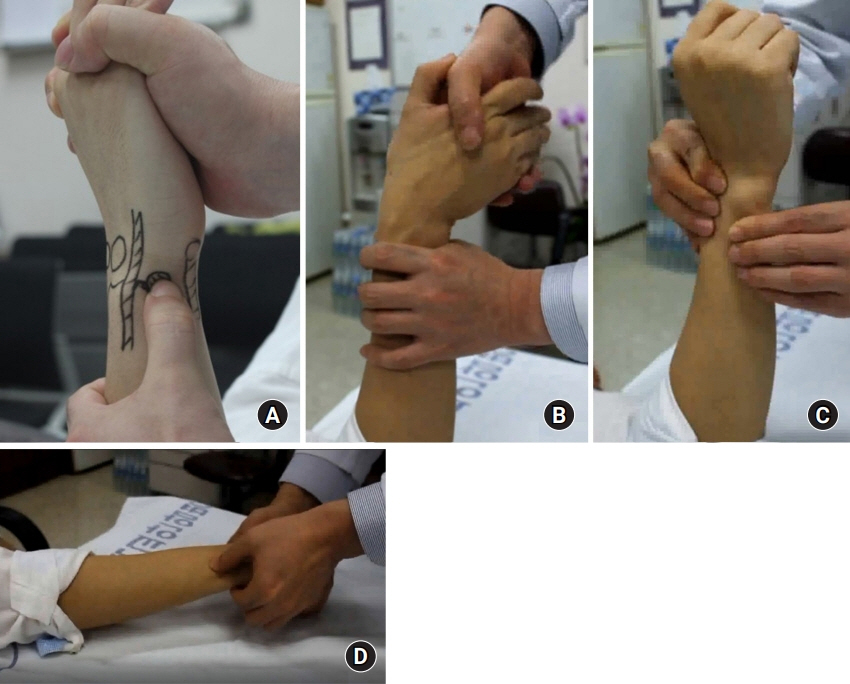
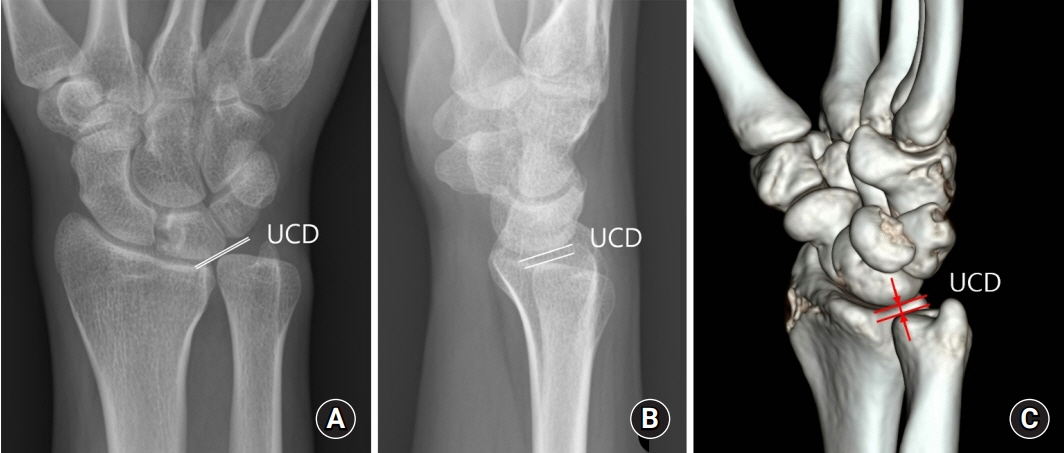
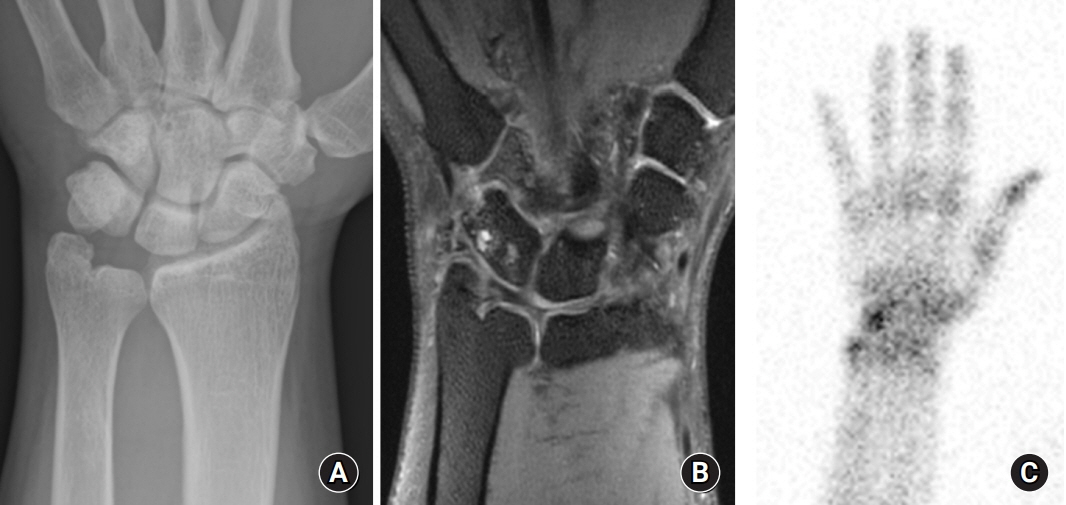
- Ulnar impaction syndrome (UIS), also called ulnocarpal abutment syndrome, is a degenerative condition induced by repeated loads on the ulnocarpal joint and is a representative cause of ulnar-sided wrist pain. Because of the small, complex, and overlapping anatomy of the ulnar wrist, ulnar wrist pathologies often present very similar symptoms to those of UIS, which causes confusion in diagnosing UIS. Thus, careful history-taking, clinical examinations, and diagnostic imaging are essential for the diagnosis of UIS. As appropriate and effective treatment for UIS, early surgical treatment should be considered if patients cannot reduce their wrist usage in daily living and work and have distal radioulnar instability. There are various surgical techniques for UIS. Surgeons should be deliberate in choosing a technique and pay attention to accompanying disorders around the ulnar wrist to achieve satisfactory treatment outcomes.
Keyword
Figure
Reference
-
References
1. Leibig N, Lampert FM, Haerle M. Ulnocarpal impaction. Hand Clin. 2021; 37:553–62.
Article2. Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Kim HH. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. J Bone Joint Surg Am. 2005; 87:2649–54.
Article3. Kim J, Gong HS, Baek GH. Updates on ulnar impaction syndrome. J Korean Orthop Assoc. 2017; 52:103–11.
Article4. Tomaino MM. Ulnar impaction syndrome in the ulnar negative and neutral wrist: diagnosis and pathoanatomy. J Hand Surg Br. 1998; 23:754–7.5. Shin AY, Deitch MA, Sachar K, Boyer MI. Ulnar-sided wrist pain: diagnosis and treatment. Instr Course Lect. 2005; 54:115–28.6. Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2012; 37:1489–500.
Article7. Zahiri H, Zahiri CA, Ravari FK. Ulnar styloid impingement syndrome. Int Orthop. 2010; 34:1233–7.
Article8. Topper SM, Wood MB, Ruby LK. Ulnar styloid impaction syndrome. J Hand Surg Am. 1997; 22:699–704.
Article9. Friedman SL, Palmer AK. The ulnar impaction syndrome. Hand Clin. 1991; 7:295–310.
Article10. Sammer DM, Rizzo M. Ulnar impaction. Hand Clin. 2010; 26:549–57.
Article11. Vezeridis PS, Yoshioka H, Han R, Blazar P. Ulnar-sided wrist pain. Part I: anatomy and physical examination. Skeletal Radiol. 2010; 39:733–45.
Article12. Parker AS, Nguyen M, Minard CG, Guffey D, Willis MH, Reichel LM. Measurement of ulnar variance from the lateral radiograph: a comparison of techniques. J Hand Surg Am. 2014; 39:1114–21.
Article13. Nakamura R, Horii E, Imaeda T, Nakao E, Kato H, Watanabe K. The ulnocarpal stress test in the diagnosis of ulnar-sided wrist pain. J Hand Surg Br. 1997; 22:719–23.
Article14. Skirven T. Clinical examination of the wrist. J Hand Ther. 1996; 9:96–107.
Article15. Tomaino MM. The importance of the pronated grip X-ray view in evaluating ulnar variance. J Hand Surg Am. 2000; 25:352–7.
Article16. Yeh GL, Beredjiklian PK, Katz MA, Steinberg DR, Bozentka DJ. Effects of forearm rotation on the clinical evaluation of ulnar variance. J Hand Surg Am. 2001; 26:1042–6.
Article17. Shin AY, Battaglia MJ, Bishop AT. Lunotriquetral instability: diagnosis and treatment. J Am Acad Orthop Surg. 2000; 8:170–9.
Article18. Baek GH, Lee HJ, Gong HS, et al. Long-term outcomes of ulnar shortening osteotomy for idiopathic ulnar impaction syndrome: at least 5-years follow-up. Clin Orthop Surg. 2011; 3:295–301.
Article19. Shin SH, Lee YS, Choi KY, Kwak DS, Chung YG. During forearm rotation the three-dimensional ulnolunate distance is affected more by translation of the ulnar head than change in ulnar variance. J Hand Surg Eur Vol. 2019; 44:517–23.
Article20. Hayter CL, Gold SL, Potter HG. Magnetic resonance imaging of the wrist: bone and cartilage injury. J Magn Reson Imaging. 2013; 37:1005–19.
Article21. Cerezal L, del Piñal F, Abascal F, García-Valtuille R, Pereda T, Canga A. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics. 2002; 22:105–21.
Article22. Imaeda T, Nakamura R, Shionoya K, Makino N. Ulnar impaction syndrome: MR imaging findings. Radiology. 1996; 201:495–500.
Article23. Honcharuk E, Monica J. Complications associated with intra-articular and extra-articular corticosteroid injections. JBJS Rev. 2016; 4:e2.
Article24. Nunez FA Jr, Barnwell J, Li Z, Nunez FA Sr. Metaphyseal ulnar shortening osteotomy for the treatment of ulnocarpal abutment syndrome using distal ulna hook plate: case series. J Hand Surg Am. 2012; 37:1574–9.
Article25. McBeath R, Katolik LI, Shin EK. Ulnar shortening osteotomy for ulnar impaction syndrome. J Hand Surg Am. 2013; 38:379–81.
Article26. Griska A, Feldon P. Wafer resection of the distal ulna. J Hand Surg Am. 2015; 40:2283–8.
Article27. Aibinder WR, Izadpanah A, Elhassan BT. Ulnar shortening versus distal radius corrective osteotomy in the management of ulnar impaction after distal radius malunion. Hand (N Y). 2018; 13:194–201.
Article28. Lautenbach M, Millrose M, Schmidt NS, Zach A, Eichenauer F, Eisenschenk A. Ulnocarpal impaction syndrome: treatment with a transverse ulnar shortening osteotomy from an ulnodorsal approach. Arch Orthop Trauma Surg. 2014; 134:881–5.
Article29. Milch H. Dislocation of the inferior end of the ulna: suggestion for a new operative procedure. Am J Surg. 1926; 1:141–6.30. Cha SM, Shin HD. Distal radioulnar joint arthritis. J Korean Orthop Assoc. 2017; 52:125–37.
Article31. Arimitsu S, Moritomo H, Kitamura T, et al. The stabilizing effect of the distal interosseous membrane on the distal radioulnar joint in an ulnar shortening procedure: a biomechanical study. J Bone Joint Surg Am. 2011; 93:2022–30.
Article32. Rajgopal R, Roth J, King G, Faber K, Grewal R. Outcomes and complications of ulnar shortening osteotomy: an institutional review. Hand (N Y). 2015; 10:535–40.
Article33. Nishiwaki M, Nakamura T, Nagura T, Toyama Y, Ikegami H. Ulnar-shortening effect on distal radioulnar joint pressure: a biomechanical study. J Hand Surg Am. 2008; 33:198–205.
Article34. Nygaard M, Nielsen NS, Bojsen-Møller F. A biomechanical evaluation of the relative load change in the joints of the wrist with ulnar shortening: a ‘handbag’ model. J Hand Surg Eur Vol. 2009; 34:724–9.
Article35. Finnigan T, Makaram N, Baumann A, Ramesh K, Mohil R, Srinivasan M. Outcomes of ulnar shortening for ulnar impaction syndrome using the 2.7 mm AO ulna shortening osteotomy system. J Hand Surg Asian Pac Vol. 2018; 23:82–9.
Article36. Marquez-Lara A, Nuñez FA Jr, Kiymaz T, Nuñez FA Sr, Li Z. Metaphyseal versus diaphyseal ulnar shortening osteotomy for treatment of ulnar impaction syndrome: a comparative study. J Hand Surg Am. 2017; 42:477.
Article37. Cha SM, Shin HD, Ahn KJ. Prognostic factors affecting union after ulnar shortening osteotomy in ulnar impaction syndrome: a retrospective case-control study. J Bone Joint Surg Am. 2017; 99:638–47.38. Feldon P, Terrono AL, Belsky MR. The “wafer” procedure. Partial distal ulnar resection. Clin Orthop Relat Res. 1992; (275):124–9.
Article39. Oh WT, Kang HJ, Chun YM, Koh IH, An HM, Choi YR. Arthroscopic wafer procedure versus ulnar shortening osteotomy as a surgical treatment for idiopathic ulnar impaction syndrome. Arthroscopy. 2018; 34:421–30.
Article40. Colantoni J, Chadderdon C, Gaston RG. Arthroscopic wafer procedure for ulnar impaction syndrome. Arthrosc Tech. 2014; 3:e123–5.
Article41. Auzias P, Delarue R, Camus EJ, Van Overstraeten L. Ulna shortening osteotomy versus arthroscopic wafer procedure in the treatment of ulnocarpal impingement syndrome. Hand Surg Rehabil. 2021; 40:156–61.
Article42. Slutsky DJ. Arthroscopic management of ulnocarpal impaction syndrome and ulnar styloid impaction syndrome. Hand Clin. 2017; 33:639–50.
Article43. Barbaric K, Rujevcan G, Labas M, Delimar D, Bicanic G. Ulnar shortening osteotomy after distal radius fracture malunion: review of literature. Open Orthop J. 2015; 9:98–106.
Article44. Wehbé MA, Cautilli DA. Ulnar shortening using the AO small distractor. J Hand Surg Am. 1995; 20:959–64.
Article45. Kang JW, Cha SM, Kim SG, Choi IC, Suh DH, Park JW. Tips and tricks to achieve osteotomy healing and prevent refracture after ulnar shortening osteotomy. J Orthop Surg Res. 2021; 16:110.
Article46. Lauder AJ, Luria S, Trumble TE. Oblique ulnar shortening osteotomy with a new plate and compression system. Tech Hand Up Extrem Surg. 2007; 11:66–73.
Article47. Firoozbakhsh K, Moneim MS, Mikola E, Haltom S. Heat generation during ulnar osteotomy with microsagittal saw blades. Iowa Orthop J. 2003; 23:46–50.48. Tolat AR, Sanderson PL, De Smet L, Stanley JK. The gymnast’s wrist: acquired positive ulnar variance following chronic epiphyseal injury. J Hand Surg Br. 1992; 17:678–81.
Article49. de Runz A, Pauchard N, Sorin T, Dap F, Dautel G. Ulna-shortening osteotomy: outcome and repercussion of the distal radioulnar joint osteoarthritis. Plast Reconstr Surg. 2016; 137:175–84.50. Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984; (187):26–35.
Article51. Hontani K, Matsui Y, Kawamura D, et al. Stress distribution pattern in the distal radioulnar joint before and after ulnar shortening osteotomy in patients with ulnar impaction syndrome. Sci Rep. 2021; 11:17891.
Article52. Moritomo H. The distal interosseous membrane: current concepts in wrist anatomy and biomechanics. J Hand Surg Am. 2012; 37:1501–7.
Article53. Orbay JL, Levaro-Pano F, Vernon LL, Cronin MH, Orbay JA, Tremols EJ. The parallelogram effect: the association between central band and positive ulnar variance. J Hand Surg Am. 2018; 43:827–32.
Article54. Megerle K, Hellmich S, Germann G, Sauerbier M. Hardware location and clinical outcome in ulna shortening osteotomy. Plast Reconstr Surg Glob Open. 2015; 3:e549.
Article55. Kitzinger HB, Karle B, Löw S, Krimmer H. Ulnar shortening osteotomy with a premounted sliding-hole plate. Ann Plast Surg. 2007; 58:636–9.
Article56. Das De S, Johnsen PH, Wolfe SW. Soft tissue complications of dorsal versus volar plating for ulnar shortening osteotomy. J Hand Surg Am. 2015; 40:928–33.
Article57. Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg Am. 1993; 18:46–53.
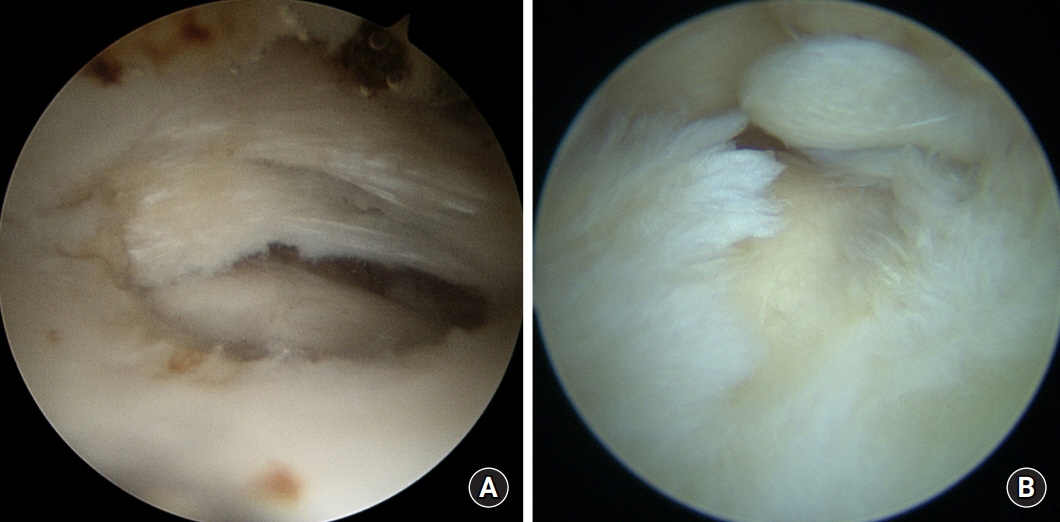
Article58. Seo JB, Kim JP, Yi HS, Park KH. The outcomes of arthroscopic repair versus debridement for chronic unstable triangular fibrocartilage complex tears in patients undergoing ulnar-shortening osteotomy. J Hand Surg Am. 2016; 41:615–23.
Article59. Kim BS, Song HS. A comparison of ulnar shortening osteotomy alone versus combined arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnar impaction syndrome. Clin Orthop Surg. 2011; 3:184–90.
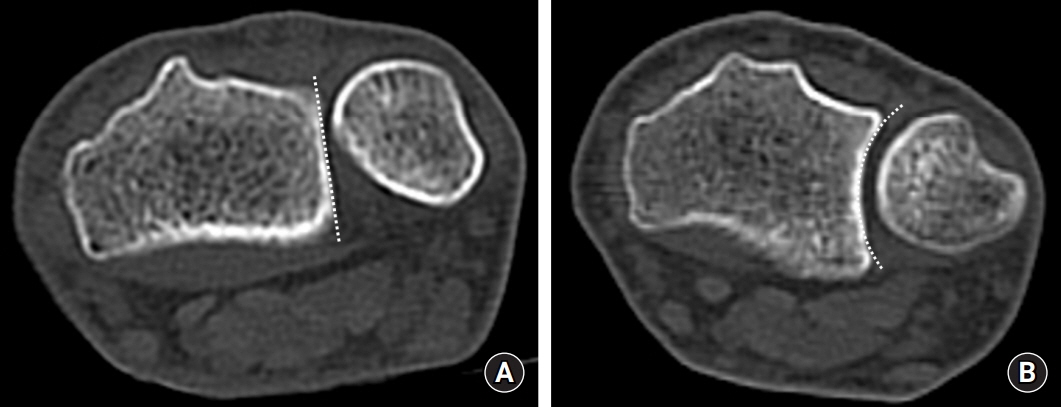
Article60. Kwon YW, Choi IC, Park JH, Nam JJ, Roh SH, Park JW. Influence of TFCC foveal tear on the location of lunate chondromalacia in ulnar impaction syndrome. Skeletal Radiol. 2021; 50:1855–61.
Article61. Iwatsuki K, Tatebe M, Yamamoto M, Shinohara T, Nakamura R, Hirata H. Ulnar impaction syndrome: incidence of lunotriquetral ligament degeneration and outcome of ulnar-shortening osteotomy. J Hand Surg Am. 2014; 39:1108–13.
Article62. Pang EQ, Yao J. Ulnar-sided wrist pain in the athlete (TFCC/DRUJ/ECU). Curr Rev Musculoskelet Med. 2017; 10:53–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroscopy of the Wrist and Ulnar Shortening Osteotomy for the Treatment of the Ulnar Impaction Syndrome
- Updates on Ulnar Impaction Syndrome
- Treatment of Ulnar Impaction Syndrome using Arthroscopy and Ulnar Shortening Osteotomy
- Intraoperative Arthroscopic Findings of Ulnar Impaction Syndrome
- Ulnar Shortening Osteotomy for the Treatment of Ulnar Impaction Syndrome