Obstet Gynecol Sci.
2022 Jul;65(4):368-375. 10.5468/ogs.22002.
Effects of high-intensity interval training and strength training on levels of testosterone and physical activity among women with polycystic ovary syndrome
- Affiliations
-
- 1Department of Health Sciences, Ziauddin University College of Rehabilitation Sciences, Karachi, Pakistan
- KMID: 2531845
- DOI: http://doi.org/10.5468/ogs.22002
Abstract
Objective
Polycystic ovary syndrome is a diverse endocrine disorder characterized by hyperandrogenism and ovulatory dysfunction. Hyperandrogenism affects body morphology, resulting in excess weight (overweight or obesity). This study aimed to evaluate the efficacy of high-intensity interval training on serum testosterone levels, body fat percentage, and level of physical activity among women with polycystic ovary syndrome.
Methods
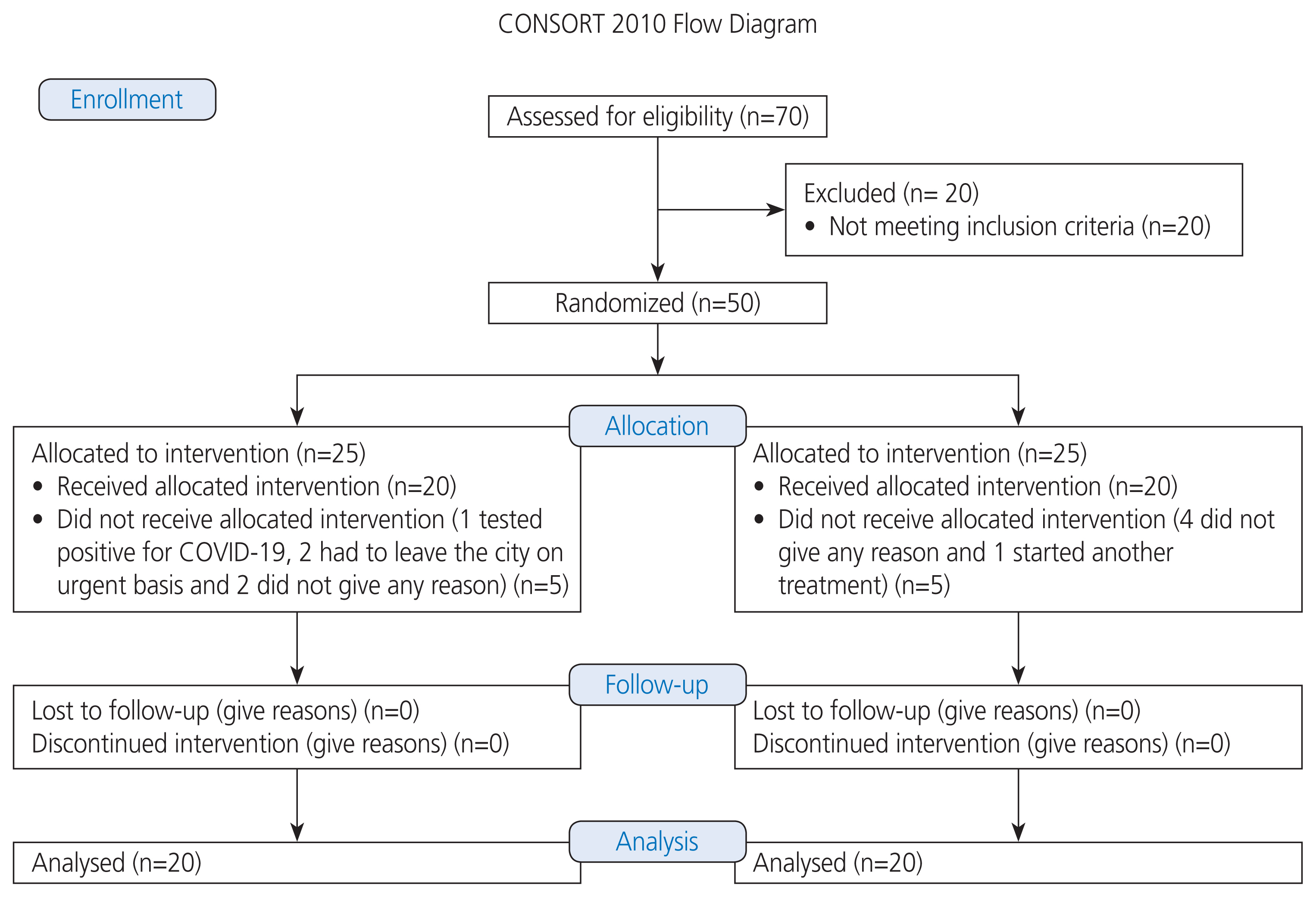
Fifty participants were enrolled in the study and randomly allocated into two groups. Group A performed highintensity interval training on alternate days per week (total of 12 weeks) and group B performed strength training on alternate days per week (total of 12 weeks). Baseline and 12th-week assessments included serum testosterone levels, body fat percentage using the skinfold method, and level of physical activity assessed using the International Physical Activity Questionnaire.
Results
After 12 weeks of intervention, both groups showed significant improvements in all the outcomes. However, group A (high intensity interval training) showed statistically significant results compared to group B (strength training) in lowering serum testosterone levels (P=0.049) and body fat percentage (P=0.001) and increasing physical activity levels (P=0.006).
Conclusion
After 12 weeks of exercise, both exercises benefited the participants; however, high-intensity interval training specifically was found to be a more effective exercise regimen than strength training in reducing serum testosterone levels and body fat percentage and enhancing levels of physical activity in women with polycystic ovary syndrome.
Figure
Reference
-
References
1. Kent J, Dodson WC, Kunselman A, Pauli J, Stone A, Diamond MP, et al. Gestational weight gain in women with polycystic ovary syndrome: a controlled study. J Clin Endocrinol Metab. 2018; 103:4315–23.
Article2. Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril. 2016; 106:6–15.
Article3. Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016; 37:467–520.
Article4. Rosenfield RL. The diagnosis of polycystic ovary syndrome in adolescents. Pediatrics. 2015; 136:1154–65.
Article5. Conway G, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Franks S, Gambineri A, ESE PCOS Special Interest Group, et al. The polycystic ovary syndrome: a position statement from the European Society of Endocrinology. Eur J Endocrinol. 2014; 171:P1–29.
Article6. Haq N, Khan Z, Riazc S, Nasim A, Shahwani R, Tahir M. Prevalence and knowledge of polycystic ovary syndrome (PCOS) among female science students of different public Universities of Quetta, Pakistan. IJIR. 2016; 3:385–92.7. Park CH, Chun S. Influence of combined oral contraceptives on polycystic ovarian morphology-related parameters in Korean women with polycystic ovary syndrome. Obstet Gynecol Sci. 2020; 63:80–6.
Article8. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018; 110:364–79.
Article9. Woodward A, Klonizakis M, Broom D. Exercise and polycystic ovary syndrome. Adv Exp Med Biol. 2020; 1228:123–36.
Article10. Zhang HY, Guo CX, Zhu FF, Qu PP, Lin WJ, Xiong J. Clinical characteristics, metabolic features, and phenotype of Chinese women with polycystic ovary syndrome: a large-scale case-control study. Arch Gynecol Obstet. 2013; 287:525–31.
Article11. Almenning I, Rieber-Mohn A, Lundgren KM, Shetelig Løvvik T, Garnæs KK, Moholdt T. Effects of high-intensity interval training and strength training on metabolic, cardiovascular and hormonal outcomes in women with polycystic ovary syndrome: a pilot study. PLoS One. 2015; 10:e0138793.12. Shele G, Genkil J, Speelman D. A systematic review of the effects of exercise on hormones in women with polycystic ovary syndrome. J Funct Morphol Kinesiol. 2020; 5:35.
Article13. Lunt H, Draper N, Marshall HC, Logan FJ, Hamlin MJ, Shearman JP, et al. High-intensity interval training in a real world setting: a randomized controlled feasibility study in overweight inactive adults, measuring change in maximal oxygen uptake. PLoS One. 2014; 9:e83256.14. Cassidy S, Thoma C, Houghton D, Trenell MI. High-intensity interval training: a review of its impact on glucose control and cardiometabolic health. Diabetologia. 2017; 60:7–23.
Article15. Hiam D, Patten R, Gibson-Helm M, Moreno-Asso A, McIlvenna L, Levinger I, et al. The effectiveness of high-intensity intermittent training on metabolic, reproductive and mental health in women with polycystic ovary syndrome: study protocol for the iHIT-randomised controlled trial. Trials. 2019; 20:221.16. Shishehgar F, Tehrani FR, Mirmiran P, Hajian S, Baghestani AR, Moslehi N. Factors influencing physical activity in women with polycystic ovary syndrome in comparison to eumenorrheic non hirsute women. Glob J Health Sci. 2016; 8:56382.
Article17. Lim JU, Lee JH, Kim JS, Hwang YI, Kim TH, Lim SY, et al. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. Int J Chron Obstruct Pulmon Dis. 2017; 12:2465–75.
Article18. Kiel IA, Lionett S, Parr EB, Jones H, Røset MAH, Salvesen Ø, et al. Improving reproductive function in women with polycystic ovary syndrome with high-intensity interval training (IMPROV-IT): study protocol for a two-centre, three-armed randomised controlled trial. BMJ Open. 2020; 10:e034733.
Article19. Abdelazim IA, Alanwar A, AbuFaza M, Amer OO, Bekmukhambetov Y, Zhurabekova G, et al. Elevated and diagnostic androgens of polycystic ovary syndrome. Prz Menopauzalny. 2020; 19:1–5.
Article20. American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 9th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health;2013.21. Moran LJ, Tassone EC, Boyle J, Brennan L, Harrison CL, Hirschberg AL, et al. Evidence summaries and recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome: lifestyle management. Obes Rev. 2020; 21:e13046.
Article22. Vizza L, Smith CA, Swaraj S, Agho K, Cheema BS. The feasibility of progressive resistance training in women with polycystic ovary syndrome: a pilot randomized controlled trial. BMC Sports Sci Med Rehabil. 2016; 8:14.
Article23. Wu X, Wu H, Sun W, Wang C. Improvement of anti-Müllerian hormone and oxidative stress through regular exercise in Chinese women with polycystic ovary syndrome. Hormones (Athens). 2021; 20:339–45.
Article24. Kirthika SV, Paul J, Selvam PS, Priya VS. Effect of aerobic exercise and life style intervention among young women with polycystic ovary syndrome. Research J Pharm Tech. 2019; 12:4269–73.
Article25. Vigorito C, Giallauria F, Palomba S, Cascella T, Manguso F, Lucci R, et al. Beneficial effects of a three-month structured exercise training program on cardiopulmonary functional capacity in young women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2007; 92:1379–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Isoflavone Supplementation on Plasma Biochemical Parameters of Women with Polycystic Ovary Syndrome
- Effect of Training Types Using Recumbent Cycle Ergometer on Ankle Strength in Healthy Male Subjects
- Obesity and Polycystic Ovary Syndrome
- Studies on Fibrinolytic System Behavior in Women with Polycystic Ovary Syndrome
- Effects of Metformin and Rosiglitazone in Overweight or Obese Women with Polycystic Ovarian Syndrome