Obstet Gynecol Sci.
2022 Jul;65(4):325-334. 10.5468/ogs.22063.
Non-invasive continuous blood pressure monitoring using the ClearSight system for pregnant women at high risks of post-partum hemorrhage: comparison with invasive blood pressure monitoring during cesarean section
- Affiliations
-
- 1Department of Obstetrics, and Gynecology, Graduate School of Medicine, Osaka Metropolitan University, Osaka, Japan
- 2Department of Anesthesiology, Graduate School of Medicine, Osaka Metropolitan University, Osaka, Japan
- KMID: 2531841
- DOI: http://doi.org/10.5468/ogs.22063
Abstract
Objective
This study aimed to investigate the accuracy and precision of continuous, non-invasive blood pressure obtained using the ClearSight system by comparing it with invasive arterial blood pressure, and to assess the hemodynamic changes using invasive methods and the ClearSight system in patients undergoing cesarean section.
Methods
Arterial pressure was measured invasively with an intra-arterial catheter and non-invasively using the ClearSight system during cesarean section in patients with placenta previa or placenta accreta. Blood pressure measurements obtained using these two means were then compared.
Results
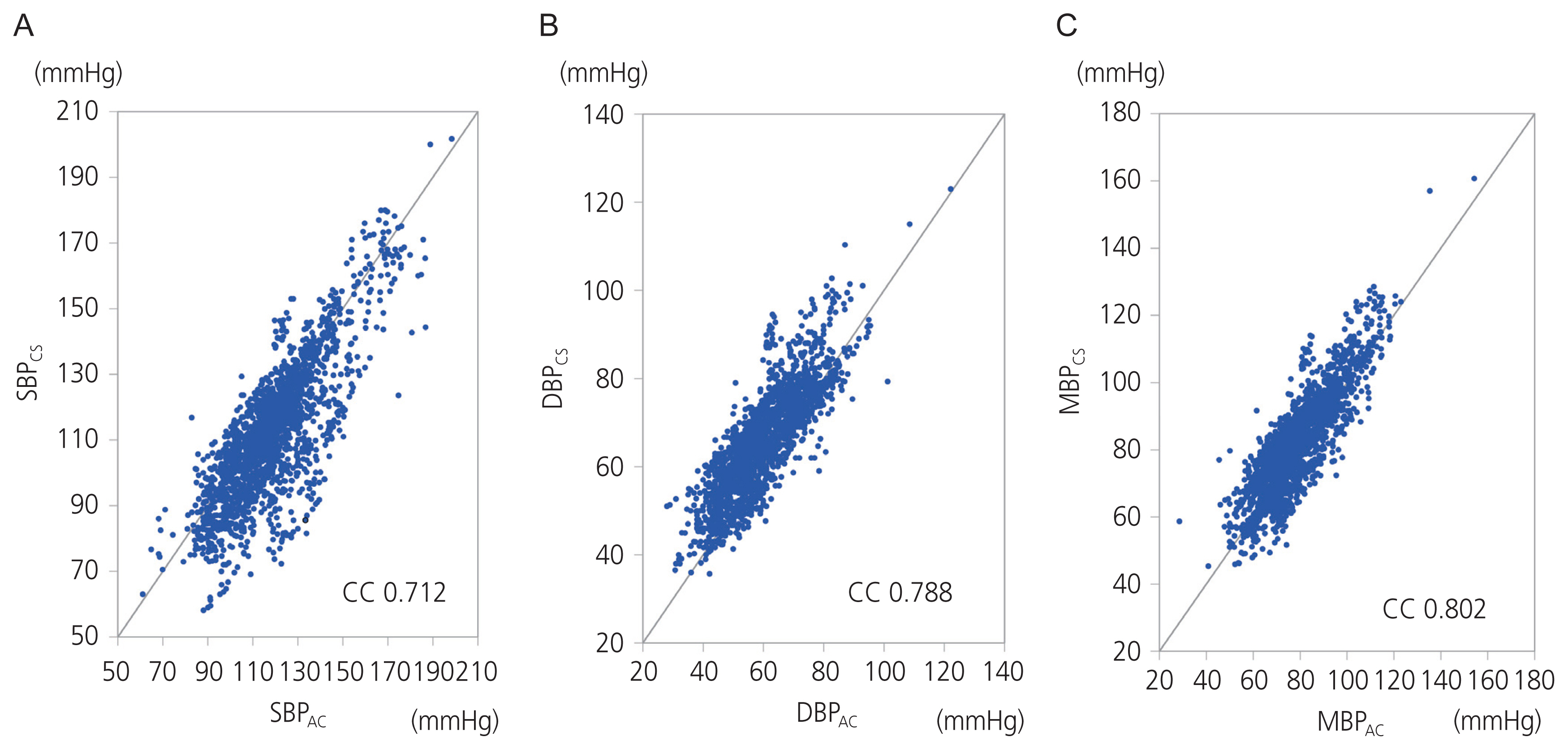
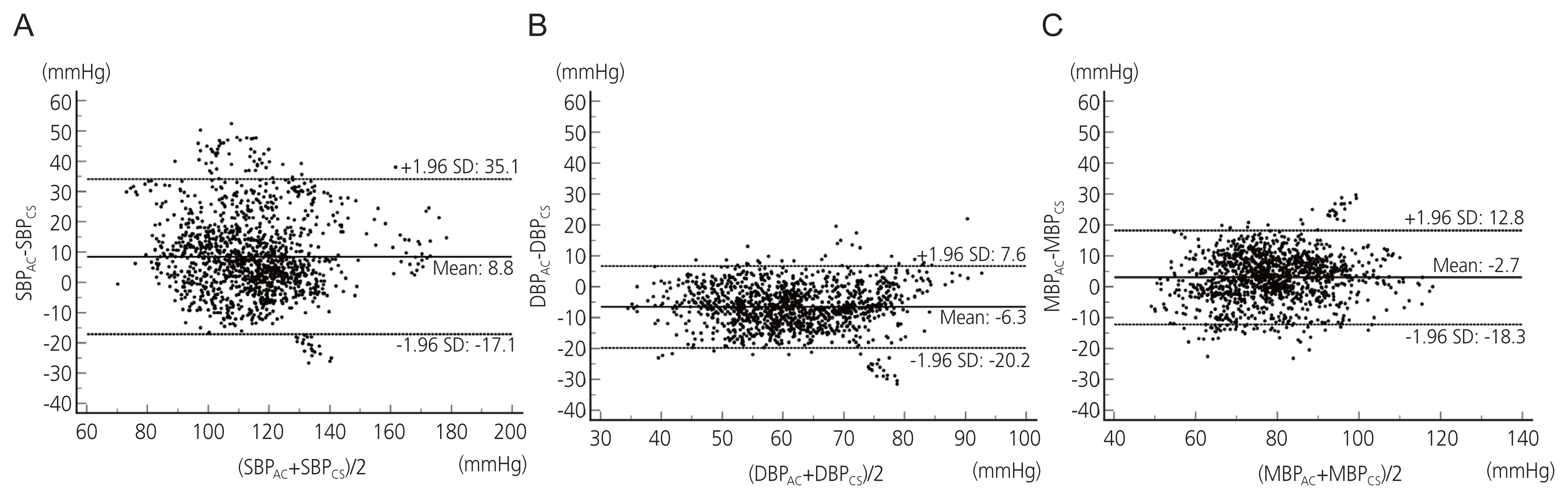
Total 1,277 blood pressure measurement pairs were collected from 21 patients. Under Bland-Altman analysis, the ClearSight system demonstrated an acceptable accuracy with a bias and standard deviation of 8.8±13.4 mmHg for systolic blood pressure, -6.3±7.1 mmHg for diastolic blood pressure, and -2.7±8.0 mmHg for median blood pressure. Cardiac index levels were significantly elevated during fetal delivery and 5 minutes after placental removal, and systemic vascular resistance index levels were significantly decreased during fetal delivery and 40 minutes after placental removal.
Conclusion
In patients undergoing cesarean section, the ClearSight system showed excellent accuracy and precision compared to that of the currently used invasive monitoring system.
Figure
Reference
-
References
1. Lee KJ, Sohn S, Hong K, Kim J, Kim R, Lee S, et al. Maternal, infant, and perinatal mortality statistics and trends in Korea between 2009 and 2017. Obstet Gynecol Sci. 2020; 63:623–30.
Article2. Kim HY, Lee D, Kim J, Noh E, Ahn KH, Hong SC, et al. Secular trends in cesarean sections and risk factors in South Korea (2006–2015). Obstet Gynecol Sci. 2020; 63:440–7.
Article3. Dilla AJ, Waters JH, Yazer MH. Clinical validation of risk stratification criteria for peripartum hemorrhage. Obstet Gynecol. 2013; 122:120–6.
Article4. Cannesson M, Pestel G, Ricks C, Hoeft A, Perel A. Hemodynamic monitoring and management in patients undergoing high risk surgery: a survey among North American and European anesthesiologists. Crit Care. 2011; 15:R197.
Article5. Huygh J, Peeters Y, Bernards J, Malbrain ML. Hemodynamic monitoring in the critically ill: an overview of current cardiac output monitoring methods. F1000Res. 2016; 5:F1000 F. aculty Rev-2855.
Article6. Brzezinski M, Luisetti T, London MJ. Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg. 2009; 109:1763–81.
Article7. Bartels K, Esper SA, Thiele RH. Blood pressure monitoring for the anesthesiologist: a practical review. Anesth Analg. 2016; 122:1866–79.8. Fischer MO, Avram R, Cârjaliu I, Massetti M, Gérard JL, Hanouz JL, et al. Non-invasive continuous arterial pressure and cardiac index monitoring with Nexfin after cardiac surgery. Br J Anaesth. 2012; 109:514–21.
Article9. Hofhuizen C, Lansdorp B, van der Hoeven JG, Scheffer GJ, Lemson J. Validation of noninvasive pulse contour cardiac output using finger arterial pressure in cardiac surgery patients requiring fluid therapy. J Crit Care. 2014; 29:161–5.
Article10. Juri T, Suehiro K, Kimura A, Mukai A, Tanaka K, Yamada T, et al. Impact of non-invasive continuous blood pressure monitoring on maternal hypotension during cesarean delivery: a randomized-controlled study. J Anesth. 2018; 32:822–30.
Article11. Jauniaux E, Alfirevic Z, Bhide AG, Belfort MA, Burton GJ, Collins SL, et al. Placenta praevia and placenta accreta: diagnosis and management: green-top guideline No. 27a. BJOG. 2019; 126:e1–48.12. Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012; 379:905–14.
Article13. Ward CR. Avoiding an incision through the anterior previa at cesarean delivery. Obstet Gynecol. 2003; 102:552–4.
Article14. Tahara M, Tachibana D, Hamuro A, Misugi T, Nakano A, Koyama M. The ward technique for anterior placenta previa. Arch Gynecol Obstet. 2021; 303:1375–6.
Article15. Hamuro A, Tachibana D, Wada N, Kurihara Y, Katayama H, Misugi T, et al. On-site hemostatic suturing technique for uterine bleeding from placenta previa and subsequent pregnancy. Arch Gynecol Obstet. 2015; 292:1181–2.
Article16. Eeftinck Schattenkerk DW, van Lieshout JJ, van den Meiracker AH, Wesseling KR, Blanc S, Wieling W, et al. Nexfin noninvasive continuous blood pressure validated against riva-rocci/korotkoff. Am J Hypertens. 2009; 22:378–83.
Article17. Sumiyoshi M, Maeda T, Miyazaki E, Hotta N, Sato H, Hamaguchi E, et al. Accuracy of the ClearSight™ system in patients undergoing abdominal aortic aneurysm surgery. J Anesth. 2019; 33:364–71.
Article18. Ganzevoort W, Rep A, Bonsel GJ, de Vries JI, Wolf H. Plasma volume and blood pressure regulation in hypertensive pregnancy. J Hypertens. 2004; 22:1235–42.
Article19. Eyeington CT, Lloyd-Donald P, Chan MJ, Eastwood GM, Young H, Peck L, et al. Non-invasive continuous haemodynamic monitoring and response to intervention in haemodynamically unstable patients during rapid response team review. Resuscitation. 2019; 143:124–33.
Article20. Heusdens JF, Lof S, Pennekamp CW, Specken-Welleweerd JC, de Borst GJ, van Klei WA, et al. Validation of non-invasive arterial pressure monitoring during carotid endarterectomy. Br J Anaesth. 2016; 117:316–23.
Article21. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 1:307–10.
Article22. Kim SH, Lilot M, Sidhu KS, Rinehart J, Yu Z, Canales C, et al. Accuracy and precision of continuous noninvasive arterial pressure monitoring compared with invasive arterial pressure: a systematic review and meta-analysis. Anesthesiology. 2014; 120:1080–97.23. Ueland K, Hansen JM. Maternal cardiovascular dynamics. II. Posture and uterine contractions. Am J Obstet Gynecol. 1969; 103:1–7.24. Stover JF, Stocker R, Lenherr R, Neff TA, Cottini SR, Zoller B, et al. Noninvasive cardiac output and blood pressure monitoring cannot replace an invasive monitoring system in critically ill patients. BMC Anesthesiol. 2009; 9:6.
Article25. Hohn A, Defosse JM, Becker S, Steffen C, Wappler F, Sakka SG. Non-invasive continuous arterial pressure monitoring with Nexfin does not sufficiently replace invasive measurements in critically ill patients. Br J Anaesth. 2013; 111:178–84.
Article26. Seifi A, Elliott RJ, Elsehety MA. Usage of Swan-Ganz catheterization during the past 2 decades in United States. J Crit Care. 2016; 35:213–4.
Article27. Monnet X, Teboul JL. Transpulmonary thermodilution: advantages and limits. Crit Care. 2017; 21:147.
Article28. Cholley BP, Singer M. Esophageal Doppler: noninvasive cardiac output monitor. Echocardiography. 2003; 20:763–9.
Article29. Truijen J, van Lieshout JJ, Wesselink WA, Westerhof BE. Noninvasive continuous hemodynamic monitoring. J Clin Monit Comput. 2012; 26:267–78.
Article30. Ameloot K, Van De Vijver K, Broch O, Van Regenmortel N, De Laet I, Schoonheydt K, et al. Nexfin noninvasive continuous hemodynamic monitoring: validation against continuous pulse contour and intermittent transpulmonary thermodilution derived cardiac output in critically ill patients. ScientificWorldJournal. 2013; 2013:519080.
Article31. Broch O, Renner J, Gruenewald M, Meybohm P, Schöttler J, Caliebe A, et al. A comparison of the Nexfin® and transcardiopulmonary thermodilution to estimate cardiac output during coronary artery surgery. Anaesthesia. 2012; 67:377–83.32. Chen G, Meng L, Alexander B, Tran NP, Kain ZN, Cannesson M. Comparison of noninvasive cardiac output measurements using the Nexfin monitoring device and the esophageal Doppler. J Clin Anesth. 2012; 24:275–83.
Article33. Bubenek-Turconi SI, Craciun M, Miclea I, Perel A. Non-invasive continuous cardiac output by the Nexfin before and after preload-modifying maneuvers: a comparison with intermittent thermodilution cardiac output. Anesth Analg. 2013; 117:366–72.34. Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999; 15:85–91.35. Romagnoli S, Ricci Z, Quattrone D, Tofani L, Tujjar O, Villa G, et al. Accuracy of invasive arterial pressure monitoring in cardiovascular patients: an observational study. Crit Care. 2014; 18:644.
Article36. McLeod G, Munishankar B, MacGregor H, Murphy DJ. Maternal haemodynamics at elective caesarean section: a randomised comparison of oxytocin 5-unit bolus and placebo infusion with oxytocin 5-unit bolus and 30-unit infusion. Int J Obstet Anesth. 2010; 19:155–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of the ClearSight System in Monitoring Patients with End-Stage Renal Stage: Two Case Reports
- Continuous Blood Pressure Monitorings during Cardiovascular Opertions in Takayasu`s Syndrome
- Usability of Esophageal Doppler for Monitoring of Concealed Retroperitoneal Hemorrhage during Laparoscopy Assisted Subtotal Gastrectomy
- Balanced Anesthesia in a Pregnant Eisenmenger`s Syndrome - A case report
- Clinical Survey of Spinal Anesthesia for Cesarean Section ( 12 years )