Obstet Gynecol Sci.
2022 Jul;65(4):317-324. 10.5468/ogs.22003.
How and on whom to perform uterine-preserving surgery for uterine prolapse
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Korea University Guro Hospital, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Seoul National University Hospital, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2531840
- DOI: http://doi.org/10.5468/ogs.22003
Abstract
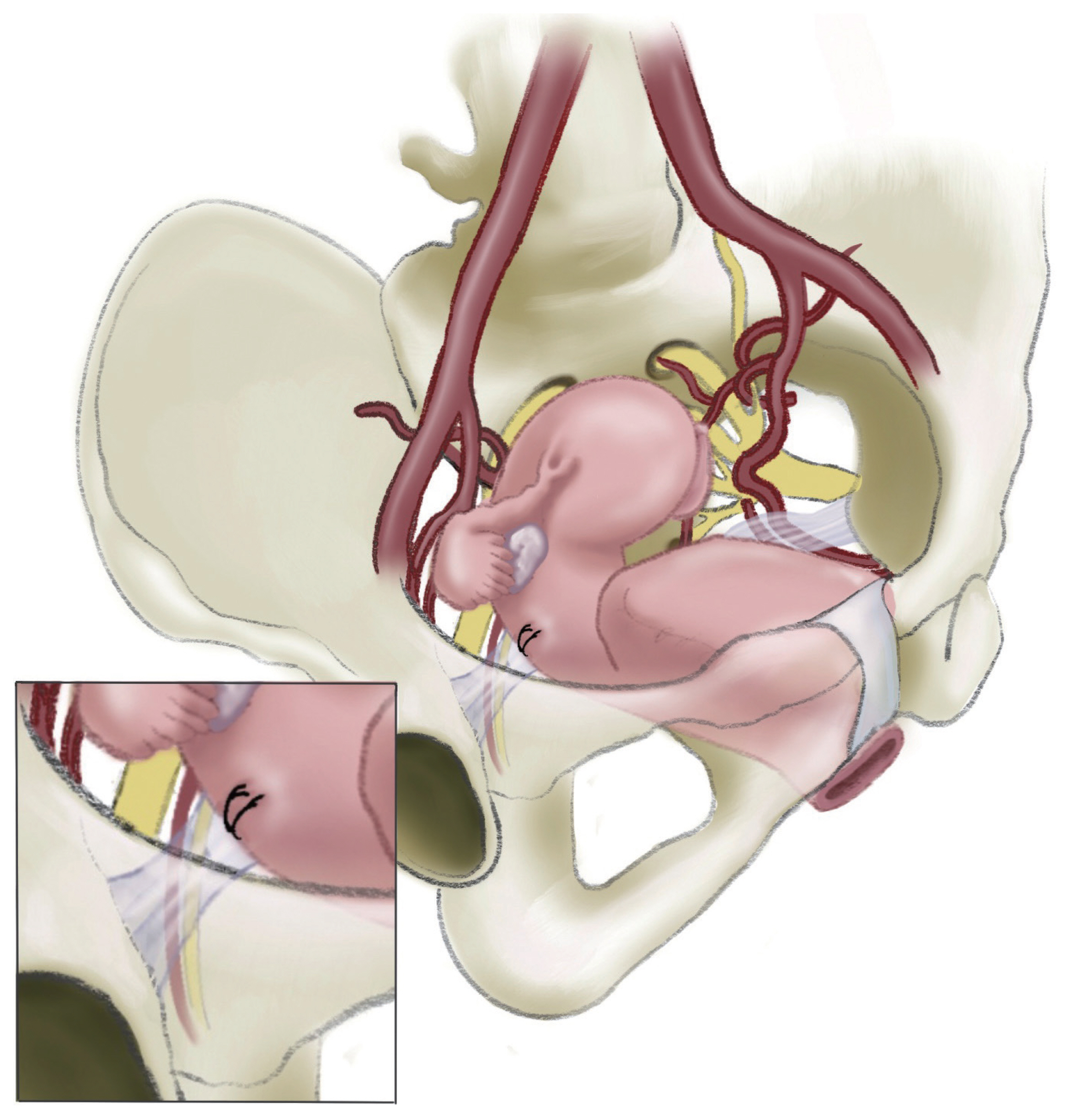
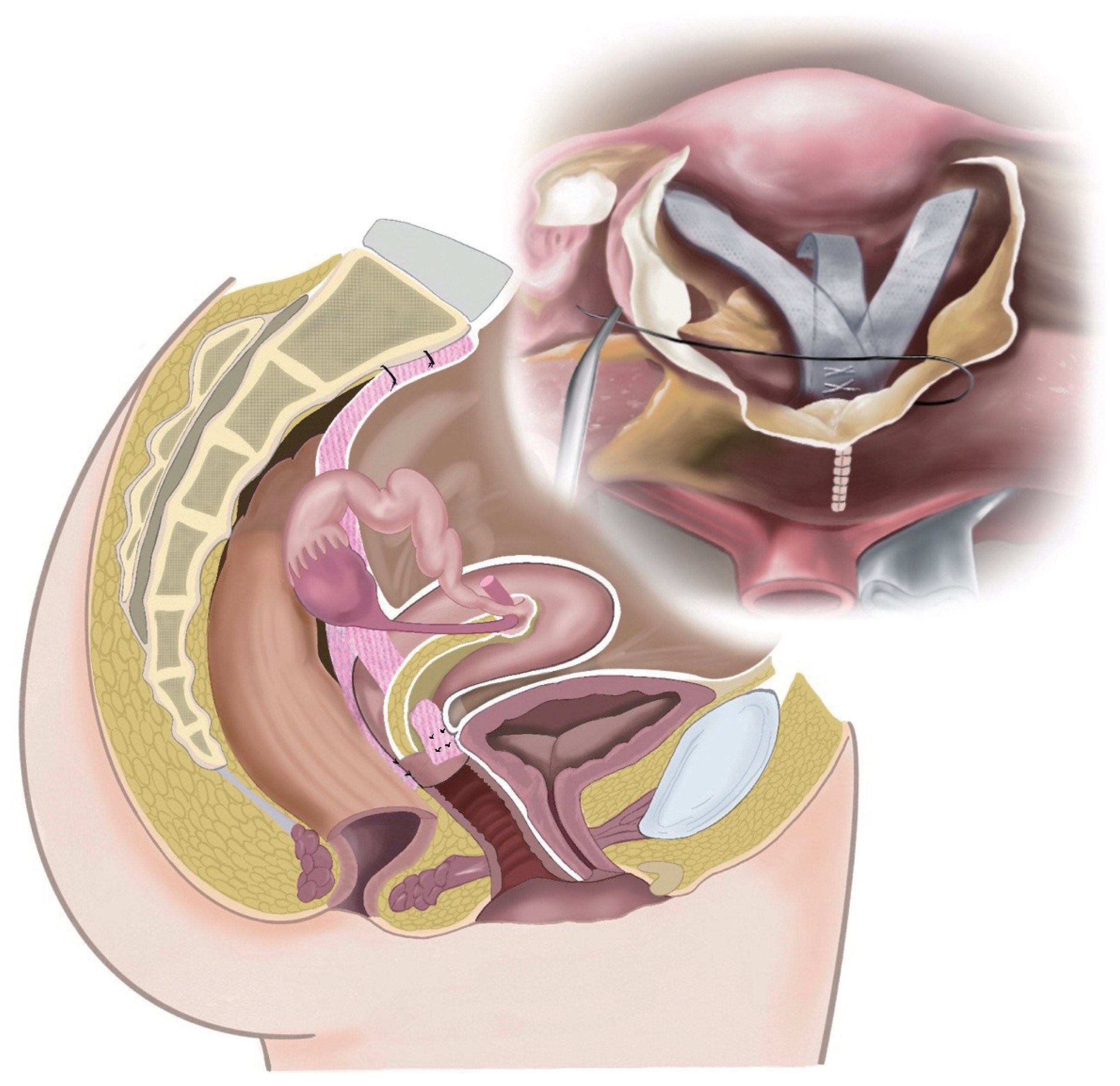
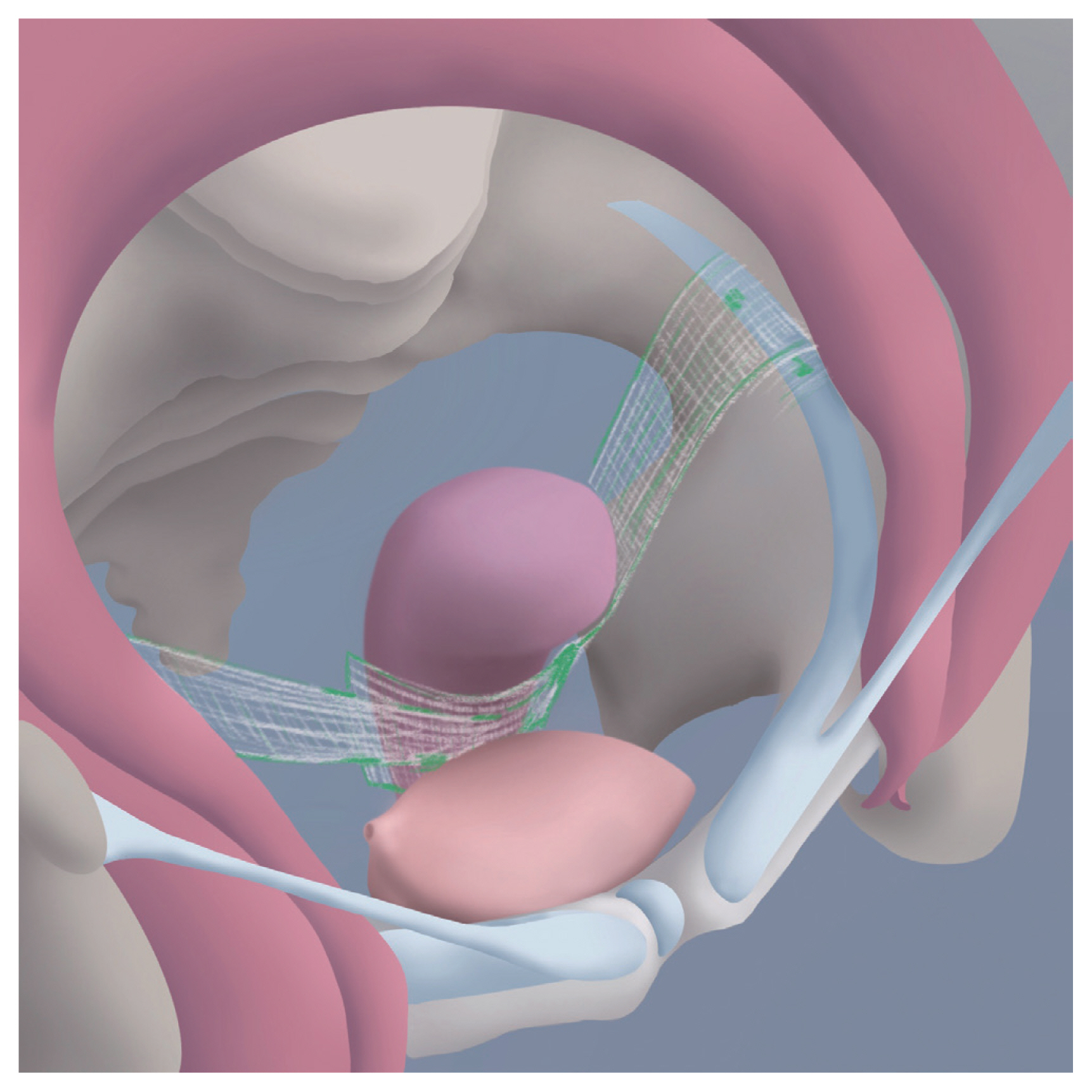
- The demand for uterine preservation in pelvic reconstructive surgery for uterovaginal prolapse is steadily increasing, and several procedures have been introduced, such as sacrospinous hysteropexy, uterosacral hysteropexy, sacrohysteropexy, and hysteropectopexy. However, the benefits and risks of uterine-preserving surgeries are not well understood. This review discusses the current evidence surrounding uterine-preserving surgery for uterovaginal prolapse repair. This may help surgeons and patients have a balanced discussion on how and on whom to perform uterine-preserving surgery.
Keyword
Figure
Cited by 1 articles
-
Outcomes of robotic sacrocolpopexy
Sumin Oh, Jung-Ho Shin
Obstet Gynecol Sci. 2023;66(6):509-517. doi: 10.5468/ogs.23073.
Reference
-
References
1. Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg. 2013; 19:103–9.
Article2. Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013; 209:470e1–6.3. Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013; 24:1803–13.
Article4. Ridgeway B, Frick AC, Walter MD. Hysteropexy. A review. Minerva Ginecol. 2008; 60:509–28.5. Gutman RE. Does the uterus need to be removed to correct uterovaginal prolapse? Curr Opin Obstet Gynecol. 2016; 28:435–40.
Article6. Kow N, Goldman HB, Ridgeway B. Management options for women with uterine prolapse interested in uterine preservation. Curr Urol Rep. 2013; 14:395–402.
Article7. Kim BH, Lee SB, Na ED, Kim HC. Correlation between obesity and pelvic organ prolapse in Korean women. Obstet Gynecol Sci. 2020; 63:719–25.
Article8. Frick AC, Walters MD, Larkin KS, Barber MD. Risk of unanticipated abnormal gynecologic pathology at the time of hysterectomy for uterovaginal prolapse. Am J Obstet Gynecol. 2010; 202:507e1–4.
Article9. Suh DH, Jeon MJ. Risk factors for the failure of iliococcygeus suspension for uterine prolapse. Eur J Obstet Gynecol Reprod Biol. 2018; 225:210–3.
Article10. Lin TY, Su TH, Wang YL, Lee MY, Hsieh CH, Wang KG, et al. Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc. 2005; 104:249–53.11. Ridgeway BM. Does prolapse equal hysterectomy? The role of uterine conservation in women with uterovaginal prolapse. Am J Obstet Gynecol. 2015; 213:802–809.
Article12. de Oliveira SA, Fonseca MCM, Bortolini MAT, Girão MJBC, Roque MT, Castro RA. Hysteropreservation versus hysterectomy in the surgical treatment of uterine prolapse: systematic review and meta-analysis. Int Urogynecol J. 2017; 28:1617–30.
Article13. Meriwether KV, Balk EM, Antosh DD, Olivera CK, Kim-Fine S, Murphy M, et al. Uterine-preserving surgeries for the repair of pelvic organ prolapse: a systematic review with meta-analysis and clinical practice guidelines. Int Urogynecol J. 2019; 30:505–22.
Article14. Nesbitt RE Jr. Uterine preservation in the surgical management of genuine stress urinary incontinence associated with uterovaginal prolapse. Surg Gynecol Obstet. 1989; 168:143–7.15. Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015; 351:h3717.
Article16. Dallas K, Elliott CS, Syan R, Sohlberg E, Enemchukwu E, Rogo-Gupta L. Association between concomitant hysterectomy and repeat surgery for pelvic organ prolapse repair in a cohort of nearly 100,000 women. Obstet Gynecol. 2018; 132:1328–36.
Article17. Jeng CJ, Yang YC, Tzeng CR, Shen J, Wang LR. Sexual functioning after vaginal hysterectomy or transvaginal sacrospinous uterine suspension for uterine prolapse: a comparison. J Reprod Med. 2005; 50:669–74.18. Yazbeck C. Sexual function following hysterectomy. Gynecol Obstet Fertil. 2004; 32:49–54.19. Mokate T, Wright C, Mander T. Hysterectomy and sexual function. J Br Menopause Soc. 2006; 12:153–7.
Article20. Danesh M, Hamzehgardeshi Z, Moosazadeh M, Shabani-Asrami F. The effect of hysterectomy on women’s sexual function: a narrative review. Med Arch. 2015; 69:387–92.
Article21. Jeon MJ. Surgical decision making for symptomatic pelvic organ prolapse: evidence-based approach. Obstet Gynecol Sci. 2019; 62:307–12.
Article22. Ridgeway BM, Frick AC. Uterine conservation for the surgical treatment of uterovaginal prolapse. Walter Mark, Karram M, editors. Urogynecology and reconstructive pelvic surgery. Phildelphia (PA): Elsevier Saunders;2015. p. 383–99.23. Romanzi LJ, Tyagi R. Hysteropexy compared to hysterectomy for uterine prolapse surgery: does durability differ? Int Urogynecol J. 2012; 23:625–31.
Article24. Barranger E, Fritel X, Pigne A. Abdominal sacrohysteropexy in young women with uterovaginal prolapse: long-term follow-up. Am J Obstet Gynecol. 2003; 189:1245–50.
Article25. Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES. Prevalence and risk factors for mesh erosion after laparoscopic-assisted sacrocolpopexy. Int Urogynecol J. 2011; 22:205–12.
Article26. Banerjee C, Noé KG. Laparoscopic pectopexy: a new technique of prolapse surgery for obese patients. Arch Gynecol Obstet. 2011; 284:631–5.
Article27. Yu EH, Jung HE, Noh HK, Joo JK. Initial experience of laparoscopic pectopexy for apical prolapse in South Korea. J Menopausal Med. 2020; 26:165–8.
Article28. Tahaoglu AE, Bakir MS, Peker N, Bagli İ, Tayyar AT. Modified laparoscopic pectopexy: short-term follow-up and its effects on sexual function and quality of life. Int Urogynecol J. 2018; 29:1155–60.
Article29. Food and Drug Administration (FDA). Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. Silver Spring (MD): FDA;2011.30. Food US; Drug Administration (FDA). FDA takes action to protect women’s health, orders manufacturers of surgical mesh intended for transvaginal repair of pelvic organ prolapse to stop selling all devices. Silver Spring (MD): FDA;2019.31. Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013; (4):CD004014.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Uterine Prolapse in Pregnancy
- Ureteral Obstruction Caused by Uterine Prolapse: 5 Cases
- Urodynamic Characteristics of Women with Severe Uterine Prolapse
- To cases of uterine prolapse combined with cervical carcinoma
- A Case Report of Rectal Herniation through Rectovaginal Fistula Associated with Uterine Prolapse