Acute Crit Care.
2022 May;37(2):237-246. 10.4266/acc.2021.01095.
Changes in the incidence of cardiopulmonary resuscitation before and after implementation of the Life-Sustaining Treatment Decisions Act
- Affiliations
-
- 1Department of Critical Care Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2531682
- DOI: http://doi.org/10.4266/acc.2021.01095
Abstract
- Background
The Life-Sustaining Treatment (LST) Decisions Act allows withholding and withdrawal of LST, including cardiopulmonary resuscitation (CPR). In the present study, the incidence of CPR before and after implementation of the Act was compared.
Methods
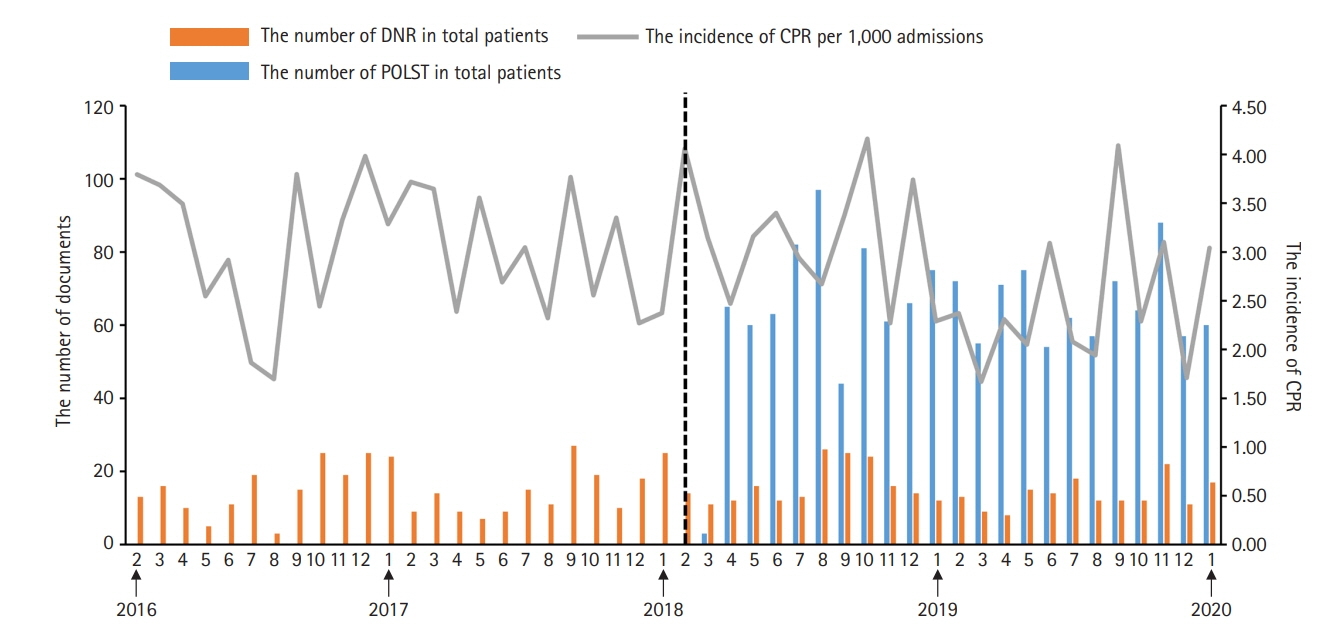
This was a retrospective review involving hospitalized patients who underwent CPR at a single center between February 2016 and January 2020 (pre-implementation period, February 2016 to January 2018; post-implementation period, February 2018 to January 2020). The primary outcome was monthly incidence of CPR per 1,000 admissions. The secondary outcomes were duration of CPR, return of spontaneous circulation (ROSC) rate, 24-hour survival rate, and survival-to-discharge rate. The study outcomes were compared before and after implementation of the Act.
Results
A total of 867 patients who underwent CPR was included in the analysis. The incidence of CPR per 1,000 admissions showed no significant difference before and after implementation of the Act (3.02±0.68 vs. 2.81±0.75, P=0.255). The ROSC rate (67.20±0.11 vs. 70.99±0.12, P=0.008) and survival to discharge rate (20.24±0.09 vs. 22.40±0.12, P=0.029) were higher after implementation of the Act than before implementation.
Conclusions
The incidence of CPR did not significantly change for 2 years after implementation of the Act. Further studies are needed to assess the changes in trends in the decisions of CPR and other LSTs in real-world practice.
Figure
Cited by 1 articles
-
Will implementation of the Life-Sustaining Treatment Decisions Act reduce the incidence of cardiopulmonary resuscitation?
In-Ae Song
Acute Crit Care. 2022;37(2):256-257. doi: 10.4266/acc.2022.00668.
Reference
-
1. Decisions near the end of life. Council on Ethical and Judicial Affairs, American Medical Association. JAMA. 1992; 267:2229–33.2. Reynolds S, Cooper AB, McKneally M. Withdrawing life-sustaining treatment: ethical considerations. Thorac Surg Clin. 2005; 15:469–80.
Article3. Krischer JP, Fine EG, Davis JH, Nagel EL. Complications of cardiac resuscitation. Chest. 1987; 92:287–91.
Article4. Deliliga A, Chatzinikolaou F, Koutsoukis D, Chrysovergis I, Voultsos P. Cardiopulmonary resuscitation (CPR) complications encountered in forensic autopsy cases. BMC Emerg Med. 2019; 19:23.
Article5. Compton S, Grace H, Madgy A, Swor RA. Post-traumatic stress disorder symptomology associated with witnessing unsuccessful out-of-hospital cardiopulmonary resuscitation. Acad Emerg Med. 2009; 16:226–9.
Article6. Kim H, Im HS, Lee KO, Min YJ, Jo JC, Choi Y, et al. Changes in decision-making process for life-sustaining treatment in patients with advanced cancer after the life-sustaining treatment decisions-making act. BMC Palliat Care. 2021; 20:63.
Article7. Kim JS, Yoo SH, Choi W, Kim Y, Hong J, Kim MS, et al. Implication of the life-sustaining treatment decisions act on end-of-life care for Korean terminal patients. Cancer Res Treat. 2020; 52:917–24.
Article8. Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014; 28:1000–25.
Article9. Han B, Chen X, Li Q. Application of case mix index in the allocation of nursing human resources. J Nurs Manag. 2018; 26:647–52.
Article10. Part 6: advance cardiovascular life support. Section 7: algorithm approach to ACLS emergencies. 7A: principles and practice of ACLS. European Resuscitation Council. Resuscitation. 2000; 46:163–6.11. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004; 110:3385–97.
Article12. Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002; 27:299–309.
Article13. Bhargava A, Franzini L, Narendranathan W. Serial correlation and the fixed effects model. Rev Econ Stud. 1982; 49:533–49.
Article14. Kirchhoff KT, Anumandla PR, Foth KT, Lues SN, Gilbertson-White SH. Documentation on withdrawal of life support in adult patients in the intensive care unit. Am J Crit Care. 2004; 13:328–34.
Article15. Lee SI, Hong KS, Park J, Lee YJ. Decision-making regarding withdrawal of life-sustaining treatment and the role of intensivists in the intensive care unit: a single-center study. Acute Crit Care. 2020; 35:179–88.
Article16. Beach MC, Morrison RS. The effect of do-not-resuscitate orders on physician decision-making. J Am Geriatr Soc. 2002; 50:2057–61.
Article17. Vranas KC, Lin AL, Zive D, Tolle SW, Halpern SD, Slatore CG, et al. The association of physician orders for life-sustaining treatment with intensity of treatment among patients presenting to the emergency department. Ann Emerg Med. 2020; 75:171–80.
Article18. Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: a review. JAMA. 2019; 321:1200–10.19. Tirkkonen J, Hellevuo H, Olkkola KT, Hoppu S. Aetiology of in-hospital cardiac arrest on general wards. Resuscitation. 2016; 107:19–24.
Article20. Bergum D, Nordseth T, Mjølstad OC, Skogvoll E, Haugen BO. Causes of in-hospital cardiac arrest: incidences and rate of recognition. Resuscitation. 2015; 87:63–8.
Article21. Yang E, Lee H, Lee SM, Kim S, Ryu HG, Lee HJ, et al. Effectiveness of a daytime rapid response system in hospitalized surgical ward patients. Acute Crit Care. 2020; 35:77–86.
Article22. Cho JY, Lee DS, Choi YY, Park JS, Cho YJ, Yoon HI, et al. Analysis of avoidable cardiopulmonary resuscitation incidents with a part-time rapid response system in place. Acute Crit Care. 2021; 36:109–17.
Article23. Perman SM, Stanton E, Soar J, Berg RA, Donnino MW, Mikkelsen ME, et al. Location of in-hospital cardiac arrest in the United States: variability in event rate and outcomes. J Am Heart Assoc. 2016; 5:e003638.24. Leloup M, Briatte I, Langlois A, Cariou A, Lesieur O, ACIR study group. Unexpected cardiac arrests occurring inside the ICU: outcomes of a French prospective multicenter study. Intensive Care Med. 2020; 46:1005–15.
Article25. Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS, et al. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012; 367:1912–20.
Article26. Ouyang DJ, Lief L, Russell D, Xu J, Berlin DA, Gentzler E, et al. Timing is everything: early do-not- resuscitate orders in the intensive care unit and patient outcomes. PLoS One. 2020; 15:e0227971.27. Zive DM, Fromme EK, Schmidt TA, Cook JN, Tolle SW. Timing of POLST form completion by cause of death. J Pain Symptom Manage. 2015; 50:650–8.
Article28. Levin TT, Li Y, Weiner JS, Lewis F, Bartell A, Piercy J, et al. How do-not-resuscitate orders are utilized in cancer patients: timing relative to death and communication-training implications. Palliat Support Care. 2008; 6:341–8.
Article29. van der Heide A, Deliens L, Faisst K, Nilstun T, Norup M, Paci E, et al. End-of-life decision-making in six European countries: descriptive study. Lancet. 2003; 362:345–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Will implementation of the Life-sustaining Treatment Decisions Act reduce the incidence of cardiopulmonary resuscitation?
- Well-Dying: Assisted Justice Act as a Dignified and Happy ‘Right to Self-Determination’
- Problems Related to the Act on Decisions on Life-Sustaining Treatment and Directions for Improvement
- Implementation of Antimicrobial Stewardship Programs in End-of-Life Care
- The Impact of Withdrawing or Withholding of Life-Sustaining Treatment: A Nationwide Case-Control Study Based on Medical Cost Analysis