Neurointervention.
2022 Jul;17(2):126-130. 10.5469/neuroint.2022.00045.
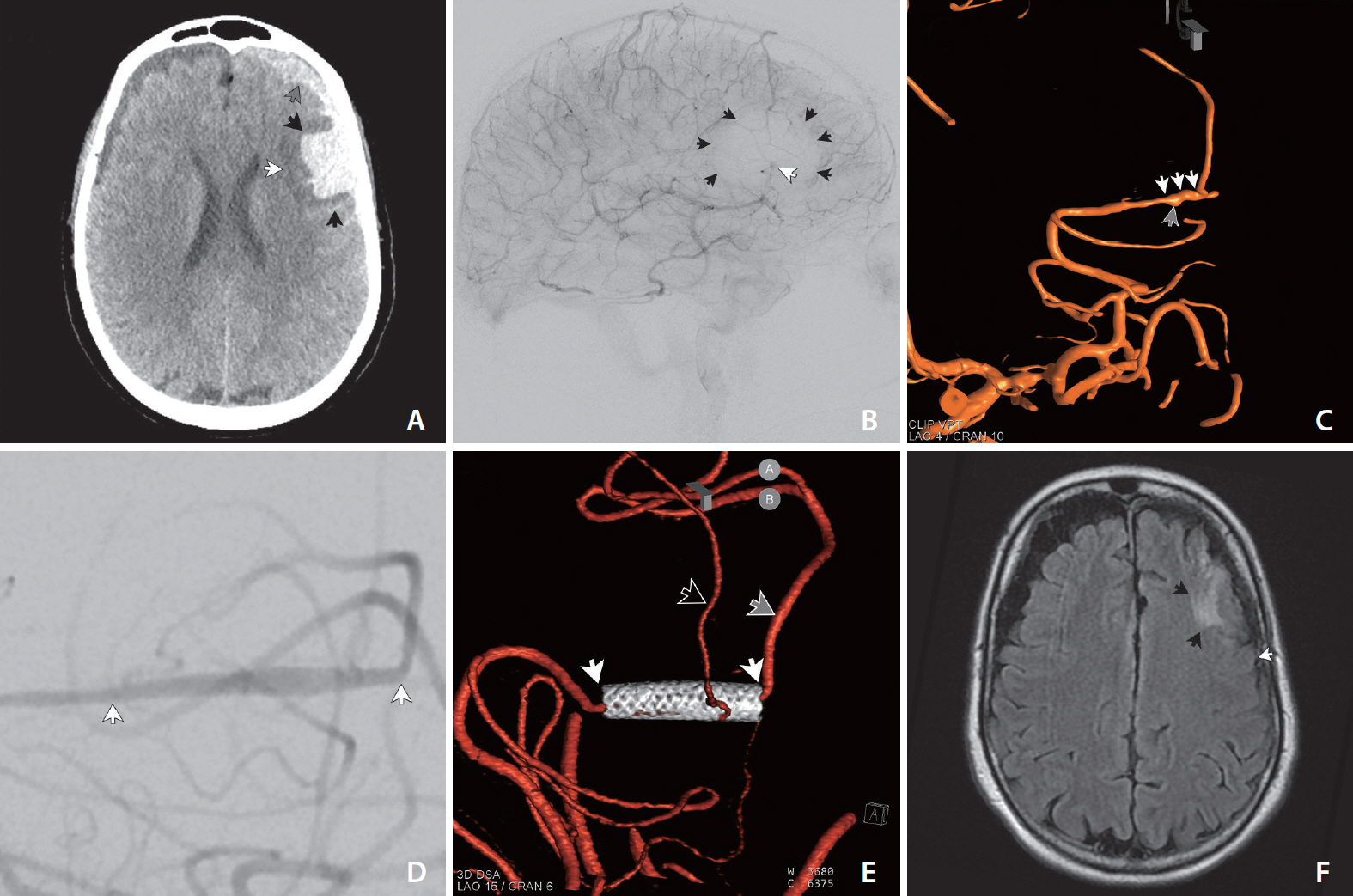
The Use of a Pipeline Embolization Device for Treatment of a Ruptured Dissecting Middle Cerebral Artery M3/M4 Aneurysm: Challenges and Technical Considerations
- Affiliations
-
- 1Department of Neurosurgery, Indiana University School of Medicine, Indianapolis, IN, USA
- 2Division of Interventional Neuroradiology, Goodman Campbell Brain and Spine at Ascension St. Vincent Hospital, Carmel, IN, USA
- KMID: 2531570
- DOI: http://doi.org/10.5469/neuroint.2022.00045
Abstract
- Prompt, effective treatment is necessary following aneurysmal subarachnoid hemorrhage to prevent recurrent rupture, which is thought to double mortality. Atypical ruptured aneurysms, such as blister or dissecting pseudoaneurysms, or those that are unusually distal in the middle cerebral artery (MCA) are challenging to treat with either open or endovascular options, though the pipeline embolization device (PED) has shown promise in multiple case series. We present a case of a ruptured dissecting pseudoaneurysm in the distal MCA (distal M3/proximal M4) prefrontal division in an healthy young patient (<60 years) successfully treated with a PED. The PED was chosen both as the only vessel sparing option in the young patient as well as for its potential as a vessel sacrifice tool if the pseudoaneurysm was felt to be incompletely treated, which in this case was not necessary—though would have leveraged the thrombogenicity of the device as a therapeutic advantage.
Figure
Reference
-
1. Long B, Koyfman A, Runyon MS. Subarachnoid hemorrhage: updates in diagnosis and management. Emerg Med Clin North Am. 2017; 35:803–824.2. Keedy A. An overview of intracranial aneurysms. Mcgill J Med. 2006; 9:141–146.
Article3. Joo SP, Kim TS, Choi JW, Lee JK, Kim YS, Moon KS, et al. Characteristics and management of ruptured distal middle cerebral artery aneurysms. Acta Neurochir (Wien). 2007; 149:661–667.
Article4. Cunegatto-Braga M, Hogan B, Aguilar-Salinas P, Beier AD, Hanel RA. Pipeline embolization device flow diversion for a dissecting ruptured posterior cerebral artery aneurysm in a pediatric patient. World Neurosurg. 2018; 117:255–260.
Article5. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; 267:858–868.
Article6. Hanel RA, Kallmes DF, Lopes DK, Nelson PK, Siddiqui A, Jabbour P, et al. Prospective study on embolization of intracranial aneurysms with the pipeline device: the PREMIER study 1 year results. J Neurointerv Surg. 2020; 12:62–66.
Article7. Chalouhi N, Zanaty M, Whiting A, Tjoumakaris S, Hasan D, Ajiboye N, et al. Treatment of ruptured intracranial aneurysms with the pipeline embolization device. Neurosurgery. 2015; 76:165–172. discussion 172.
Article8. Lozupone E, Piano M, Valvassori L, Quilici L, Pero G, Visconti E, et al. Flow diverter devices in ruptured intracranial aneurysms: a single-center experience. J Neurosurg. 2018; 128:1037–1043.
Article9. Johnson AM, Sugo E, Barreto D, Hiew CC, Lawson JA, Connolly AM, et al. The severity of gliosis in hippocampal sclerosis correlates with pre-operative seizure burden and outcome after temporal lobectomy. Mol Neurobiol. 2016; 53:5446–5456.
Article10. Bender MT, Zarrin DA, Campos JK, Lin LM, Huang J, Caplan JM, et al. Tiny pipes: 67 cases of flow diversion for aneurysms in distal vessels measuring less than 2.0 mm. World Neurosurg. 2019; 127:e193–e201.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inadvertent Complication of a Pipeline Embolization Device for Treatment with Vertebral Artery Dissecting Aneurysm : Distal Tip Fracture of Delivery Wire
- A Case of Migration of Pipeline Embolization Device Causing Rupture during Treatment of an Unruptured Vertebral Artery Dissecting Aneurysm
- Ruptured Dissecting Aneurysm of the Middle Cerebral Artery with Spontaneous Resolution: A Case Report
- Distal Middle Cerebral Artery M4 Aneurysm Surgery Using Navigation-CT Angiography
- Coil Embolization for Distal Middle Cerebral Artery Aneurysm