Pediatr Emerg Med J.
2022 Jun;9(1):48-51. 10.22470/pemj.2022.00479.
Kawasaki disease shock syndrome rescued by a combination of extracorporeal membrane oxygenation, steroids, and intravenous immunoglobulin
- Affiliations
-
- 1Division of Pediatric Cardiology, Department of Pediatrics, Pusan National University Yangsan Hospital, Yangsan, Republic of Korea
- KMID: 2531530
- DOI: http://doi.org/10.22470/pemj.2022.00479
Abstract
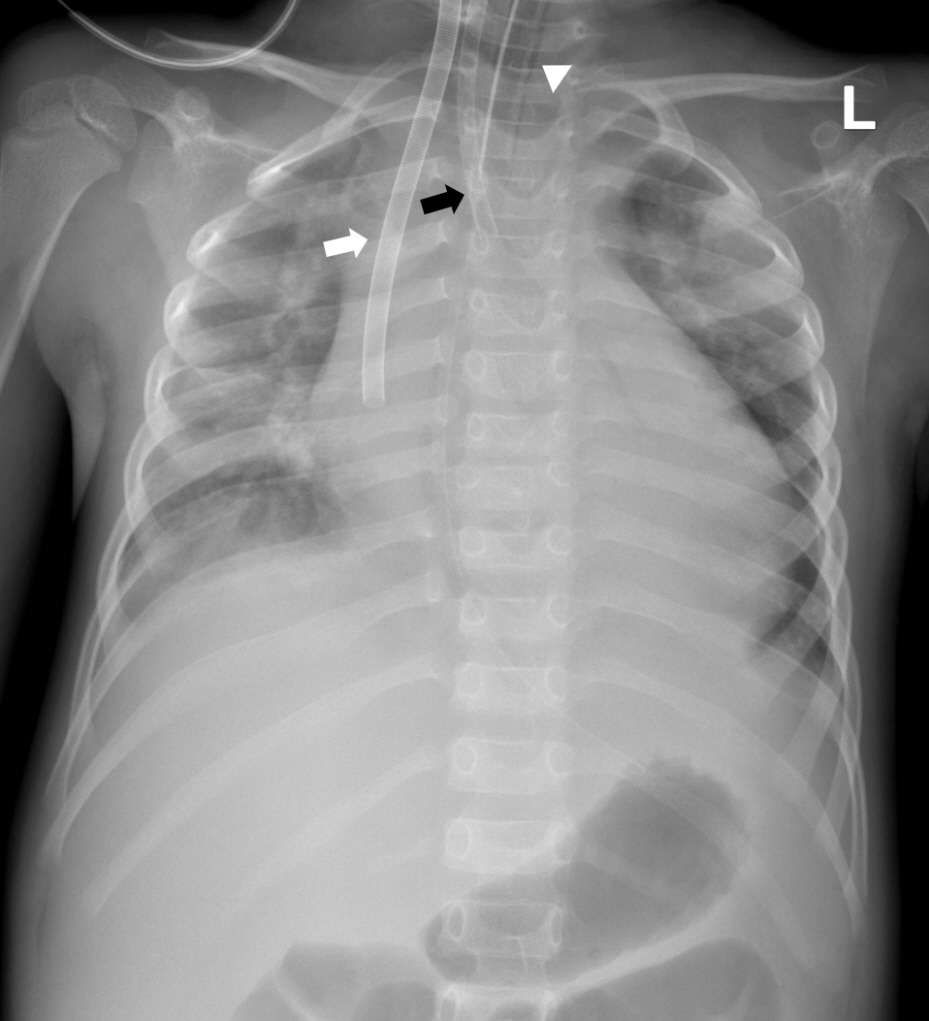
- Kawasaki disease shock syndrome (KDSS) is defined as a sustained decrease in systolic blood pressure or signs of poor perfusion. Some children with KDSS are refractory to conventional therapy, such as intravenous immunoglobulin (IVIG). A 4-year-old boy with Kawasaki disease was referred to the emergency department. Despite the conventional therapy, his vital signs and cardiac function worsened. The boy promptly underwent extracorporeal membrane oxygenation (ECMO), which did not relieve the symptoms. Subsequently, he underwent methylprednisolone pulse therapy and the second cycle of IVIG therapy. Two days after the start of a combination of ECMO, steroids, and IVIG started, his clinical condition was stabilized, and finally, ECMO was removed. This case highlights the combination of ECMO, steroids, and IVIG as a treatment option for children with IVIG-resistant KDSS.
Keyword
Figure
Reference
-
References
1. Kanegaye JT, Wilder MS, Molkara D, Frazer JR, Pancheri J, Tremoulet AH, et al. Recognition of a Kawasaki disease shock syndrome. Pediatrics. 2009; 123:e783–9.
Article2. Gamez-Gonzalez LB, Moribe-Quintero I, Cisneros-Castolo M, Varela-Ortiz J, Muñoz-Ramírez M, Garrido-García M, et al. Kawasaki disease shock syndrome: unique and severe subtype of Kawasaki disease. Pediatr Int. 2018; 60:781–90.
Article3. Eleftheriou D, Levin M, Shingadia D, Tulloh R, Klein NJ, Brogan PA. Management of Kawasaki disease. Arch Dis Child. 2014; 99:74–83.
Article4. Aggarwal P, Suri D, Narula N, Manojkumar R, Singh S. Symptomatic myocarditis in Kawasaki disease. Indian J Pediatr. 2012; 79:813–4.
Article5. Ono R, Shimizu M, Yamamoto K, Umehara N, Manabe A. Kawasaki disease shock syndrome: case report and cytokine profiling. Pediatr Int. 2019; 61:620–2.
Article6. Park WY, Lee SY, Kim GB, Song MK, Kwon HW, Bae EJ, et al. Clinical aspects for differential diagnosis of Kawasaki disease shock syndrome: a case control study. BMC Pediatr. 2021; 21:25.
Article7. Sato T, Somura J, Maruo Y. Steroid pulse therapy for Kawasaki disease complicated with myocarditis. Indian Pediatr. 2016; 53:1015–6.
Article8. Zhang H, Xie L, Xiao T. Extracorporeal membrane oxygenation support for cardiac dysfunction due to Kawasaki disease shock syndrome. Front Pediatr. 2019; 7:221.
Article9. Best D, Millar J, Kornilov I, Sinelnikov Y, Chiletti R, Rycus P, et al. Extracorporeal membrane oxygenation for Kawasaki disease: two case reports and the Extracorporeal Life Support Organization experience 1999-2015. Perfusion. 2017; 32:609–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catastrophic catecholamine-induced cardiomyopathy rescued by extracorporeal membrane oxygenation in recurrent malignant pheochromocytoma
- A case of rescuing a patient with acute cardiovascular instability from sudden and massive intraoperative pulmonary thromboembolism by extracorporeal membrane oxygenation
- Atypical Kawasaki Disease Presented with Toxic Shock Syndrome
- Preoperative Extracorporeal Membrane Oxygenation for Severe Ischemic Mitral Regurgitation: 2 case reports
- 2009 H1N1 influenza virus infection and necrotizing pneumonia treated with extracorporeal membrane oxygenation