Pediatr Emerg Med J.
2022 Jun;9(1):1-9. 10.22470/pemj.2022.00437.
Risk stratification of intermediate-risk children with minor head injury: a secondary publication translated into Korean
- Affiliations
-
- 1Department of Emergency Medicine, Ajou University School of Medicine, Suwon, Republic of Korea
- KMID: 2531522
- DOI: http://doi.org/10.22470/pemj.2022.00437
Abstract
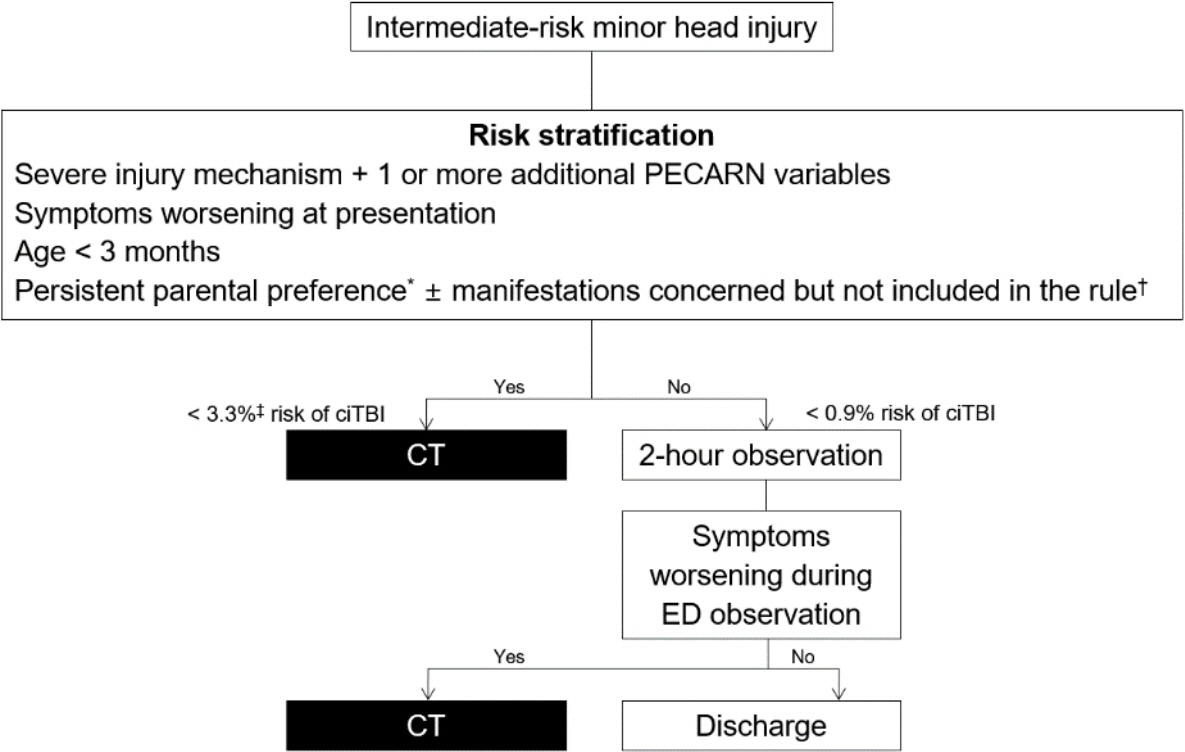
- The Pediatric Emergency Care Applied Research Network rule helps emergency physicians identify very low-risk children with minor head injury who can forgo head computed tomography. This rule contributes to reducing lifetime risk of radiation-induced cancers while minimizing missing clinically important traumatic brain injury. However, in intermediate-risk children, decisions on whether to perform computed tomography remain at the emergency physicians' discretion. To reduce this gray zone, this review summarizes evidence for risk stratification of intermediate-risk children with minor head injury.
Keyword
Figure
Reference
-
References
1. Kuppermann N, Holmes JF, Dayan PS, Hoyle JD Jr, Atabaki SM, Holubkov R, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009; 374:1160–70.
Article2. Babl FE, Borland ML, Phillips N, Kochar A, Dalton S, McCaskill M, et al. Accuracy of PECARN, CATCH, and CHALICE head injury decision rules in children: a prospective cohort study. Lancet. 2017; 389:2393–402.
Article3. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007; 357:2277–84.
Article4. Stein SC, Hurst RW, Sonnad SS. Meta-analysis of cranial CT scans in children. A mathematical model to predict radiation-induced tumors. Pediatr Neurosurg. 2008; 44:448–57.5. Bressan S, Steiner IP, Mion T, Berlese P, Romanato S, Da Dalt L. The Pediatric Emergency Care Applied Research Network intermediate-risk predictors were not associated with scanning decisions for minor head injuries. Acta Paediatr. 2015; 104:47–52.
Article6. Homme JJ. Pediatric minor head injury 2.0: moving from injury exclusion to risk stratification. Emerg Med Clin North Am. 2018; 36:287–304.7. Nigrovic LE, Lee LK, Hoyle J, Stanley RM, Gorelick MH, Miskin M, et al. Prevalence of clinically important traumatic brain injuries in children with minor blunt head trauma and isolated severe injury mechanisms. Arch Pediatr Adolesc Med. 2012; 166:356–61.
Article8. Lee LK, Monroe D, Bachman MC, Glass TF, Mahajan PV, Cooper A, et al. Isolated loss of consciousness in children with minor blunt head trauma. JAMA Pediatr. 2014; 168:837–43.
Article9. Dayan PS, Holmes JF, Schutzman S, Schunk J, Lichenstein R, Foerster LA, et al. Risk of traumatic brain injuries in children younger than 24 months with isolated scalp hematomas. Ann Emerg Med. 2014; 64:153–62.10. Nishijima DK, Holmes JF, Dayan PS, Kuppermann N. Association of a guardian’s report of a child acting abnormally with traumatic brain injury after minor blunt head trauma. JAMA Pediatr. 2015; 169:1141–7.
Article11. Dayan PS, Holmes JF, Atabaki S, Hoyle J Jr, Tunik MG, Lichenstein R, et al. Association of traumatic brain injuries with vomiting in children with blunt head trauma. Ann Emerg Med. 2014; 63:657–65.
Article12. Dayan PS, Holmes JF, Hoyle J Jr, Atabaki S, Tunik MG, Lichenstein R, et al. Headache in traumatic brain injuries from blunt head trauma. Pediatrics. 2015; 135:504–12.
Article13. Graham ID, Stiell IG, Laupacis A, O’Connor AM, Wells GA. Emergency physicians’ attitudes toward and use of clinical decision rules for radiography. Acad Emerg Med. 1998; 5:134–40.
Article14. Eagles D, Stiell IG, Clement CM, Brehaut J, Taljaard M, Kelly AM, et al. International survey of emergency physicians’ awareness and use of the Canadian Cervical-Spine Rule and the Canadian Computed Tomography Head Rule. Acad Emerg Med. 2008; 15:1256–61.
Article15. Ballard DW, Rauchwerger AS, Reed ME, Vinson DR, Mark DG, Offerman SR, et al. Emergency physicians’ knowledge and attitudes of clinical decision support in the electronic health record: a survey-based study. Acad Emerg Med. 2013; 20:352–60.
Article16. Croskerry P. Clinical cognition and diagnostic error: applications of a dual process model of reasoning. Adv Health Sci Educ Theory Pract. 2009; 14 Suppl 1:27–35.
Article17. Shaw K. To err is human, but our errors affect children how you reason reduces errors. In : Proceedings of the Advanced Pediatric Emergency Medicine Assembly; 2018 Mar 13-15; Lake Buena Vista, FL. Irving (TX): Americal College of Emergency Physicians;2018. p. unknown.18. Cheng CY, Pan HY, Li CJ, Chen YC, Chen CC, Huang YS, et al. Physicians’ risk tolerance and head computed tomography use for pediatric patients with minor head injury. Pediatr Emerg Care. 2021; 37:e129–35.
Article19. Conrad HB, Hollenbach KA, Ratnayake K, Gehlbach DL, Carstairs KL. A specialized pediatric emergency medicine track decreases computed tomography in head injured patients. Pediatr Emerg Care. 2019; 35:506–8.
Article20. Wylie MC, Merritt C, Clark M, Garro AC, Rutman MS. Imaging of pediatric head injury in the emergency department. Pediatr Emerg Care. 2014; 30:680–5.
Article21. Ukwuoma OI, Allareddy V, Allareddy V, Rampa S, Rose JA, Shein SL, et al. Trends in head computed tomography utilization in children presenting to emergency departments after traumatic head injury. Pediatr Emerg Care. 2021; 37:e384–90.
Article22. Miescier MJ, Dudley NC, Kadish HA, Mundorff MB, Corneli HM. Variation in computed tomography use for evaluation of head injury in a pediatric emergency department. Pediatr Emerg Care. 2017; 33:156–60.
Article23. Corwin DJ, Durbin DR, Hayes KL, Zonfrillo MR. Trends in emergent head computed tomography utilization for minor head trauma after implementation of a clinical pathway. Pediatr Emerg Care. 2021; 37:437–41.
Article24. Lefort R, Hunter JV, Cruz AT, Caviness AC, Luerssen TG, Adekunle-Ojo A. Utility of emergency department observation units for neurologically intact children with head CT abnormalities secondary to acute closed head injury. Pediatr Emerg Care. 2017; 33:161–5.
Article25. Stippler M, Smith C, McLean AR, Carlson A, Morley S, Murray-Krezan C, et al. Utility of routine follow-up head CT scanning after mild traumatic brain injury: a systematic review of the literature. Emerg Med J. 2012; 29:528–32.
Article26. Aziz H, Rhee P, Pandit V, Ibrahim-Zada I, Kulvatunyou N, Wynne J, et al. Mild and moderate pediatric traumatic brain injury: replace routine repeat head computed tomography with neurologic examination. J Trauma Acute Care Surg. 2013; 75:550–4.27. Chern JJ, Sarda S, Howard BM, Jea A, Tubbs RS, Brahma B, et al. Utility of surveillance imaging after minor blunt head trauma. J Neurosurg Pediatr. 2014; 14:306–10.
Article28. Patel SK, Gozal YM, Krueger BM, Bayley JC, Moody S, Andaluz N, et al. Routine surveillance imaging following mild traumatic brain injury with intracranial hemorrhage may not be necessary. J Pediatr Surg. 2018; 53:2048–54.
Article29. Varano P, Cabrera KI, Kuppermann N, Dayan PS. Acute outcomes of isolated cerebral contusions in children with Glasgow Coma Scale scores of 14 to 15 after blunt head trauma. J Trauma Acute Care Surg. 2015; 78:1039–43.
Article30. Hagiwara Y, Inoue N. The effect of an observation unit on pediatric minor head injury. Pediatr Emerg Care. 2020; 36:e564–7.
Article31. Schonfeld D, Fitz BM, Nigrovic LE. Effect of the duration of emergency department observation on computed tomography use in children with minor blunt head trauma. Ann Emerg Med. 2013; 62:597–603.
Article32. Hamilton M, Mrazik M, Johnson DW. Incidence of delayed intracranial hemorrhage in children after uncomplicated minor head injuries. Pediatrics. 2010; 126:e33–9.
Article33. Schutzman SA, Barnes P, Duhaime AC, Greenes D, Homer C, Jaffe D, et al. Evaluation and management of children younger than two years old with apparently minor head trauma: proposed guidelines. Pediatrics. 2001; 107:983–93.
Article34. Christian CW; Committee on Child Abuse and Neglect; American Academy of Pediatrics. The evaluation of suspected child physical abuse. Pediatrics. 2015; 135:e1337–54.
Article35. Greenes DS, Schutzman SA. Clinical indicators of intracranial injury in head-injured infants. Pediatrics. 1999; 104:861–7.
Article36. Rana KS, Behera MK, Adhikari KM. Ischemic stroke following mild head injury is it the cause. Indian Pediatr. 2006; 43:994–7.37. Shaffer L, Rich PM, Pohl KR, Ganesan V. Can mild head injury cause ischaemic stroke? Arch Dis Child. 2003; 88:267–9.
Article38. Hartwig HD, Clingenpeel J, Perkins AM, Rose W, Abdullah-Anyiwo J. Parental knowledge of radiation exposure in medical imaging used in the pediatric emergency department. Pediatr Emerg Care. 2013; 29:705–9.
Article39. Karpas A, Finkelstein M, Reid S. Which management strategy do parents prefer for their head-injured child: immediate computed tomography scan or observation? Pediatr Emerg Care. 2013; 29:30–5.40. Jeong JH, Lee JH, Kim K, Rhee JE, Kim TY, Jo YH, et al. Change in guardians’ preference for computed tomography after explanation by emergency physicians in pediatric head injury. Clin Exp Emerg Med. 2015; 2:226–35.
Article41. Reilly C, Zhang N, Babcock L, Wade SL, Rhine T. Emergency department care of young children at risk for traumatic brain injury: what are we doing and do parents understand? Pediatr Emerg Care. 2019; 35:468–73.42. Hess EP, Homme JL, Kharbanda AB, Tzimenatos L, Louie JP, Cohen DM, et al. Effect of the head computed tomography choice decision aid in parents of children with minor head trauma: a cluster randomized trial. JAMA Netw Open. 2018; 1:e182430.43. Hull A, Friedman T, Christianson H, Moore G, Walsh R, Wills B. Risk acceptance and desire for shared decision making in pediatric computed tomography scans: a survey of 350. Pediatr Emerg Care. 2015; 31:759–61.44. Boutis K, Thomas KE. Radiation dose awareness and disclosure practice in paediatric emergency medicine: how far have we come? Br J Radiol. 2016; 89:20160022.
Article45. Donaldson K, Li X, Sartorelli KH, Weimersheimer P, Durham SR. Management of isolated skull fractures in pediatric patients: a systematic review. Pediatr Emerg Care. 2019; 35:301–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid Nodules with Isolated Macrocalcifications:Malignancy Risk of Isolated Macrocalcifications andPostoperative Risk Stratification of Malignant TumorsManifesting as Isolated Macrocalcifications
- Post-Traumatic Basal Gangliar Ischemia in Children
- Unilateral Internuclear Ophthalmoplegia Following Minor Head Injury
- The Role of Carotid Ultrasound for Cardiovascular Risk Stratification beyond Traditional Risk Factors
- The Usefulness of Serum S-100 beta Levels as a Screening Test for Pediatric Minor Head Trauma