Korean J healthc assoc Infect Control Prev.
2022 Jun;27(1):43-50. 10.14192/kjicp.2022.27.1.43.
Outbreak of Carbapenem-resistant Enterobacteriaceae (CRE) in a Long-term Acute Care Facility in the Republic of Korea
- Affiliations
-
- 1National Rehabitation Center, Seoul, Korea
- 2Graduate School of Urban Public Health, University of Seoul, Seoul, Korea
- 3Department of Urban Big Data Convergence, University of Seoul, Seoul, Korea
- KMID: 2530825
- DOI: http://doi.org/10.14192/kjicp.2022.27.1.43
Abstract
- Background
Carbapenem-resistant Enterobacteriaceae (CRE) emerged in a long-term acute care hospital in 2017. Therefore, this study aimed to examine the reasons for the occurrence of the CRE epidemic, the risk of infection, its spread, and the effects of interventions.
Methods
A total of 149 patients were hospitalised in a long-term acute care hospital, and 15 of 39 patients in the same ward tested positive. A retrospective cohort study was conducted on all patients (n=39) who were hospitalised in the same ward.
Results
The incidence rates of CRE were 50.0% for the intensive care unit, 2.8% for each general ward, and 10.0% for the entire hospital, with a case fatality rate of 53.3%. The risk factors for its spread included antibiotic use (relative risk [RR]=18.12; 95% confidence interval [CI]=2.64-124.5), ventilator use (RR=3.95; 95% CI=1.53-10.22), decubitus (RR=15.56; 95% CI=2.27-106.8), use of tracheostomy tube (RR=2.75; 95% CI=1.06-7.12), and hemodialysis (RR=2.43; 95% CI=1.21-4.89).
Conclusion
Both the incidence and case fatality rates of CRE were increased when it emerged in a long-term acute care hospital. The risk factors for its spread included antibiotic use, decubitus, tracheostomy, ventilator use, and dialysis. Interventions, including intensive infection monitoring, were effective in preventing the spread and relapse of CRE epidemics.
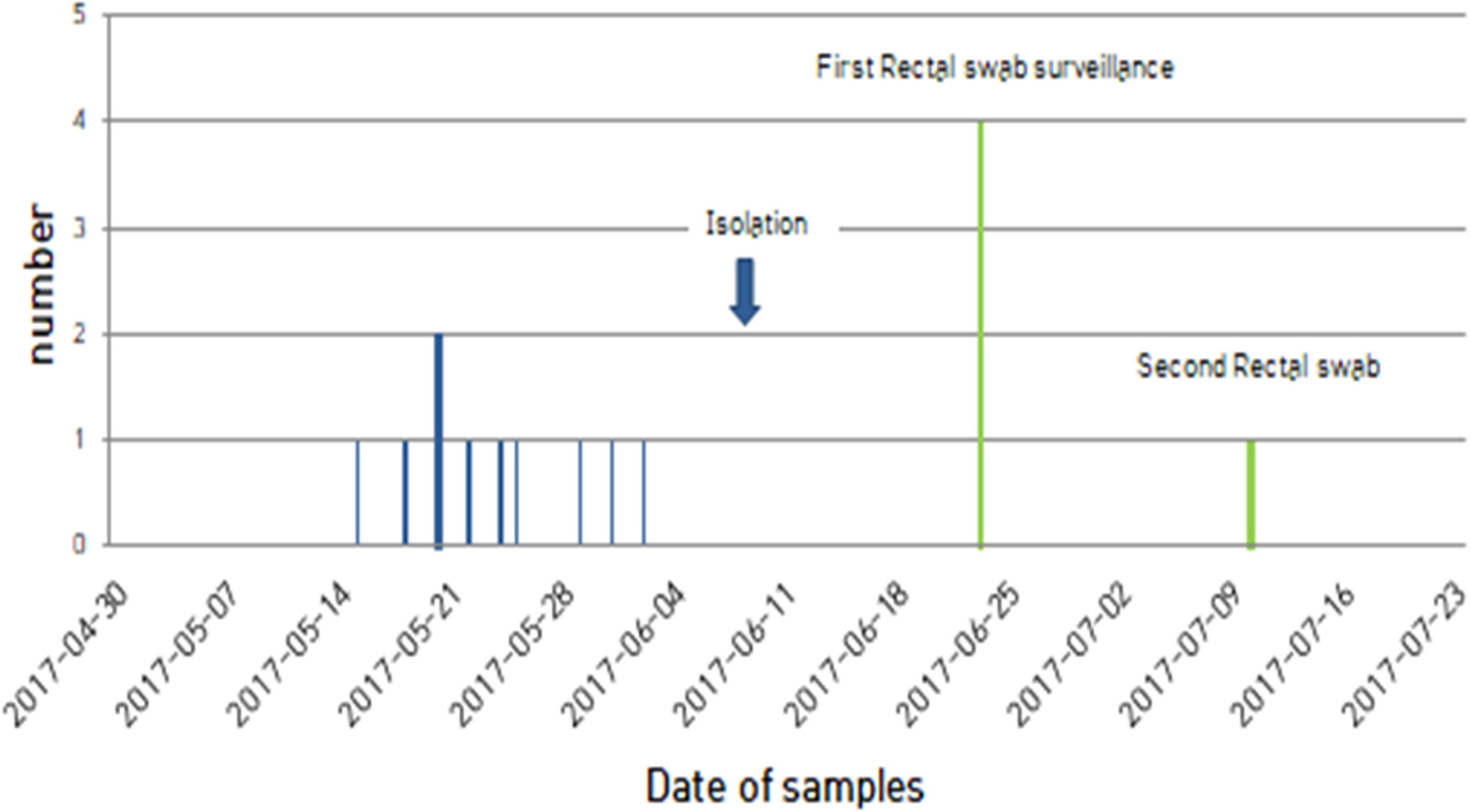
Figure
Reference
-
1. Nordmann P, Naas T, Poirel L. 2011; Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 17:1791–8. DOI: 10.3201/eid1710.110655. PMID: 22000347. PMCID: PMC3310682.2. Gupta N, Limbago BM, Patel JB, Kallen AJ. 2011; Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin Infect Dis. 53:60–7. DOI: 10.1093/cid/cir202. PMID: 21653305.
Article3. Centers for Disease Control. 2009; Guidance for control of infections with carbapenem-resistant or carbapenemase-producing Enterobacteriaceae in acute care facilities. MMWR Morb Mortal Wkly Rep. 58:256–60. PMID: 19300408.4. Centers for Disease Control. 2013. Antibiotic resistance threats in the United States. Centers for Disease Control and Prevention;Atlanta: p. 49–89.5. Peleg AY, Hooper DC. 2010; Hospital-acquired infections due to gram-negative bacteria. N Engl J Med. 362:1804–13. DOI: 10.1056/NEJMra0904124. PMID: 20463340. PMCID: PMC3107499.
Article6. Lin MY, Lyles-Banks RD, Lolans K, Hines DW, Spear JB, Petrak R, et al. 2013; The importance of long-term acute care hospitals in the regional epidemiology of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin Infect Dis. 57:1246–52. DOI: 10.1093/cid/cit500. PMID: 23946222. PMCID: PMC8383150.7. Perez F, Endimiani A, Ray AJ, Decker BK, Wallace CJ, Hujer KM, et al. 2010; Carbapenem-resistant Acinetobacter baumannii and Klebsiella pneumoniae across a hospital system: impact of post-acute care facilities on dissemination. J Antimicrob Chemother. 65:1807–18. DOI: 10.1093/jac/dkq191. PMID: 20513702. PMCID: PMC2904665.
Article8. Toth DJA, Khader K, Slayton RB, Kallen AJ, Gundlapalli AV, O'Hagan JJ, et al. 2017; The Potential for interventions in a long-term acute care hospital to reduce transmission of carbapenem-resistant Enterobacteriaceae in affiliated healthcare facilities. Clin Infect Dis. 65:581–7. DOI: 10.1093/cid/cix370. PMID: 28472233.
Article9. Kim MN, Yong D, An D, Chung HS, Woo JH, Lee K, et al. 2012; Nosocomial clustering of NDM-1-producing Klebsiella pneumoniae sequence type 340 strains in four patients at a South Korean tertiary care hospital. J Clin Microbiol. 50:1433–6. DOI: 10.1128/JCM.06855-11. PMID: 22259206. PMCID: PMC3318568.
Article10. Korea Disease Control. Infectious Disease Portal. http://www.kdca.go.kr/npt/biz/npp/ist/simple/simplePdStatsMain.do. (Updated on 14 June 2022).11. Kim J, Lee JY, Kim SI, Song W, Kim JS, Jung S, et al. 2014; Rates of fecal transmission of extended-spectrum β-lactamase-producing and carbapenem-resistant Enterobacteriaceae among patients in intensive care units in Korea. Ann Lab Med. 34:20–5. DOI: 10.3343/alm.2014.34.1.20. PMID: 24422191. PMCID: PMC3885768.
Article12. Kang JS, Yi J, Ko MK, Lee SO, Lee JE, Kim KH. 2019; Prevalence and risk factors of carbapenem-resistant Enterobacteriaceae acquisition in an emergency intensive care unit in a tertiary hospital in Korea: a case-control study. J Korean Med Sci. 34:e140. DOI: 10.3346/jkms.2019.34.e140. PMID: 31074254. PMCID: PMC6509365.
Article13. Ahn JY, Song JE, Kim MH, Choi H, Kim JK, Ann HW, et al. 2014; Risk factors for the acquisition of carbapenem-resistant Escherichia coli at a tertiary care center in South Korea: a matched case-control study. Am J Infect Control. 42:621–5. DOI: 10.1016/j.ajic.2014.02.024. PMID: 24837112.
Article14. Lee HJ, Choi JK, Cho SY, Kim SH, Park SH, Choi SM, et al. 2016; Carbapenem-resistant Enterobacteriaceae: prevalence and risk factors in a single community-based hospital in Korea. Infect Chemother. 48:166–73. Erratum in: Infect Chemother 2019;51:435-8. DOI: 10.3947/ic.2019.51.4.435. PMID: 31898429. PMCID: PMC6940368.
Article15. Korean Centers for Disease Control. Infection control guidelines for multidrug resistant microorganisms in healthcare facilities. https://www.koshic.org/related/%EB%8B%A4%EC%A0%9C%EB%82%B4%EC%84%B1%EA%B7%A0%EA%B0%90%EC%97%BC%EA%B4%80%EB%A6%AC%EC%A7%80%EC%B9%A8.pdf. (Updated on 14 June 2022).16. Clinical. 2007. Performance standards for antimicrobial susceptibility testing; seventeenth informational supplement. CLSI document M100-S17. Clinical and Laboratory Standards Institute;Wayne: p. 1–362. DOI: 10.1201/9781420014495.ch1. PMCID: PMC2173926.17. Tischendorf J, de Avila RA, Safdar N. 2016; Risk of infection following colonization with carbapenem-resistant Enterobactericeae: a systematic review. Am J Infect Control. 44:539–43. DOI: 10.1016/j.ajic.2015.12.005. PMID: 26899297. PMCID: PMC5262497.
Article18. Ben-David D, Kordevani R, Keller N, Tal I, Marzel A, Gal-Mor O, et al. 2012; Outcome of carbapenem resistant Klebsiella pneumoniae bloodstream infections. Clin Microbiol Infect. 18:54–60. DOI: 10.1111/j.1469-0691.2011.03478.x. PMID: 21722257.
Article19. Bogan C, Kaye KS, Chopra T, Hayakawa K, Pogue JM, Lephart PR, et al. 2014; Outcomes of carbapenem-resistant Enterobacteriaceae isolation: matched analysis. Am J Infect Control. 42:612–20. DOI: 10.1016/j.ajic.2014.02.013. PMID: 24837111.
Article20. Hussein K, Raz-Pasteur A, Finkelstein R, Neuberger A, Shachor-Meyouhas Y, Oren I, et al. 2013; Impact of carbapenem resistance on the outcome of patients' hospital-acquired bacteraemia caused by Klebsiella pneumoniae. J Hosp Infect. 83:307–13. DOI: 10.1016/j.jhin.2012.10.012. PMID: 23313086.
Article21. Ben-David D, Kordevani R, Keller N, Tal I, Marzel A, Gal-Mor O, et al. 2012; Outcome of carbapenem resistant Klebsiella pneumoniae bloodstream infections. Clin Microbiol Infect. 18:54–60. DOI: 10.1111/j.1469-0691.2011.03478.x. PMID: 21722257.
Article22. Borer A, Saidel-Odes L, Eskira S, Nativ R, Riesenberg K, Livshiz-Riven I, et al. 2012; Risk factors for developing clinical infection with carbapenem-resistant Klebsiella pneumoniae in hospital patients initially only colonized with carbapenem-resistant K pneumoniae. Am J Infect Control. 40:421–5. DOI: 10.1016/j.ajic.2011.05.022. PMID: 21906844.
Article23. Jiao Y, Qin Y, Liu J, Li Q, Dong Y, Shang Y, et al. 2015; Risk factors for carbapenem-resistant Klebsiella pneumoniae infection/colonization and predictors of mortality: a retrospective study. Pathog Glob Health. 109:68–74. DOI: 10.1179/2047773215Y.0000000004. PMID: 25707874. PMCID: PMC4455340.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiological Characteristics of Carbapenemase Producing Carbapenem-Resistant Enterobacteriaceae Colonization
- Carbapenem-resistant Enterobacteriaceae in Korea
- The Infinity War: How to Cope with Carbapenem-resistant Enterobacteriaceae
- Carbapenem-Resistant Enterobacteriaceae: Rapid Laboratory Diagnosis and Surveillance Culture for Infection Control
- Identification and infection control of carbapenem-resistant Enterobacterales in intensive care units