J Korean Med Sci.
2022 Jun;37(24):e196. 10.3346/jkms.2022.37.e196.
The Changes in Epidemiology of Imipenem-Resistant Acinetobacter baumannii Bacteremia in a Pediatric Intensive Care Unit for 17 Years
- KMID: 2530507
- DOI: http://doi.org/10.3346/jkms.2022.37.e196
Abstract
- Background
Acinetobacter baumannii infections cause high morbidity and mortality in intensive care unit (ICU) patients. However, there are limited data on the changes of longterm epidemiology of imipenem resistance in A. baumannii bacteremia among pediatric ICU (PICU) patients.
Methods
A retrospective review was performed on patients with A. baumannii bacteremia in PICU of a tertiary teaching hospital from 2000 to 2016. Antimicrobial susceptibility tests, multilocus sequence typing (MLST), and polymerase chain reaction for antimicrobial resistance genes were performed for available isolates.
Results
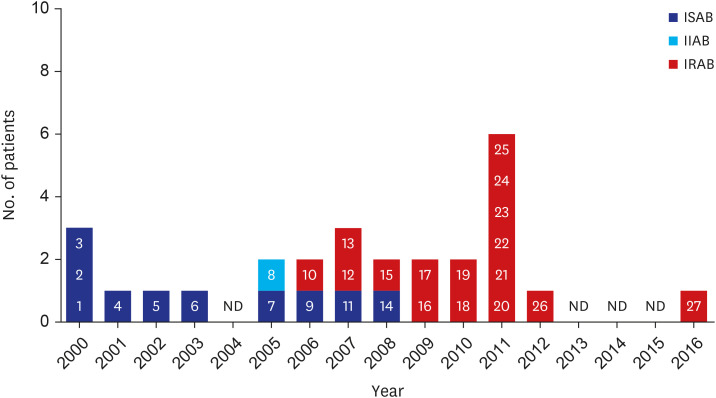
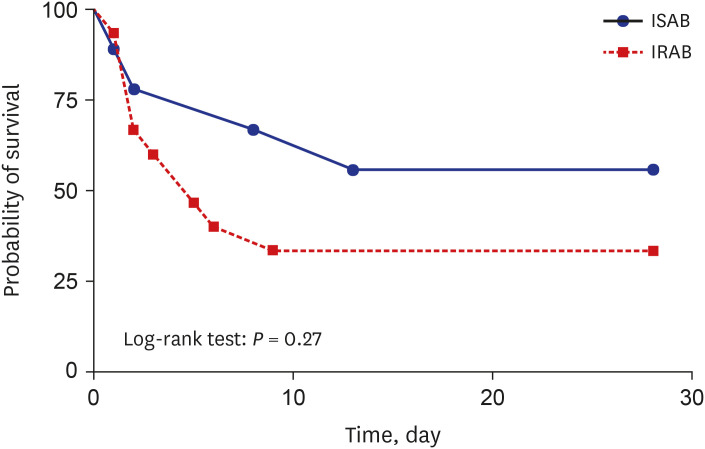
A. baumannii bacteremia occurred in 27 patients; imipenem-sensitive A. baumannii (ISAB, n = 10, 37%) and imipenem-resistant A. baumannii (IRAB, n = 17, 63%). There was a clear shift in the antibiogram of A. baumannii during the study period. From 2000 to 2003, all isolates were ISAB (n = 6). From 2005 to 2008, both IRAB (n = 5) and ISAB (n = 4) were isolated. However, from 2009, all isolates were IRAB (n = 12). Ten isolates were available for additional test and confirmed as IRAB. MLST analysis showed that among 10 isolates, sequence type 138 was predominant (n = 7). All 10 isolates were positive for OXA-23-like and OXA-51-like carbapenemase. Of 27 bacteremia patients, 11 were male (41%), the median age at bacteremia onset was 5.2 years (range, 0–18.6 years). In 33% (9/27) of patients, A. baumannii was isolated from tracheal aspirate prior to development of bacteremia (median, 8 days; range, 5–124 days). The overall case-fatality rate was 63% (17/27) within 28 days. There was no statistical difference in the case fatality rate between ISAB and IRAB groups (50% vs. 71%; P = 0.422).
Conclusion
IRAB bacteremia causes serious threat in patients in PICU. Proactive infection control measures and antimicrobial stewardship are crucial for managing IRAB infection in PICU.
Figure
Cited by 1 articles
-
Clinical Effectiveness of Tetracycline-Class Agents Based Regimens in Patients With Carbapenem-Resistant
Acinetobacter baumannii Bacteremia: A Single-Center Retrospective Cohort Study
Si-Ho Kim, Yu Mi Wi, Kyong Ran Peck
J Korean Med Sci. 2023;38(34):e263. doi: 10.3346/jkms.2023.38.e263.
Reference
-
1. Lakshmi KS, Jayashree M, Singhi S, Ray P. Study of nosocomial primary bloodstream infections in a pediatric intensive care unit. J Trop Pediatr. 2007; 53(2):87–92. PMID: 17151083.
Article2. Le NK, Hf W, Vu PD, Khu DT, Le HT, Hoang BT, et al. High prevalence of hospital-acquired infections caused by Gram-negative carbapenem resistant strains in Vietnamese pediatric ICUs: a multi-centre point prevalence survey. Medicine (Baltimore). 2016; 95(27):e4099. PMID: 27399106.3. Lake JG, Weiner LM, Milstone AM, Saiman L, Magill SS, See I. Pathogen distribution and antimicrobial resistance among pediatric healthcare-associated infections reported to the National Healthcare Safety Network, 2011-2014. Infect Control Hosp Epidemiol. 2018; 39(1):1–11. PMID: 29249216.
Article4. Vila J, Bonomo RA. 46th Interscience Conference on Antimicrobial Agents and Chemotherapy. Future Microbiol. 2007; 2(1):9–12. PMID: 17661671.
Article5. Endo S, Yano H, Hirakata Y, Arai K, Kanamori H, Ogawa M, et al. Molecular epidemiology of carbapenem-non-susceptible Acinetobacter baumannii in Japan. J Antimicrob Chemother. 2012; 67(7):1623–1626. PMID: 22447879.
Article6. Evans BA, Amyes SG. OXA β-lactamases. Clin Microbiol Rev. 2014; 27(2):241–263. PMID: 24696435.
Article7. Lee HY, Hsu SY, Hsu JF, Chen CL, Wang YH, Chiu CH. Risk factors and molecular epidemiology of Acinetobacter baumannii bacteremia in neonates. J Microbiol Immunol Infect. 2018; 51(3):367–376. PMID: 28830746.
Article8. Sultan AM, Seliem WA. Identifying risk factors for healthcare-associated infections caused by carbapenem-resistant Acinetobacter baumannii in a neonatal intensive care unit. Sultan Qaboos Univ Med J. 2018; 18(1):e75–e80. PMID: 29666685.9. Hong KB, Oh HS, Song JS, Lim JH, Kang DK, Son IS, et al. Investigation and control of an outbreak of imipenem-resistant Acinetobacter baumannii infection in a pediatric intensive care unit. Pediatr Infect Dis J. 2012; 31(7):685–690. PMID: 22466324.
Article10. Ko KS, Kuwahara T, Haehwa L, Yoon YJ, Kim BJ, Lee KH, et al. RNA polymerase beta-subunit gene (rpoB) sequence analysis for the identification of Bacteroides spp. Clin Microbiol Infect. 2007; 13(1):48–54. PMID: 17184287.
Article11. La Scola B, Gundi VA, Khamis A, Raoult D. Sequencing of the rpoB gene and flanking spacers for molecular identification of Acinetobacter species. J Clin Microbiol. 2006; 44(3):827–832. PMID: 16517861.
Article12. Clinical and Laboratory Standards Institute (CLSI). CLSI Supplement M100S. Performance Standards for Antimicrobial Susceptibility Testing. 26th ed. Wayne, PA, USA: CLSI;2016.13. Park YK, Choi JY, Jung SI, Park KH, Lee H, Jung DS, et al. Two distinct clones of carbapenem-resistant Acinetobacter baumannii isolates from Korean hospitals. Diagn Microbiol Infect Dis. 2009; 64(4):389–395. PMID: 19631092.
Article14. Public databases for molecular typing and microbial genome diversity. Updated 2022. Accessed September 5, 2021. https://pubmlst.org/bigsdb?db=pubmlst_abaumannii_seqdef&page=profiles .15. Bartual SG, Seifert H, Hippler C, Luzon MA, Wisplinghoff H, Rodríguez-Valera F. Development of a multilocus sequence typing scheme for characterization of clinical isolates of Acinetobacter baumannii . J Clin Microbiol. 2005; 43(9):4382–4390. PMID: 16145081.
Article16. Feil EJ, Smith JM, Enright MC, Spratt BG. Estimating recombinational parameters in Streptococcus pneumoniae from multilocus sequence typing data. Genetics. 2000; 154(4):1439–1450. PMID: 10747043.
Article17. Park YK, Jung SI, Park KH, Kim DH, Choi JY, Kim SH, et al. Changes in antimicrobial susceptibility and major clones of Acinetobacter calcoaceticus-baumannii complex isolates from a single hospital in Korea over 7 years. J Med Microbiol. 2012; 61(Pt 1):71–79. PMID: 21852525.
Article18. Rhomberg PR, Jones RN. Summary trends for the Meropenem Yearly Susceptibility Test Information Collection Program: a 10-year experience in the United States (1999-2008). Diagn Microbiol Infect Dis. 2009; 65(4):414–426. PMID: 19833471.
Article19. Kim D, Ahn JY, Lee CH, Jang SJ, Lee H, Yong D, et al. Increasing resistance to extended-spectrum cephalosporins, fluoroquinolone, and carbapenem in Gram-negative bacilli and the emergence of carbapenem non-susceptibility in Klebsiella pneumoniae: analysis of Korean Antimicrobial Resistance Monitoring System (KARMS) data from 2013 to 2015. Ann Lab Med. 2017; 37(3):231–239. PMID: 28224769.
Article20. Xu A, Zheng B, Xu YC, Huang ZG, Zhong NS, Zhuo C. National epidemiology of carbapenem-resistant and extensively drug-resistant Gram-negative bacteria isolated from blood samples in China in 2013. Clin Microbiol Infect. 2016; 22(Suppl 1):S1–S8. PMID: 26846351.
Article21. Thatrimontrichai A, Apisarnthanarak A, Chanvitan P, Janjindamai W, Dissaneevate S, Maneenil G. Risk factors and outcomes of carbapenem-resistant Acinetobacter baumannii bacteremia in neonatal intensive care unit: a case-case-control study. Pediatr Infect Dis J. 2013; 32(2):140–145. PMID: 22935872.
Article22. Garcia Casallas JC, Robayo-Amortegui H, Corredor-Rozo Z, Carrasco-Márquez AM, Escobar-Perez J. Bacteremia by colistin-resistant Acinetobacter baumannii isolate: a case report. J Med Case Reports. 2019; 13(1):141.23. Jeon H, Kim S, Kim MH, Kim SY, Nam D, Park SC, et al. Molecular epidemiology of carbapenem-resistant Acinetobacter baumannii isolates from a Korean hospital that carry blaOXA-23 . Infect Genet Evol. 2018; 58:232–236. PMID: 29307769.
Article24. Smith CA, Antunes NT, Stewart NK, Toth M, Kumarasiri M, Chang M, et al. Structural basis for carbapenemase activity of the OXA-23 β-lactamase from Acinetobacter baumannii . Chem Biol. 2013; 20(9):1107–1115. PMID: 24012371.
Article25. Karah N, Sundsfjord A, Towner K, Samuelsen Ø. Insights into the global molecular epidemiology of carbapenem non-susceptible clones of Acinetobacter baumannii . Drug Resist Updat. 2012; 15(4):237–247. PMID: 22841809.
Article26. Kim DH, Jung SI, Kwon KT, Ko KS. Occurrence of diverse AbGRI1-type genomic islands in Acinetobacter baumannii global clone 2 isolates from South Korea. Antimicrob Agents Chemother. 2017; 61(2):e01972-16. PMID: 27895018.
Article27. Kim MH, Jeong H, Sim YM, Lee S, Yong D, Ryu CM, et al. Using comparative genomics to understand molecular features of carbapenem-resistant Acinetobacter baumannii from South Korea causing invasive infections and their clinical implications. PLoS One. 2020; 15(2):e0229416. PMID: 32084241.28. Lampati L, Maggioni E, Langer M, Malacarne P, Mozzo R, Pesenti A, et al. Can routine surveillance samples from tracheal aspirate predict bacterial flora in cases of ventilator-associated pneumonia? Minerva Anestesiol. 2009; 75(10):555–562. PMID: 19461563.29. Karageorgopoulos DE, Falagas ME. Current control and treatment of multidrug-resistant Acinetobacter baumannii infections. Lancet Infect Dis. 2008; 8(12):751–762. PMID: 19022191.
Article30. An JH, Kim YH, Moon JE, Jeong JH, Kim SH, Kang SJ, et al. Active surveillance for carbapenem-resistant Acinetobacter baumannii in a medical intensive care unit: can it predict and reduce subsequent infections and the use of colistin? Am J Infect Control. 2017; 45(6):667–672. PMID: 28242072.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multidrug-resistant Acinetobacter baumannii infection in the intensive care unit
- Carbapenem-Resistant Acinetobacter baumannii
- Correlation between Carbapenem Prescription Trends and Imipenem Resistance in Acinetobacter baumannii at an Intensive Care Unit between 2006 and 2010
- Nosocomial Infection by Sequence Type 357 Multidrug-Resistant Acinetobacter baumannii Isolates in a Neonatal Intensive Care Unit in Daejeon, Korea
- Three Cases of Central Nervous System Infection Caused by Multi-Drug-Resistant Acinetobacter baumannii