Nutr Res Pract.
2022 Jun;16(3):379-391. 10.4162/nrp.2022.16.3.379.
Eating away from home is associated with overweight and obesity among Ugandan adults: the 2014 Uganda non-communicable disease risk factor survey
- Affiliations
-
- 1Department of Food Science and Nutrition, Kyungpook National University, Daegu 41566, Korea
- KMID: 2530398
- DOI: http://doi.org/10.4162/nrp.2022.16.3.379
Abstract
- BACKGROUND/OBJECTIVES
We investigated the associations between eating away from home (EAFH) and overweight and obesity among Ugandan adults using the 2014 Uganda non-communicable disease risk factor survey.
SUBJECTS/METHODS
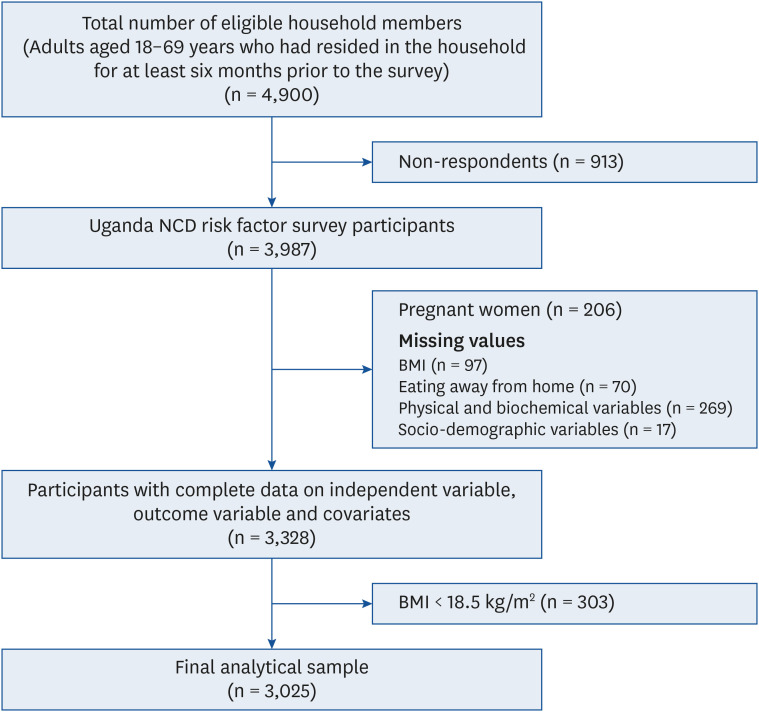
In total, 3,025 participants aged 18–69 years were included in the analysis. The frequency of EAFH was assessed by asking participants the number of meals eaten per week that were not prepared at a home. EAFH frequency was categorized as; less than once/week, 1-2 times/week, or ≥ 3 times/week. Logistic regression was used to evaluate the associations between overweight, obesity, and EAFH. We also tested whether sex and age modified these associations.
RESULTS
Participants that ate away from home ≥ 3 times/week were 2.13 times more likely to be obese than those that ate away from home less than once/week (odds ratio [OR], 2.13; 95% confidence interval [CI], 1.28–3.54). However, when the analysis was stratified by sex, women that ate away from home ≥ 3 times/week were 42% less likely to be overweight than those that ate away from home less than once/week (OR, 0.58; 95% CI, 0.36–0.94). Men that ate away from home ≥ 3 times a week were 3.89 times and 2.23 times more likely to be obese and overweight, respectively, than those that ate away from home less than once/week (obesity: OR, 3.89; 95% CI, 1.50–10.09; overweight: OR, 2.23; 95% CI, 1.42–3.51). Agestratified analysis showed that among participants aged 31–50 years, those that ate away from home ≥ 3 times a week were 3.53 times more likely to be obese than those that ate away from home less than once/week (OR, 3.53; 95% CI, 1.69–7.37).
CONCLUSIONS
Frequent EAFH was positively associated with overweight and obesity among men, and obesity among young/middle-aged adults, but negatively associated with overweight in women. Nutritional interventions for obesity reduction in Uganda should include strategies aimed at reducing the frequency of eating meals prepared away from home, and specifically target men and young/middle-aged adults.
Keyword
Figure
Reference
-
1. Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, Adams RJ, Aekplakorn W, Afsana K, Aguilar-Salinas CA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017; 390:2627–2642. PMID: 29029897.2. Steyn NP, McHiza ZJ. Obesity and the nutrition transition in Sub-Saharan Africa. Ann N Y Acad Sci. 2014; 1311:88–101. PMID: 24725148.3. NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016; 387:1377–1396. PMID: 27115820.4. Mattei J, Malik V, Wedick NM, Campos H, Spiegelman D, Willett W, Hu FB. A symposium and workshop report from the Global Nutrition and Epidemiologic Transition Initiative: nutrition transition and the global burden of type 2 diabetes. Br J Nutr. 2012; 108:1325–1335. PMID: 22863082.5. Cohen DA, Bhatia R. Nutrition standards for away-from-home foods in the USA. Obes Rev. 2012; 13:618–629. PMID: 22329431.6. Ayo AS, Sserunkuuma D, Bonabana-Wabbi J. Determinants of fast-food consumption in Kampala, Uganda. Afr J Food Agric Nutr Dev. 2012; 12:6567–6581.7. Uganda Ministry of Health. Non Communicable Disease Risk Factor Baseline Survey 2014 [Internet]. Kampala: Uganda Ministry of Health;2014. cited 2021 April 21. Available from: https://www.health.go.ug/cause/non-communicable-disease-risk-factor-baseline-survey/.8. Sseguya W, Matovu N, Swann J, Draper A. Contribution of street food to dietary intake of habitual urban consumers: a cross-sectional study in Kampala city, Uganda. Nutr Health. 2020; 26:187–195. PMID: 32329392.9. Bezerra IN, Sichieri R. Eating out of home and obesity: a Brazilian nationwide survey. Public Health Nutr. 2009; 12:2037–2043. PMID: 19433008.10. Bezerra IN, Curioni C, Sichieri R. Association between eating out of home and body weight. Nutr Rev. 2012; 70:65–79. PMID: 22300594.11. Nago ES, Lachat CK, Dossa RA, Kolsteren PW. Association of out-of-home eating with anthropometric changes: a systematic review of prospective studies. Crit Rev Food Sci Nutr. 2014; 54:1103–1116. PMID: 24499144.12. Bhutani S, Schoeller DA, Walsh MC, McWilliams C. Frequency of eating out at both fast-food and sit-down restaurants was associated with high body mass index in non-large metropolitan communities in Midwest. Am J Health Promot. 2018; 32:75–83. PMID: 27574335.13. Orfanos P, Naska A, Trichopoulos D, Slimani N, Ferrari P, van Bakel M, Deharveng G, Overvad K, Tjønneland A, Halkjaer J, et al. Eating out of home and its correlates in 10 European countries. The European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2007; 10:1515–1525. PMID: 17582244.14. Guwatudde D, Mutungi G, Wesonga R, Kajjura R, Kasule H, Muwonge J, Ssenono V, Bahendeka SK. The epidemiology of hypertension in Uganda: findings from the national non-communicable diseases risk factor survey. PLoS One. 2015; 10:e0138991. PMID: 26406462.15. Bahendeka S, Wesonga R, Mutungi G, Muwonge J, Neema S, Guwatudde D. Prevalence and correlates of diabetes mellitus in Uganda: a population-based national survey. Trop Med Int Health. 2016; 21:405–416. PMID: 26729021.16. Wesonga R, Guwatudde D, Bahendeka SK, Mutungi G, Nabugoomu F, Muwonge J. Burden of cumulative risk factors associated with non-communicable diseases among adults in Uganda: evidence from a national baseline survey. Int J Equity Health. 2016; 15:195. PMID: 27905949.17. World Health Organization. A Framework for Surveillance The WHO STEPwise Approach to Surveillance of Noncommunicable Diseases (STEPS). Geneva: World Health Organization;2003.18. World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation (WHO Technical Report Series 894) [Internet]. Geneva: World Health Organization;2000. cited 2021 May 25. Available from: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/.19. World Health Organization. Global Physical Activity Questionnaire Global Physical Activity Questionnaire (GPAQ) [Internet]. Geneva: World Health Organization;2021. cited 2021 August 16. Available from: www.who.int/chp/steps.20. World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Technical Report Series No. 854. Technical Report Series No. 854. Geneva: World Health Organization;1995.21. U.S. Department of Health and Human Services, U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans [Internet]. Washington, D.C.: U.S. Department of Health and Human Services, U.S. Department of Agriculture;2015. cited 2021 April 21. Available from: http://health.gov/dietaryguidelines/2015/guidelines/.22. Seguin RA, Aggarwal A, Vermeylen F, Drewnowski A. Consumption frequency of foods away from home linked with higher body mass index and lower fruit and vegetable intake among adults: a cross-sectional study. J Environ Public Health. 2016; 2016:3074241. PMID: 26925111.23. Popkin BM, Hawkes C. Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 2016; 4:174–186. PMID: 26654575.24. Hall KD, Guo J, Dore M, Chow CC. The progressive increase of food waste in America and its environmental impact. PLoS One. 2009; 4:e7940. PMID: 19946359.25. Heymsfield SB, Wadden TA. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med. 2017; 376:254–266. PMID: 28099824.26. Lachat C, Nago E, Verstraeten R, Roberfroid D, Van Camp J, Kolsteren P. Eating out of home and its association with dietary intake: a systematic review of the evidence. Obes Rev. 2012; 13:329–346. PMID: 22106948.27. Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008; 9:535–547. PMID: 18346099.28. Namugumya BS, Muyanja C. Contribution of street foods to the dietary needs of street food vendors in Kampala, Jinja and Masaka districts, Uganda. Public Health Nutr. 2012; 15:1503–1511. PMID: 22015148.29. van’t Riet H, den Hartog AP, van Staveren WA. Non-home prepared foods: contribution to energy and nutrient intake of consumers living in two low-income areas in Nairobi. Public Health Nutr. 2002; 5:515–522. PMID: 12186659.30. Wolfson JA, Bleich SN. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutr. 2015; 18:1397–1406. PMID: 25399031.31. Larson NI, Perry CL, Story M, Neumark-Sztainer D. Food preparation by young adults is associated with better diet quality. J Am Diet Assoc. 2006; 106:2001–2007. PMID: 17126631.32. Choi MK, Kim TY, Yoon JS. Does frequent eating out cause undesirable food choices? Association of food away from home with food consumption frequencies and obesity among Korean housewives. Ecol Food Nutr. 2011; 50:263–280. PMID: 21888582.33. French SA, Harnack L, Jeffery RW. Fast food restaurant use among women in the Pound of Prevention study: dietary, behavioral and demographic correlates. Int J Obes Relat Metab Disord. 2000; 24:1353–1359. PMID: 11093299.34. Heng HL, Guan AT. Factors affecting Malaysian household purchase decisions of food-away-from-home. J Int Food Agribus Mark. 2007; 19:97–115.35. van ’t Riet H, den Hartog AP, Mwangi AM, Mwadime RK, Foeken DW, van Staveren WA. The role of street foods in the dietary pattern, of two low-income groups in Nairobi. Eur J Clin Nutr. 2001; 55:562–570. PMID: 11464230.36. van ’t Riet H, den Hartog AP, Hooftman DA, Foeken DW, van Staveren WA, Van Staveren WA. Determinants of non-home-prepared food consumption in two low-income areas in Nairobi. Nutrition. 2003; 19:1006–1012. PMID: 14624955.37. Larson N, Neumark-Sztainer D, Laska MN, Story M. Young adults and eating away from home: associations with dietary intake patterns and weight status differ by choice of restaurant. J Am Diet Assoc. 2011; 111:1696–1703. PMID: 22027052.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Away-from-Home Eating and Dietary Patterns of Ugandan Adults: a Web-based- Survey
- The Paradox of the Ugandan Health Insurance System: Challenges and Opportunities for Health Reform
- Factors Affecting Obesity and Overweight in Korean Preschool Children: Based on the Korea National Health and Nutrition Examination Survey 2013-2014
- Management of Overweight and Obesity: Review of the "2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults"
- The double burden of malnutrition among adults in India: evidence from the National Family Health Survey-4 (2015-16)