Korean J Gastroenterol.
2022 May;79(5):217-221. 10.4166/kjg.2022.034.
Liver Graft Failure after Plastic Stent Removal of an Anastomotic Biliary Stricture
- Affiliations
-
- 1Center for Liver and Pancreatobiliary Cancer, Research Institute and Hospital, National Cancer Center, Goyang
- 2Departments of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Departments of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 4Internal Medicine and Liver Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2530329
- DOI: http://doi.org/10.4166/kjg.2022.034
Abstract
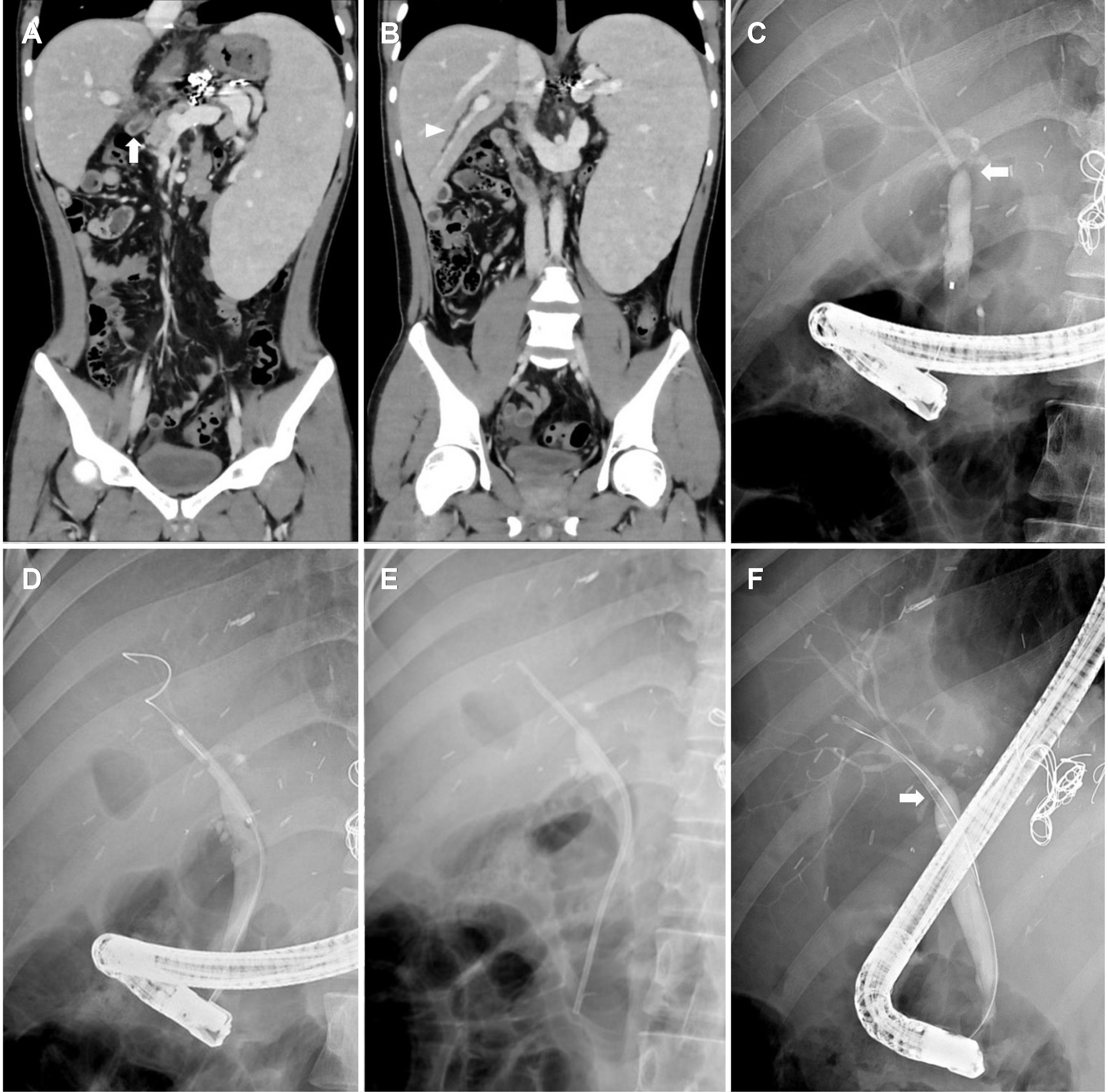
- A biliary anastomotic stricture developed 13 months after living donor liver transplantation in a 19-year-old male with congenital hepatic fibrosis. Endoscopic management with balloon dilation followed by the placement of a 7F plastic stent was performed for the anastomotic stricture. After 6 months of indwelling of the stent, the plastic stent was removed because the stenosis and cholestasis were improved. One month after stent removal, he was admitted for acute liver graft failure owing to cholestatic hepatitis, and required retransplantation secondary to graft loss.
Figure
Reference
-
1. Tsujino T, Isayama H, Kogure H, Sato T, Nakai Y, Koike K. 2017; Endoscopic management of biliary strictures after living donor liver transplantation. Clin J Gastroenterol. 10:297–311. DOI: 10.1007/s12328-017-0754-z. PMID: 28600688.
Article2. Villa NA, Harrison ME. 2015; Management of biliary strictures after liver transplantation. Gastroenterol Hepatol (N Y). 11:316–328.3. Sharma S, Gurakar A, Jabbour N. 2008; Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl. 14:759–769. DOI: 10.1002/lt.21509. PMID: 18508368.
Article4. Williams ED, Draganov PV. 2009; Endoscopic management of biliary strictures after liver transplantation. World J Gastroenterol. 15:3725–3733. DOI: 10.3748/wjg.15.3725. PMID: 19673012. PMCID: PMC2726449.
Article5. Liu CL, Fan ST, Lo CM, et al. 2006; Operative outcomes of adult-to-adult right lobe live donor liver transplantation: a comparative study with cadaveric whole-graft liver transplantation in a single center. Ann Surg. 243:404–410. DOI: 10.1097/01.sla.0000201544.36473.a2. PMID: 16495707. PMCID: PMC1448929.
Article6. Gómez CM, Dumonceau JM, Marcolongo M, et al. 2009; Endoscopic management of biliary complications after adult living-donor versus deceased-donor liver transplantation. Transplantation. 88:1280–1285. DOI: 10.1097/TP.0b013e3181bb48c2. PMID: 19996927.
Article7. Ayoub WS, Esquivel CO, Martin P. 2010; Biliary complications following liver transplantation. Dig Dis Sci. 55:1540–1546. DOI: 10.1007/s10620-010-1217-2. PMID: 20411422.
Article8. You MS, Paik WH, Choi YH, et al. 2019; Optimal biliary drainage for patients with biliary anastomotic strictures after right lobe living donor liver transplantation. Liver Transpl. 25:1209–1219. DOI: 10.1002/lt.25472. PMID: 30980451.
Article9. Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. 2001; Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 54:162–168. DOI: 10.1067/mge.2001.116876. PMID: 11474384.
Article10. Seo JK, Ryu JK, Lee SH, et al. 2009; Endoscopic treatment for biliary stricture after adult living donor liver transplantation. Liver Transpl. 15:369–380. DOI: 10.1002/lt.21700. PMID: 19326412.
Article11. Pasha SF, Harrison ME, Das A, et al. 2007; Endoscopic treatment of anastomotic biliary strictures after deceased donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc. 66:44–51. DOI: 10.1016/j.gie.2007.02.017. PMID: 17591473.
Article12. Srinath A, Shneider BL. 2012; Congenital hepatic fibrosis and autosomal recessive polycystic kidney disease. J Pediatr Gastroenterol Nutr. 54:580–587. DOI: 10.1097/MPG.0b013e31824711b7. PMID: 22197937. PMCID: PMC4369775.
Article13. Habib S, Shakil O, Couto OF, et al. 2006; Caroli's disease and orthotopic liver transplantation. Liver Transpl. 12:416–421. DOI: 10.1002/lt.20719. PMID: 16498655.
Article14. Alazmi WM, Fogel EL, Watkins JL, et al. 2006; Recurrence rate of anastomotic biliary strictures in patients who have had previous successful endoscopic therapy for anastomotic narrowing after orthotopic liver transplantation. Endoscopy. 38:571–574. DOI: 10.1055/s-2006-925027. PMID: 16802268.
Article15. Kashyap R, Jain A, Reyes J, et al. 2001; Causes of retransplantation after primary liver transplantation in 4000 consecutive patients: 2 to 19 years follow-up. Transplant Proc. 33:1486–1487. DOI: 10.1016/S0041-1345(00)02563-X.
Article16. Chen GH, Fu BS, Cai CJ, et al. 2008; A single-center experience of retransplantation for liver transplant recipients with a failing graft. Transplant Proc. 40:1485–1487. DOI: 10.1016/j.transproceed.2008.01.076. PMID: 18589134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case with combined postoperative bile leakage and anastomotic stricture after liver transplantation treated with magnet compression anastomosis
- Temporary Placement of Stent Grafts in Postsurgical Benign Biliary Strictures: a Single Center Experience
- Endoscopic Management of Anastomotic Strictures after Liver Transplantation
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Anastomotic stricture after liver transplantation: It is not Achilles' heel anymore!