Diabetes Metab J.
2022 May;46(3):499-505. 10.4093/dmj.2021.0059.
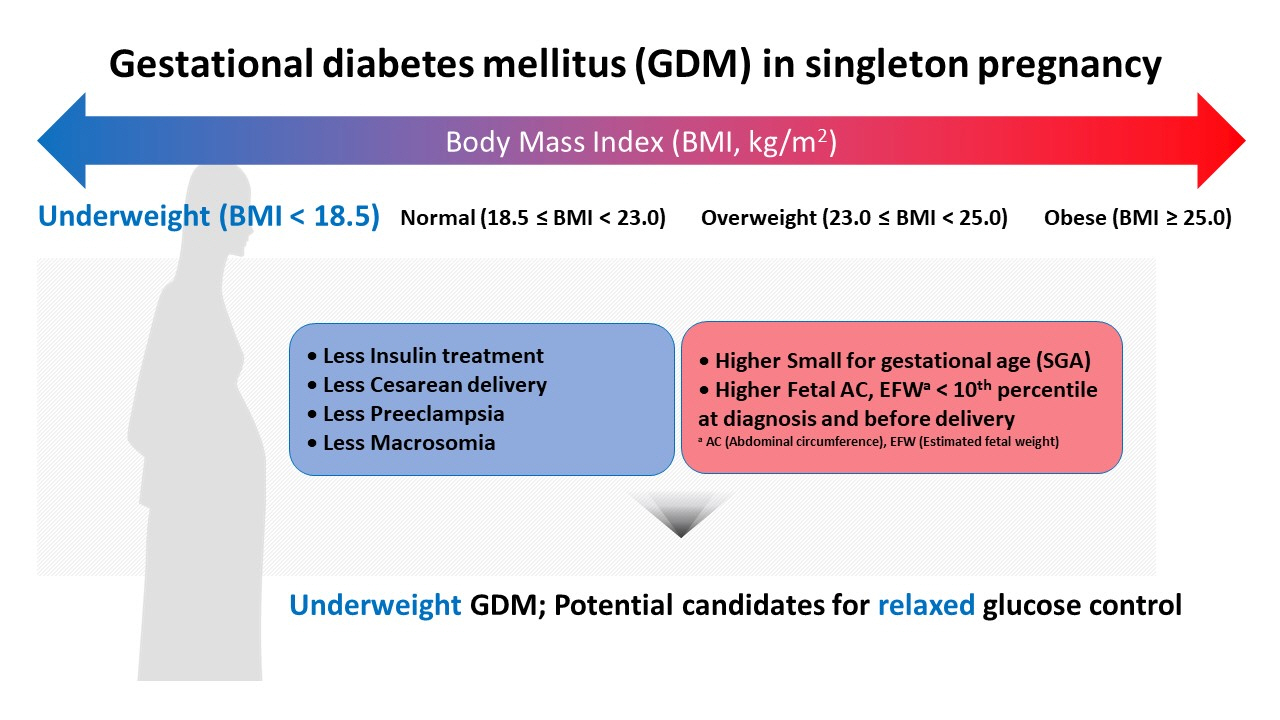
Influence of Pre-Pregnancy Underweight Body Mass Index on Fetal Abdominal Circumference, Estimated Weight, and Pregnancy Outcomes in Gestational Diabetes Mellitus
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2530188
- DOI: http://doi.org/10.4093/dmj.2021.0059
Abstract
- This study aimed to determine the influence of pre-pregnancy body mass index on pregnancy outcomes in gestational diabetes mellitus (GDM), comparing underweight patients with GDM with normal weight patients with GDM. Maternal baseline characteristics, ultrasonographic results, and pregnancy and neonatal outcomes were reviewed in 946 women with GDM with singleton pregnancies. Underweight patients with GDM showed a benign course in most aspects during pregnancy, except for developing a higher risk of giving birth to small for gestational age neonates. Underweight women with GDM required less insulin treatment, had a higher rate of vaginal delivery, and had a lower rate of cesarean delivery. In addition, their neonates were more likely to have fetal abdominal circumference and estimated fetal weight below the 10th percentile both at the time of GDM diagnosis and before delivery. Notably, their risk for preeclampsia and macrosomia were lower. Collectively, our data suggest that underweight women with GDM may require a different approach in terms of diagnosis and management throughout their pregnancy.
Keyword
Figure
Reference
-
1. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: preeclampsia. Am J Obstet Gynecol. 2010; 202:255.2. Vaarasmaki M. Is it worth treating gestational diabetes: if so, when and how? Diabetologia. 2016; 59:1391–5.
Article3. Langer O, Levy J, Brustman L, Anyaegbunam A, Merkatz R, Divon M. Glycemic control in gestational diabetes mellitus: how tight is tight enough: small for gestational age versus large for gestational age? Am J Obstet Gynecol. 1989; 161:646–53.4. Kjos SL, Schaefer-Graf U, Sardesi S, Peters RK, Buley A, Xiang AH, et al. A randomized controlled trial using glycemic plus fetal ultrasound parameters versus glycemic parameters to determine insulin therapy in gestational diabetes with fasting hyperglycemia. Diabetes Care. 2001; 24:1904–10.
Article5. Yogev Y, Langer O. Pregnancy outcome in obese and morbidly obese gestational diabetic women. Eur J Obstet Gynecol Reprod Biol. 2008; 137:21–6.
Article6. Buchanan TA, Kjos SL, Schafer U, Peters RK, Xiang A, Byrne J, et al. Utility of fetal measurements in the management of gestational diabetes mellitus. Diabetes Care. 1998; 21(Suppl 2):B99–106.7. Kim M, Park J, Kim SH, Kim YM, Yee C, Choi SJ, et al. The trends and risk factors to predict adverse outcomes in gestational diabetes mellitus: a 10-year experience from 2006 to 2015 in a single tertiary center. Obstet Gynecol Sci. 2018; 61:309–18.
Article8. Katon J, Reiber G, Williams MA, Yanez D, Miller E. Weight loss after diagnosis with gestational diabetes and birth weight among overweight and obese women. Matern Child Health J. 2013; 17:374–83.
Article9. Kurtzhals LL, Norgaard SK, Secher AL, Nichum VL, Ronneby H, Tabor A, et al. The impact of restricted gestational weight gain by dietary intervention on fetal growth in women with gestational diabetes mellitus. Diabetologia. 2018; 61:2528–38.
Article10. Zheng W, Huang W, Liu C, Yan Q, Zhang L, Tian Z, et al. Weight gain after diagnosis of gestational diabetes mellitus and its association with adverse pregnancy outcomes: a cohort study. BMC Pregnancy Childbirth. 2021; 21:216.
Article11. Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011; 364:719–29.12. Roman AS, Rebarber A, Fox NS, Klauser CK, Istwan N, Rhea D, et al. The effect of maternal obesity on pregnancy outcomes in women with gestational diabetes. J Matern Fetal Neonatal Med. 2011; 24:723–7.
Article13. Quevedo SF, Bovbjerg ML, Kington RL. Translation of fetal abdominal circumference-guided therapy of gestational diabetes complicated by maternal obesity to a clinical outpatient setting. J Matern Fetal Neonatal Med. 2017; 30:1450–5.
Article14. Kjos SL, Schaefer-Graf UM. Modified therapy for gestational diabetes using high-risk and low-risk fetal abdominal circumference growth to select strict versus relaxed maternal glycemic targets. Diabetes Care. 2007; 30(Suppl 2):S200–5.
Article15. Metzger BE, Buchanan TA, Coustan DR, de Leiva A, Dunger DB, Hadden DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care. 2007; 30(Suppl 2):S251–60.
Article16. Dooley SL, Metzger BE, Cho NH. Gestational diabetes mellitus: influence of race on disease prevalence and perinatal outcome in a U.S. population. Diabetes. 1991; 40(Suppl 2):25–9.
Article17. Schaefer-Graf UM, Kjos SL, Fauzan OH, Buhling KJ, Siebert G, Buhrer C, et al. A randomized trial evaluating a predominantly fetal growth-based strategy to guide management of gestational diabetes in Caucasian women. Diabetes Care. 2004; 27:297–302.
Article18. Bonomo M, Cetin I, Pisoni MP, Faden D, Mion E, Taricco E, et al. Flexible treatment of gestational diabetes modulated on ultrasound evaluation of intrauterine growth: a controlled randomized clinical trial. Diabetes Metab. 2004; 30:237–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Obesity on Pregnancy Outcomes
- Gestational Diabetes in Korea: Incidence and Risk Factors of Diabetes in Women with Previous Gestational Diabetes
- Determinants of Infant Birthweight
- Perinatal outcomes associated with prepregnancy body mass index and weight gain during pregnancy
- The trends and risk factors to predict adverse outcomes in gestational diabetes mellitus: a 10-year experience from 2006 to 2015 in a single tertiary center