Clin Endosc.
2022 May;55(3):401-407. 10.5946/ce.2021.197.
Endoscopic internal drainage with double pigtail stents for upper gastrointestinal anastomotic leaks: suitable for all cases?
- Affiliations
-
- 1Upper Gastrointestinal and Bariatric Service, Department of General Surgery, Sengkang General Hospital, Singapore, Singapore
- 2Department of Upper Gastrointestinal and Bariatric Surgery, Singapore General Hospital, Singapore, Singapore
- KMID: 2529962
- DOI: http://doi.org/10.5946/ce.2021.197
Abstract
- Background/Aims
Surgeons and endoscopists have started to use endoscopically inserted double pigtail stents (DPTs) in the management of upper gastrointestinal (UGI) leaks, including UGI anastomotic leaks. We investigated our own experiences in this patient population.
Methods
From March 2017 to June 2020, 12 patients had endoscopic internal drainage of a radiologically proven anastomotic leak after UGI surgery in two tertiary UGI centers. The primary outcome measure was the time to removal of the DPTs after anastomotic healing. The secondary outcome measure was early oral feeding after DPT insertion.
Results
Eight of the 12 patients (67%) required only one DPT, whereas four (33%) required two DPTs. The median duration of drainage was 42 days. Two patients required surgery due to inadequate control of sepsis. Of the remaining 10 patients, nine did not require a change in DPT before anastomotic healing. Nine patients were allowed oral fluids within the 1st week and a soft diet in the 2nd week. One patient was allowed clear oral feeds on the 8th day after DPT insertion.
Conclusions
Endoscopic internal drainage is becoming an established minimally invasive technique for controlling anastomotic leak after UGI surgery. It allows for early oral nutritional feeding and minimizes discomfort from conventional external drainage.
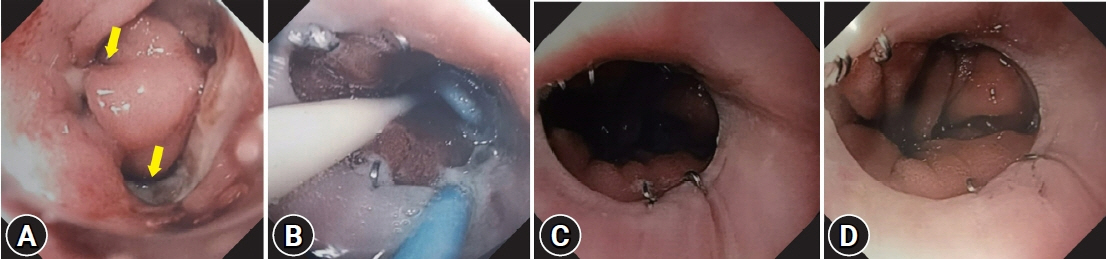
Figure
Reference
-
1. Lang H, Piso P, Stukenborg C, et al. Management and results of proximal anastomotic leaks in a series of 1114 total gastrectomies for gastric carcinoma. Eur J Surg Oncol. 2000; 26:168–171.2. Oh SJ, Choi WB, Song J, et al. Complications requiring reoperation after gastrectomy for gastric cancer: 17 years experience in a single institute. J Gastrointest Surg. 2009; 13:239–245.3. Carboni F, Valle M, Federici O, et al. Esophagojejunal anastomosis leakage after total gastrectomy for esophagogastric junction adenocarcinoma: options of treatment. J Gastrointest Oncol. 2016; 7:515–522.4. Yoo HM, Lee HH, Shim JH, et al. Negative impact of leakage on survival of patients undergoing curative resection for advanced gastric cancer. J Surg Oncol. 2011; 104:734–740.5. Li QG, Li P, Tang D, et al. Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World J Gastroenterol. 2013; 19:4060–4065.6. Rizk NP, Bach PB, Schrag D, et al. The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg. 2004; 198:42–50.7. Rogalski P, Daniluk J, Baniukiewicz A, et al. Endoscopic management of gastrointestinal perforations, leaks and fistulas. World J Gastroenterol. 2015; 21:10542–10552.8. Bemelman WA, Baron TH. Endoscopic management of transmural defects, including leaks, perforations, and fistulae. Gastroenterology. 2018; 154:1938–1946.e1.9. Kahler G. Anastomotic leakage after upper gastrointestinal surgery: endoscopic treatment. Visc Med. 2017; 33:202–206.10. Willingham FF, Buscaglia JM. Endoscopic management of gastrointestinal leaks and fistulae. Clin Gastroenterol Hepatol. 2015; 13:1714–1721.11. Hummel R, Bausch D. Anastomotic leakage after upper gastrointestinal surgery: surgical treatment. Visc Med. 2017; 33:207–211.12. Talbot M, Yee G, Saxena P. Endoscopic modalities for upper gastrointestinal leaks, fistulae and perforations. ANZ J Surg. 2017; 87:171–176.13. Tan JT, Kariyawasam S, Wijeratne T, et al. Diagnosis and management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010; 20:403–409.14. Johnson MD, Walsh RM, Henderson JM, et al. Surgical versus nonsurgical management of pancreatic pseudocysts. J Clin Gastroenterol. 2009; 43:586–590.15. Akshintala VS, Saxena P, Zaheer A, et al. A comparative evaluation of outcomes of endoscopic versus percutaneous drainage for symptomatic pancreatic pseudocysts. Gastrointest Endosc. 2014; 79:921–928.16. Varadarajulu S, Bang JY, Sutton BS, et al. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology. 2013; 145:583–590.e1.17. Foo JW, Balshaw J, Tan MH, et al. Leaks in fixed-ring banded sleeve gastrectomies: a management approach. Surg Obes Relat Dis. 2017; 13:1259–1264.18. Donatelli G, Dumont JL, Cereatti F, et al. Treatment of leaks following sleeve gastrectomy by endoscopic internal drainage (EID). Obes Surg. 2015; 25:1293–1301.19. Donatelli G, Dumont JL, Cereatti F, et al. Endoscopic internal drainage as first-line treatment for fistula following gastrointestinal surgery: a case series. Endosc Int Open. 2016; 4:E647–E651.20. Lorenzo D, Guilbaud T, Gonzalez JM, et al. Endoscopic treatment of fistulas after sleeve gastrectomy: a comparison of internal drainage versus closure. Gastrointest Endosc. 2018; 87:429–437.21. Rodrigues-Pinto E, Pereira P, Sousa-Pinto B, et al. Retrospective multicenter study on endoscopic treatment of upper GI postsurgical leaks. Gastrointest Endosc. 2021; 93:1283–1299.e2.22. Jung CF, Hallit R, Muller-Dornieden A, et al. Endoscopic internal drainage and low negative-pressure endoscopic vacuum therapy for anastomotic leaks after oncologic upper gastrointestinal surgery. Endoscopy. 2022; 54:71–74.23. Still S, Mencio M, Ontiveros E, et al. Primary and rescue endoluminal vacuum therapy in the management of esophageal perforations and leaks. Ann Thorac Cardiovasc Surg. 2018; 24:173–179.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic management of postsurgical leaks
- Stent occlusion in endoscopic ultrasound-guided gallbladder drainage from bleeding mitigated by double pigtail plastic stent deployment within lumen apposing metal stent
- Enteral stents in the management of gastrointestinal leaks, perforations and fistulae
- A Gastrobronchial Fistula Secondary to Endoscopic Internal Drainage of a Post-Sleeve Gastrectomy Fluid Collection
- Endoscopic treatment of upper gastrointestinal postsurgical leaks: a narrative review