J Korean Med Sci.
2022 May;37(18):e134. 10.3346/jkms.2022.37.e134.
Risk Factors for Coronavirus Disease 2019 (COVID-19)-Associated Pulmonary Aspergillosis in Critically Ill Patients: A Nationwide, Multicenter, Retrospective Cohort Study
- Affiliations
-
- 1Division of Infectious Diseases, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 2Division of Infectious Diseases, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Infectious Diseases, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Division of Infectious Diseases, Department of Internal Medicine, Dong-A University Hospital, Busan, Korea
- 5Division of Infectious Diseases, Department of Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 6Division of Infectious Diseases, Department of Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 7Division of Infectious Diseases, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 8Department of Internal Medicine, Jeju National University College of Medicine, Jeju, South Korea
- 9Division of Infectious Diseases, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 10Division of Infectious Diseases, Department of Medicine, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- 11Division of Infectious Diseases, Department of Internal Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 12Division of Infectious Diseases, Department of Internal Medicine, Chungnam National University School of Medicine, Daejeon, Korea
- 13Division of Infectious Diseases, Department of Internal Medicine, Chung-Ang University Hospital, Seoul, Korea
- KMID: 2529708
- DOI: http://doi.org/10.3346/jkms.2022.37.e134
Abstract
- Background
Coronavirus disease 2019 (COVID-19) is often accompanied by secondary infections, such as invasive aspergillosis. In this study, risk factors for developing COVID-19-associated pulmonary aspergillosis (CAPA) and their clinical outcomes were evaluated.
Methods
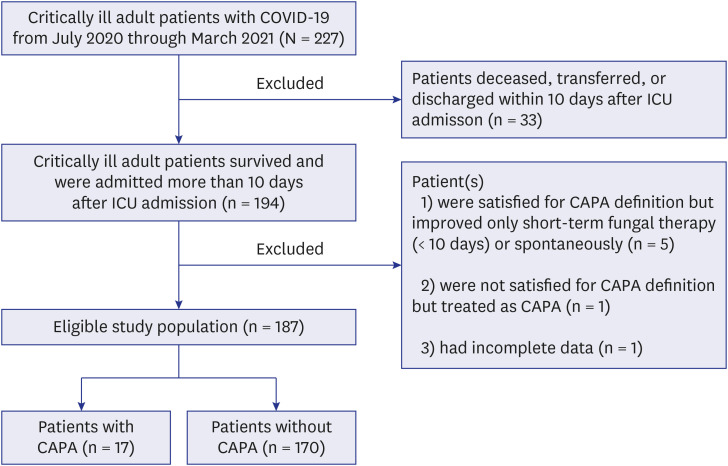
This multicenter retrospective cohort study included critically ill COVID-19 patients from July 2020 through March 2021. Critically ill patients were defined as patients requiring high-flow respiratory support or mechanical ventilation. CAPA was defined based on the 2020 European Confederation of Medical Mycology and the International Society for Human and Animal Mycology consensus criteria. Factors associated with CAPA were analyzed, and their clinical outcomes were adjusted by a propensity score-matched model.
Results
Among 187 eligible patients, 17 (9.1%) developed CAPA, which is equal to 33.10 per 10,000 patient-days. Sixteen patients received voriconazole-based antifungal treatment. In addition, 82.4% and 53.5% of patients with CAPA and without CAPA, respectively, received early high-dose corticosteroids (P = 0.022). In multivariable analysis, initial 10-day cumulative steroid dose > 60 mg of dexamethasone or dexamethasone equivalent dose) (adjusted odds ratio [OR], 3.77; 95% confidence interval [CI], 1.03–13.79) and chronic pulmonary disease (adjusted OR, 4.20; 95% CI, 1.26–14.02) were independently associated with CAPA. Tendencies of higher 90-day overall mortality (54.3% vs. 35.2%, P= 0.346) and lower respiratory support-free rate were observed in patients with CAPA (76.3% vs. 54.9%, P = 0.089).
Conclusion
Our study showed that the dose of corticosteroid use might be a risk factor for CAPA development and the possibility of CAPA contributing to adverse outcomes in critically ill COVID-19 patients.
Keyword
Figure
Reference
-
1. World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 2022. Accessed March 12, 2022. https://covid19.who.int/ .2. Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020; 26(7):1017–1032. PMID: 32651579.3. Koehler P, Bassetti M, Chakrabarti A, Chen SC, Colombo AL, Hoenigl M, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2021; 21(6):e149–e162. PMID: 33333012.4. Heard KL, Hughes S, Mughal N, Moore LS. COVID-19 and fungal superinfection. Lancet Microbe. 2020; 1(3):e107. PMID: 32835341.5. Schauwvlieghe AF, Rijnders BJ, Philips N, Verwijs R, Vanderbeke L, Van Tienen C, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med. 2018; 6(10):782–792. PMID: 30076119.6. Ajmal S, Mahmood M, Abu Saleh O, Larson J, Sohail MR. Invasive fungal infections associated with prior respiratory viral infections in immunocompromised hosts. Infection. 2018; 46(4):555–558. PMID: 29627936.7. Verweij PE, Rijnders BJ, Brüggemann RJ, Azoulay E, Bassetti M, Blot S, et al. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: an expert opinion. Intensive Care Med. 2020; 46(8):1524–1535. PMID: 32572532.8. Salmanton-García J, Sprute R, Stemler J, Bartoletti M, Dupont D, Valerio M, et al. COVID-19-associated pulmonary aspergillosis, March-August 2020. Emerg Infect Dis. 2021; 27(4):1077–1086. PMID: 33539721.9. Lahmer T, Kriescher S, Herner A, Rothe K, Spinner CD, Schneider J, et al. Invasive pulmonary aspergillosis in critically ill patients with severe COVID-19 pneumonia: results from the prospective AspCOVID-19 study. PloS One. 2021; 16(3):e0238825. PMID: 33730058.10. Permpalung N, Chiang TP, Massie AB, Zhang SX, Avery RK, Nematollahi S, et al. Coronavirus disease 2019–associated pulmonary aspergillosis in mechanically ventilated patients. Clin Infect Dis. 2022; 74(1):83–91. PMID: 33693551.11. Bartoletti M, Pascale R, Cricca M, Rinaldi M, Maccaro A, Bussini L, et al. Epidemiology of invasive pulmonary aspergillosis among intubated patients with COVID-19: a prospective study. Clin Infect Dis. 2021; 73(11):e3606–e3614. PMID: 32719848.12. Prattes J, Wauters J, Giacobbe DR, Salmanton-García J, Maertens J, Bourgeois M, et al. Risk factors and outcome of pulmonary aspergillosis in critically ill coronavirus disease 2019 patients-a multinational observational study by the European Confederation of Medical Mycology. Clin Microbiol Infect. 2022; 28(4):580–587. PMID: 34454093.13. Dellière S, Dudoignon E, Fodil S, Voicu S, Collet M, Oillic PA, et al. Risk factors associated with COVID-19-associated pulmonary aspergillosis in ICU patients: a French multicentric retrospective cohort. Clin Microbiol Infect. 2020; 27(5):790.e1–790.e5.14. National Institutes of Health. COVID-19 treatment guidelines panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. Updated 2022. Accessed September 18, 2021. https://www.covid19treatmentguidelines.nih.gov/ .15. Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020; 39(5):405–407. PMID: 32362390.16. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021; 384(8):693–704. PMID: 32678530.17. Tomazini BM, Maia IS, Cavalcanti AB, Berwanger O, Rosa RG, Veiga VC, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA. 2020; 324(13):1307–1316. PMID: 32876695.18. Munch MW, Myatra SN, Vijayaraghavan BK, Saseedharan S, Benfield T, Wahlin RR, et al. Effect of 12 mg vs 6 mg of dexamethasone on the number of days alive without life support in adults with COVID-19 and severe hypoxemia: the COVID STEROID 2 randomized trial. JAMA. 2021; 326(18):1807–1817. PMID: 34673895.19. White PL, Dhillon R, Cordey A, Hughes H, Faggian F, Soni S, et al. A national strategy to diagnose coronavirus disease 2019-associated invasive fungal disease in the intensive care Unit. Clin Infect Dis. 2021; 73(7):e1634–e1644. PMID: 32860682.20. Blot SI, Taccone FS, Van den Abeele AM, Bulpa P, Meersseman W, Brusselaers N, et al. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Am J Respir Crit Care Med. 2012; 186(1):56–64. PMID: 22517788.21. Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, et al. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin Infect Dis. 2020; 71(6):1367–1376. PMID: 31802125.22. Chong WH, Saha BK, Neu KP. Comparing the clinical characteristics and outcomes of COVID-19-associate pulmonary aspergillosis (CAPA): a systematic review and meta-analysis. Infection. 2022; 50(1):43–56. PMID: 34570355.23. Lionakis MS, Kontoyiannis DP. Glucocorticoids and invasive fungal infections. Lancet. 2003; 362(9398):1828–1838. PMID: 14654323.24. Liu Y, Li Y, Xu D, Zhang J, Peng Z. Severe COVID-19: immunosuppression or hyperinflammation? Shock. 2021; 56(2):188–199. PMID: 33443366.25. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020; 130(5):2620–2629. PMID: 32217835.26. Fu Y, Cheng Y, Wu Y. Understanding SARS-CoV-2-mediated inflammatory responses: from mechanisms to potential therapeutic tools. Virol Sin. 2020; 35(3):266–271. PMID: 32125642.27. Short KR, Kasper J, van der Aa S, Andeweg AC, Zaaraoui-Boutahar F, Goeijenbier M, et al. Influenza virus damages the alveolar barrier by disrupting epithelial cell tight junctions. Eur Respir J. 2016; 47(3):954–966. PMID: 26743480.28. Salihu HM, Dongarwar D, Aliyu MH, Azuine RE. Global ranking of COVID-19-related mortality by country using a novel pandemic efficiency index (PEI). Int J MCH AIDS. 2020; 9(2):182–185. PMID: 32431961.29. Shim E. Projecting the impact of SARS-CoV-2 variants and the vaccination program on the fourth wave of the COVID-19 pandemic in South Korea. Int J Environ Res Public Health. 2021; 18(14):7578. PMID: 34300029.30. Bian L, Gao Q, Gao F, Wang Q, He Q, Wu X, et al. Impact of the Delta variant on vaccine efficacy and response strategies. Expert Rev Vaccines. 2021; 20(10):1201–1209. PMID: 34488546.31. Ryu BH, Hong SI, Lim SJ, Cho Y, Hwang C, Kang H, et al. Clinical features of adult COVID-19 patients without risk factors before and after the nationwide SARS-CoV-2 B.1.617.2 (Delta)-variant outbreak in Korea: experience from Gyeongsangnam-do. J Korean Med Sci. 2021; 36(49):e341. PMID: 34931500.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coronavirus Disease 2019-Associated Pulmonary Aspergillosis
- High-Dose Corticosteroid Use in Severe to Critically Ill Patients With COVID-19: A Nationwide PopulationBased Matched Cohort Study
- How We Have Treated Severe to Critically Ill Patients With Coronavirus Disease 2019 in Korea
- Treatment of Critically Ill Patients with Coronavirus Disease 2019
- Experience of Treating Critically Ill COVID-19 Patients in Daegu, South Korea