J Korean Neurosurg Soc.
2022 May;65(3):457-468. 10.3340/jkns.2021.0187.
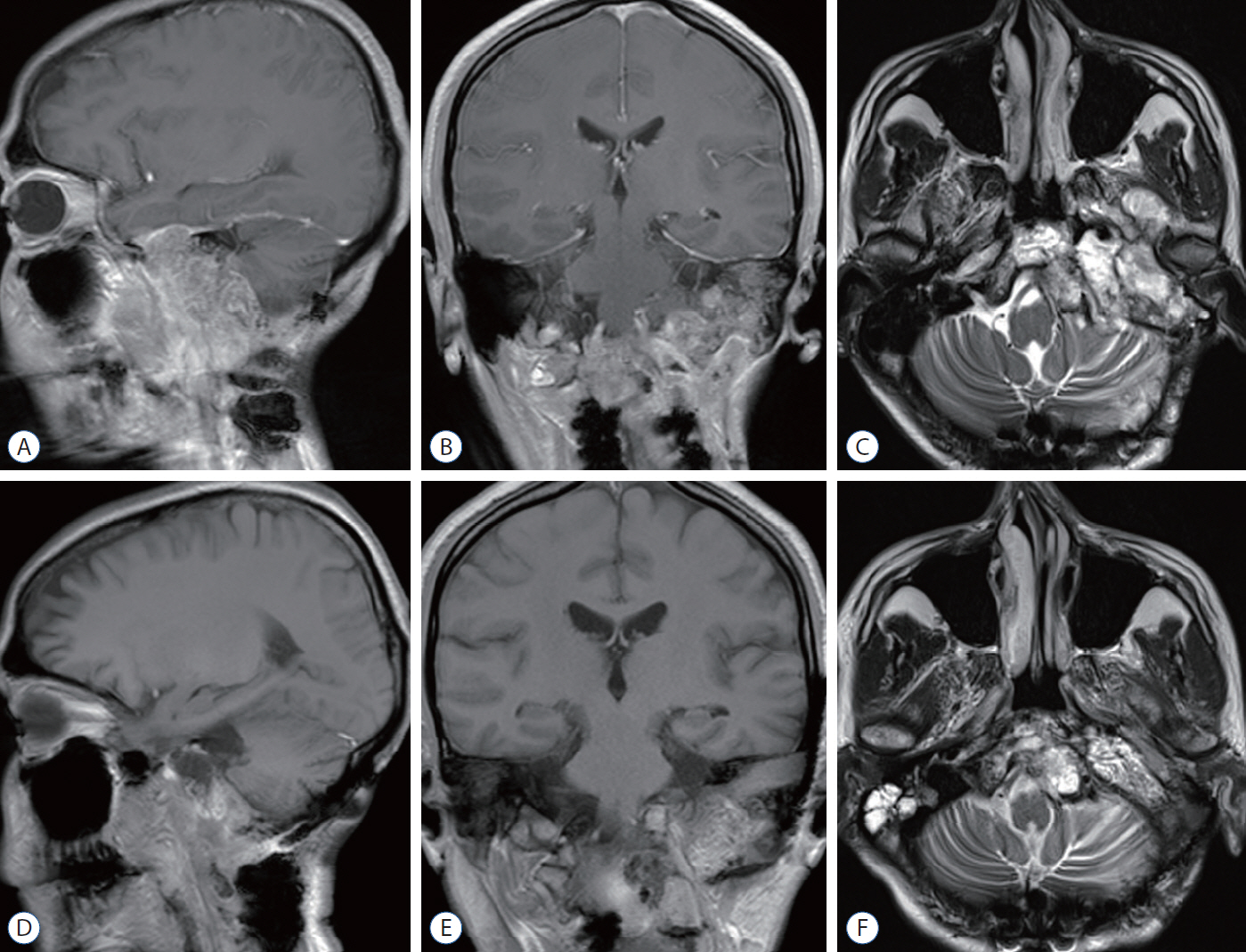
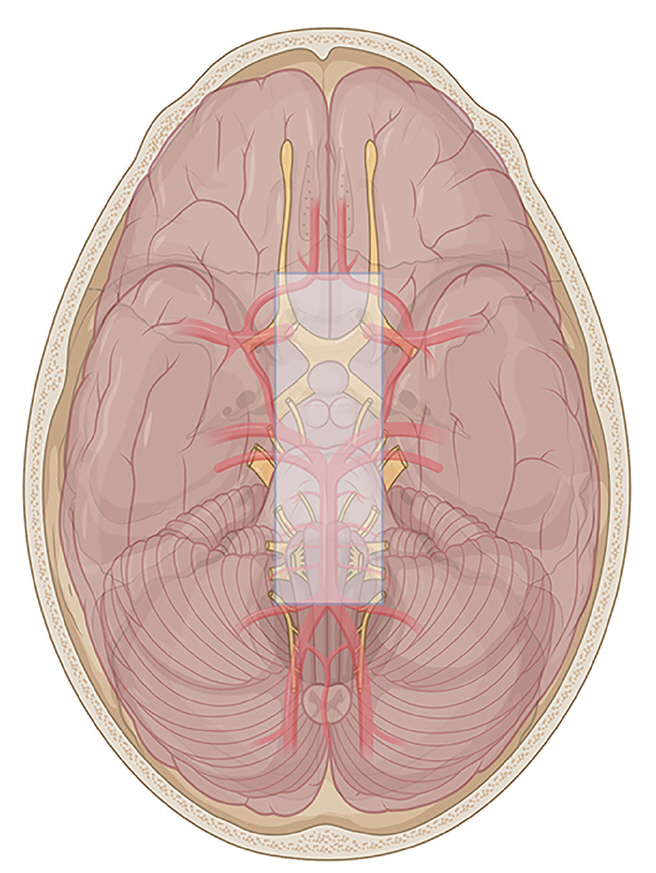
Surgical Strategy for Skull Base Chordomas : Transnasal Midline Approach or Transcranial Lateral Approach
- Affiliations
-
- 1School of Medicine, Nankai University, Tianjin, China
- 2Clinical College of Neurology, Neurosurgery and Neurorehabilitation, Tianjin Medical University, Tianjin, China
- 3Department of Neurosurgery, Tianjin Huanhu Hospital, Tianjin, China
- KMID: 2529591
- DOI: http://doi.org/10.3340/jkns.2021.0187
Abstract
Objective
: The clinical management paradigm of skull base chordomas is still challenging. Surgical resection plays an important role of affecting the prognosis. Endonasal endoscopic approach (EEA) has gradually become the preferred surgical approach in most cases, but traditional transcranial surgery cannot be completely replaced. This study presents a comparison of the results of the two surgical strategies and a summary of the treatment algorithms for skull base chordomas.
Methods
: We retrospectively analyzed the surgical outcomes and follow-up data of 48 patients with skull base chordomas diagnosed pathologically who received transnasal midline approaches (TMA) and transcranial lateral approaches (TLA) from 2010 to 2020.
Results
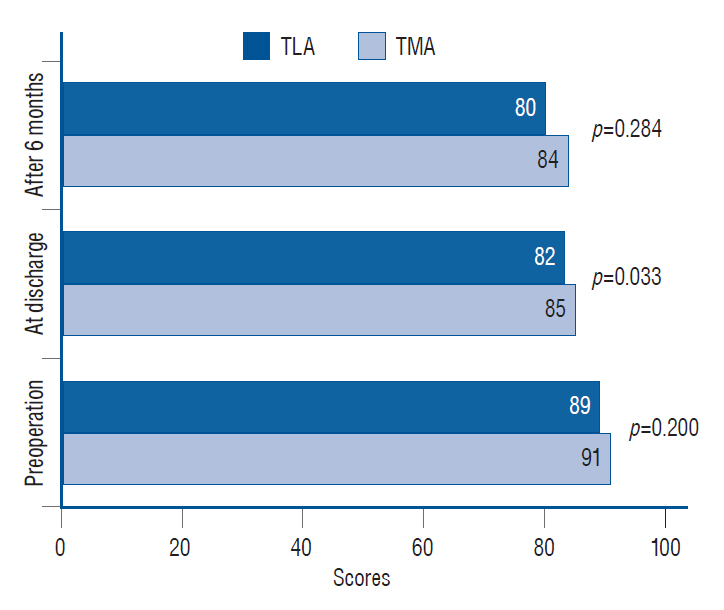
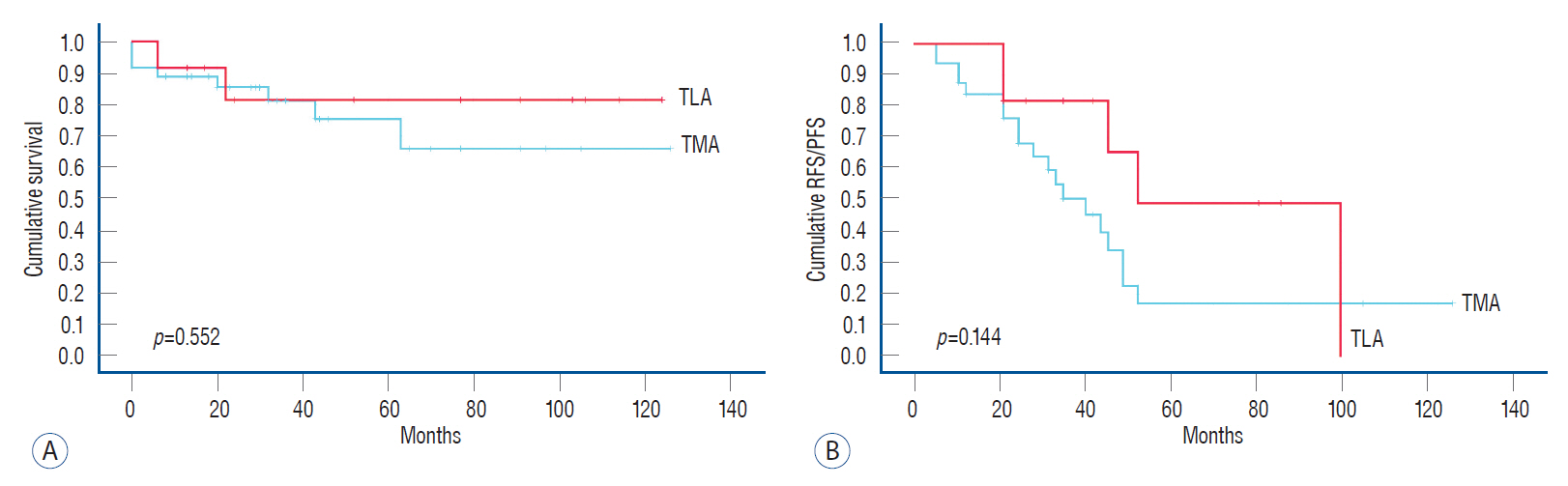
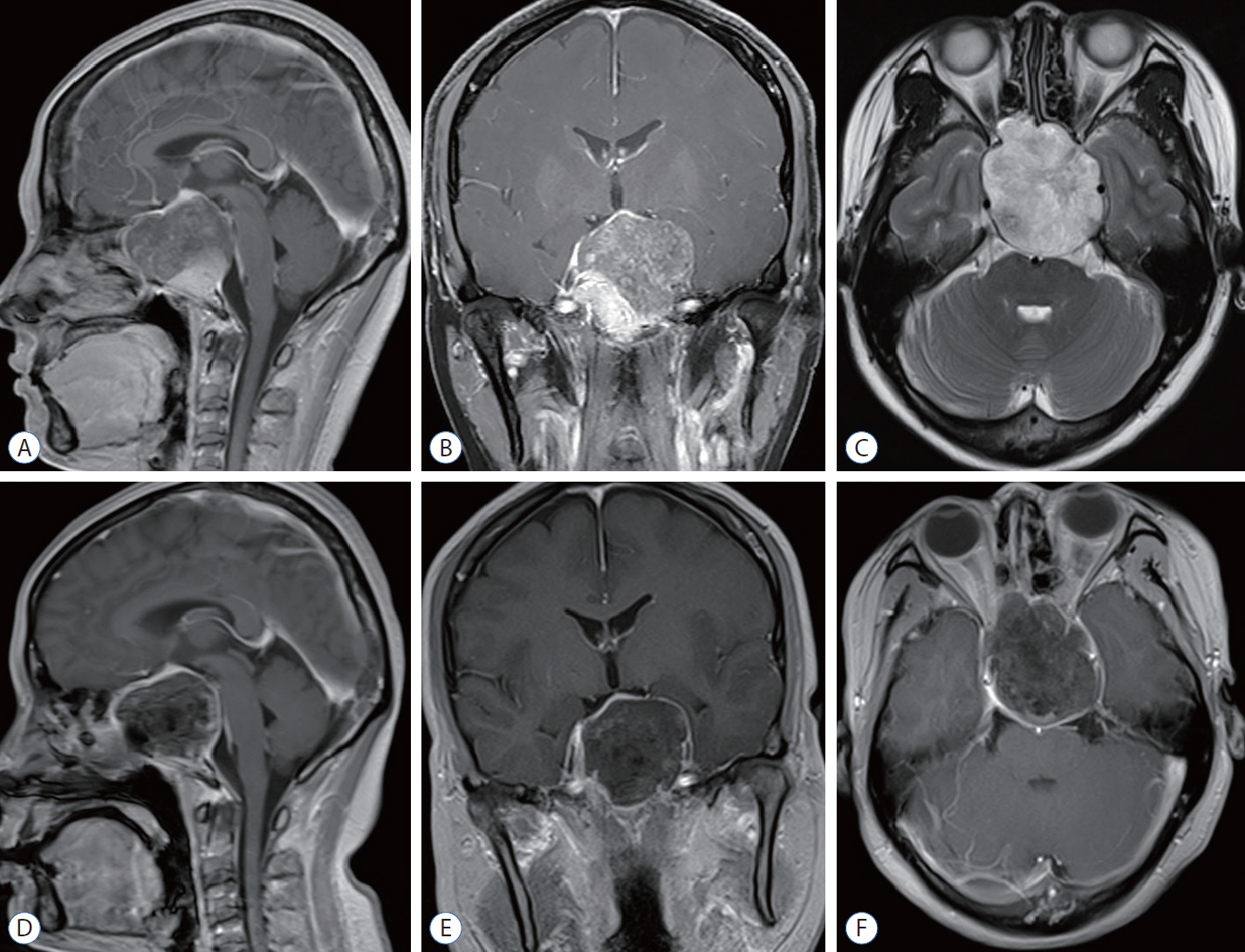
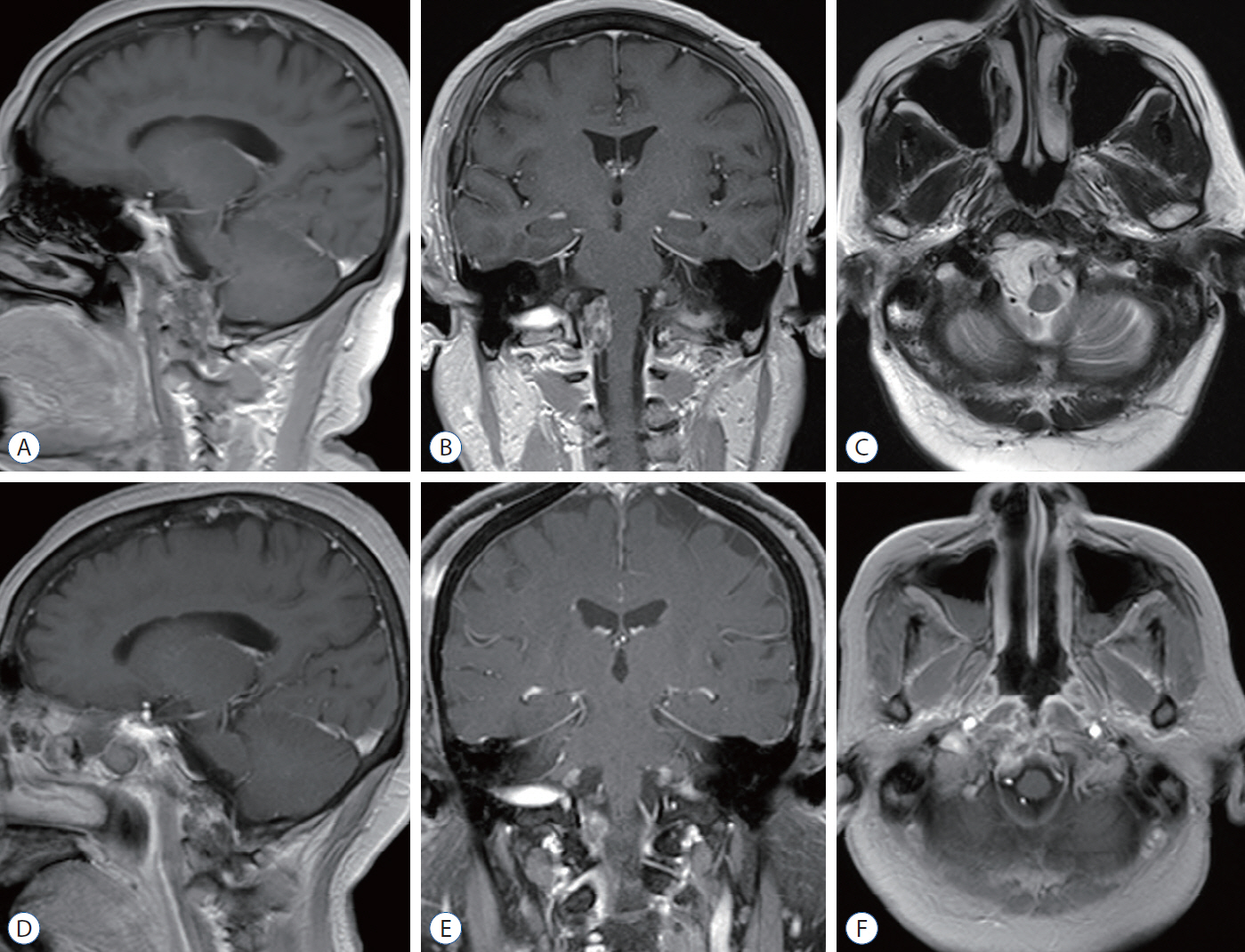
: Among the 48 patients, 36 cases were adopted TMA and 12 cases were performed with TLA. In terms of gross total resection (GTR) rate, 27.8% in TMA and 16.7% in TLA and with EEA alone it was increased to 38.9%, while 29.7% in primary surgery. In TMA, the cerebrospinal fluid (CSF) leak remains the most common complication (13 cases, 36.1%), other main complications included death, cranial nerve palsy, hypopituitarism, all the comparisons were no statistical significance. The Karnofsky Performance Scale scores in TMA were all better than those in TLA at different time, and the overall survival (OS) and recurrence free survival/progression free survival was just the reverse.
Conclusion
: The EEA for skull base chordomas resection has improved the GTR rate, but transcranial approach is still an alternative approach. It is necessary to select an appropriate surgical approach based on the location and the pattern of tumor growth in order to obtain the best surgical outcomes.
Keyword
Figure
Reference
-
References
1. al-Mefty O, Borba LA. Skull base chordomas: a management challenge. J Neurosurg. 86:182–189. 1997.
Article2. Chibbaro S, Cornelius JF, Froelich S, Tigan L, Kehrli P, Debry C, et al. Endoscopic endonasal approach in the management of skull base chordomas--clinical experience on a large series, technique, outcome, and pitfalls. Neurosurg Rev. 37:217–224. discussion 224-225. 2014.
Article3. Choi D, Melcher R, Harms J, Crockard A. Outcome of 132 operations in 97 patients with chordomas of the craniocervical junction and upper cervical spine. Neurosurgery. 66:59–65. discussion 65. 2010.
Article4. Colli B, Al-Mefty O. Chordomas of the craniocervical junction: follow-up review and prognostic factors. J Neurosurg. 95:933–943. 2001.
Article5. Colli BO, Al-Mefty O. Chordomas of the skull base: follow-up review and prognostic factors. Neurosurg Focus. 10:E1. 2001.
Article6. Couldwell WT, Weiss MH, Rabb C, Liu JK, Apfelbaum RI, Fukushima T. Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: surgical experience in 105 cases. Neurosurgery. 55:539–547. discussion 547-550. 2004.
Article7. Delgado TE, Garrido E, Harwick RD. Labiomandibular, transoral approach to chordomas in the clivus and upper cervical spine. Neurosurgery. 8:675–679. 1981.
Article8. DeMonte F, Diaz E Jr, Callender D, Suk I. Transmandibular, circumglossal, retropharyngeal approach for chordomas of the clivus and upper cervical spine. Technical note. Neurosurg Focus. 10:E10. 2001.9. Fatemi N, Dusick JR, Gorgulho AA, Mattozo CA, Moftakhar P, De Salles AA, et al. Endonasal microscopic removal of clival chordomas. Surg Neurol. 69:331–338. 2008.
Article10. Fraser JF, Nyquist GG, Moore N, Anand VK, Schwartz TH. Endoscopic endonasal transclival resection of chordomas: operative technique, clinical outcome, and review of the literature. J Neurosurg. 112:1061–1069. 2010.
Article11. Gay E, Sekhar LN, Rubinstein E, Wright DC, Sen C, Janecka IP, et al. Chordomas and chondrosarcomas of the cranial base: results and follow-up of 60 patients. Neurosurgery. 36:887–896. discussion 896-897. 1995.12. Gui S, Zong X, Wang X, Li C, Zhao P, Cao L, et al. Classification and surgical approaches for transnasal endoscopic skull base chordoma resection: a 6-year experience with 161 cases. Neurosurg Rev. 39:321–332. discussion 332-333. 2016.
Article13. Ito E, Saito K, Okada T, Nagatani T, Nagasaka T. Long-term control of clival chordoma with initial aggressive surgical resection and gamma knife radiosurgery for recurrence. Acta Neurochir (Wien). 152:57–67. discussion 67. 2010.
Article14. Koutourousiou M, Gardner PA, Tormenti MJ, Henry SL, Stefko ST, Kassam AB, et al. Endoscopic endonasal approach for resection of cranial base chordomas: outcomes and learning curve. Neurosurgery. 71:614–624. discussion 624-625. 2012.15. Maira G, Pallini R, Anile C, Fernandez E, Salvinelli F, La Rocca LM, et al. Surgical treatment of clival chordomas: the transsphenoidal approach revisited. J Neurosurg. 85:784–792. 1996.
Article16. Mangussi-Gomes J, Beer-Furlan A, Balsalobre L, Vellutini EA, Stamm AC. Endoscopic endonasal management of skull base chordomas: surgical technique, nuances, and pitfalls. Otolaryngol Clin North Am. 49:167–182. 2016.17. Margalit NS, Lesser JB, Singer M, Sen C. Lateral approach to anterolateral tumors at the foramen magnum: factors determining surgical procedure. Neurosurgery. 56(2 Suppl):324–336. discussion 324-336. 2005.
Article18. Saito K, Toda M, Tomita T, Ogawa K, Yoshida K. Surgical results of an endoscopic endonasal approach for clival chordomas. Acta Neurochir (Wien). 154:879–886. 2012.
Article19. Salas E, Sekhar LN, Ziyal IM, Caputy AJ, Wright DC. Variations of the extreme-lateral craniocervical approach: anatomical study and clinical analysis of 69 patients. J Neurosurg. 90(2 Suppl):206–219. 1999.
Article20. Sekhar LN, Nanda A, Sen CN, Snyderman CN, Janecka IP. The extended frontal approach to tumors of the anterior, middle, and posterior skull base. J Neurosurg. 76:198–206. 1992.
Article21. Sekhar LN, Schramm VL Jr, Jones NF. Subtemporal-preauricular infratemporal fossa approach to large lateral and posterior cranial base neoplasms. J Neurosurg. 67:488–499. 1987.
Article22. Sen C, Triana A. Cranial chordomas: results of radical excision. Neurosurg Focus. 10:E3. 2001.
Article23. Sen C, Triana AI, Berglind N, Godbold J, Shrivastava RK. Clival chordomas: clinical management, results, and complications in 71 patients. J Neurosurg. 113:1059–1071. 2010.
Article24. Sen CN, Sekhar LN. An extreme lateral approach to intradural lesions of the cervical spine and foramen magnum. Neurosurgery. 27:197–204. 1990.
Article25. Sen CN, Sekhar LN. The subtemporal and preauricular infratemporal approach to intradural structures ventral to the brain stem. J Neurosurg. 73:345–354. 1990.
Article26. Stacchiotti S, Sommer J; Chordoma Global Consensus Group. Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol. 16:e71–e83. 2015.
Article27. Stippler M, Gardner PA, Snyderman CH, Carrau RL, Prevedello DM, Kassam AB. Endoscopic endonasal approach for clival chordomas. Neurosurgery. 64:268–277. discussion 277-278. 2009.
Article28. Tzortzidis F, Elahi F, Wright D, Natarajan SK, Sekhar LN. Patient outcome at long-term follow-up after aggressive microsurgical resection of cranial base chordomas. Neurosurgery. 59:230–237. discussion 230-237. 2006.
Article29. Walcott BP, Nahed BV, Mohyeldin A, Coumans JV, Kahle KT, Ferreira MJ. Chordoma: current concepts, management, and future directions. Lancet Oncol. 13:e69–e76. 2012.
Article30. Zoli M, Milanese L, Bonfatti R, Faustini-Fustini M, Marucci G, Tallini G, et al. Clival chordomas: considerations after 16 years of endoscopic endonasal surgery. J Neurosurg. 128:329–338. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iatrogenic Skull Base Defect Accompanied by Brain Injury After Endoscopic Sinus Surgery: A Report of Two Cases
- Anterior Approaches to Midline Skull Base Tumors
- Extensive Transbasal Approach to Skull Base Tumor
- The Role of Transfacial Approach in Skull Base Surgery
- Transoral Approach to Lower Third of a Clival Meningioma