Ann Surg Treat Res.
2022 May;102(5):248-256. 10.4174/astr.2022.102.5.248.
Predicting prognosis and evaluating the benefits of adjuvant chemotherapy depending on the tumor location in intrahepatic cholangiocarcinoma: focusing on the involvement of below 2nd bile duct confluence
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Surgery, Gyeongsang National University Changwon Hospital, Changwon, Korea
- KMID: 2529499
- DOI: http://doi.org/10.4174/astr.2022.102.5.248
Abstract
- Purpose
Intrahepatic cholangiocarcinoma (ICC) has various characteristics according to anatomical, histologic classifications, and its prognoses are different. This study aimed to compare oncologic outcomes according to tumor location (second bile duct confluence) and evaluate the effect of adjuvant chemotherapy.
Methods
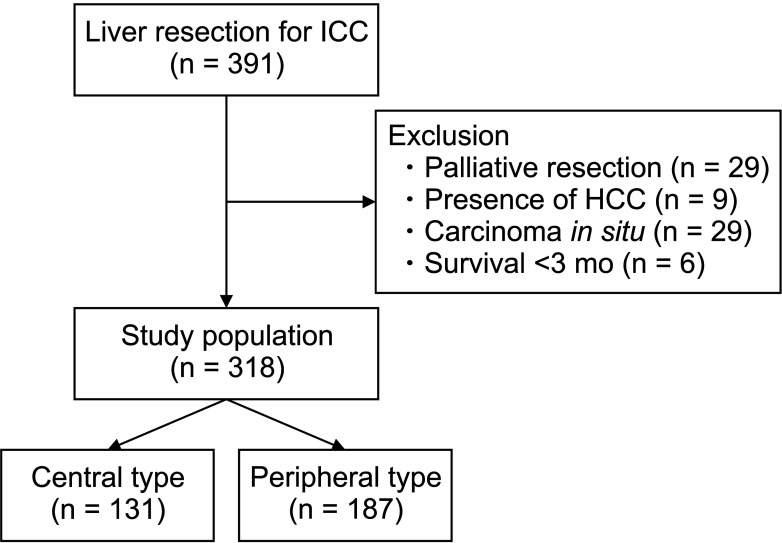
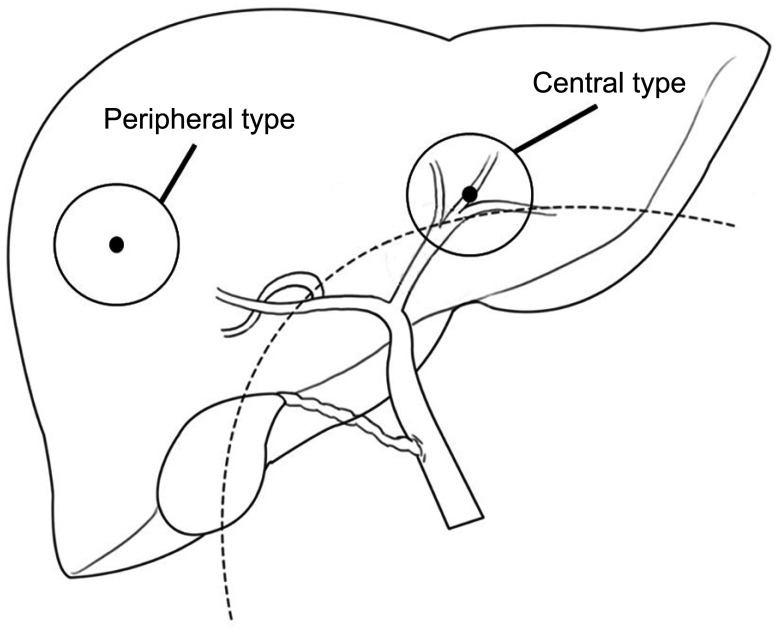
Clinical data of 318 patients who underwent curative resection for ICC was reviewed. Central type ICC (C-ICC) and peripheral type ICC (P-ICC) were defined when the tumor invades the intrahepatic secondary biliary confluence and when located more peripherally, respectively.
Results
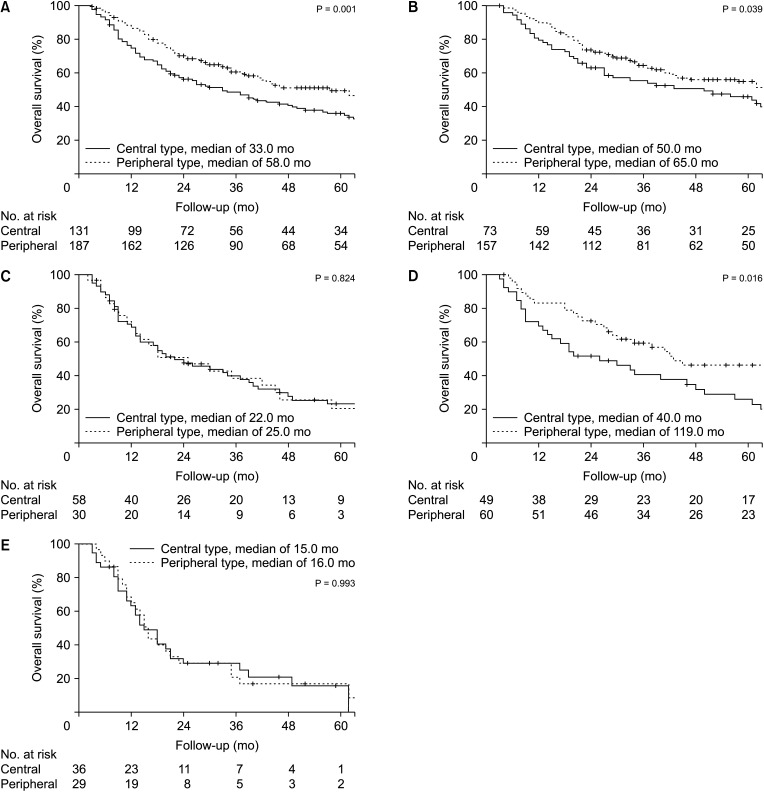
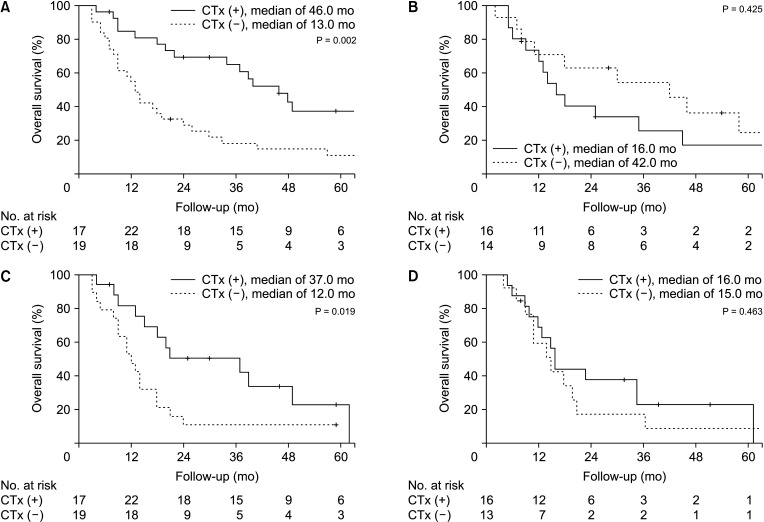
A larger tumor size, higher rate of elevated CA 19-9 level, vascular invasion, R1 resection, advanced T stage, and lymph node metastasis were found in C-ICC. C-ICC had poorer overall survival (median, 33 months vs. 58 months; P = 0.001), and the difference was more prominent in the early stage. C-ICC had a higher recurrence rate (68.7% vs. 55.1%, P = 0.014); otherwise, there was no difference in the recurrence patterns. There were no survival benefits of adjuvant chemotherapy in the entire cohort, but there were benefits in advanced stages (T3–4, N1 stage), especially in C-ICC.
Conclusion
C-ICC has more aggressive tumor characteristics and poor survival compared to P-ICC. Adjuvant chemotherapy seems to have survival benefits in the advanced stages, especially in the central type.
Figure
Reference
-
1. De Oliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007; 245:755–762. PMID: 17457168.2. Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet. 2014; 383:2168–2179. PMID: 24581682.3. Saha SK, Zhu AX, Fuchs CS, Brooks GA. Forty-year trends in cholangiocarcinoma incidence in the U.S.: intrahepatic disease on the rise. Oncologist. 2016; 21:594–599. PMID: 27000463.4. Aljiffry M, Abdulelah A, Walsh M, Peltekian K, Alwayn I, Molinari M. Evidence-based approach to cholangiocarcinoma: a systematic review of the current literature. J Am Coll Surg. 2009; 208:134–147. PMID: 19228515.5. Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014; 60:1268–1289. PMID: 24681130.6. Hu LS, Zhang XF, Weiss M, Popescu I, Marques HP, Aldrighetti L, et al. Recurrence patterns and timing courses following curative-intent resection for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2019; 26:2549–2557. PMID: 31020501.7. Kojima T, Umeda Y, Fuji T, Niguma T, Sato D, Endo Y, et al. Efficacy of surgical management for recurrent intrahepatic cholangiocarcinoma: a multi-institutional study by the Okayama Study Group of HBP surgery. PLoS One. 2020; 15:e0238392. PMID: 32881910.8. Yamasaki S. Intrahepatic cholangiocarcinoma: macroscopic type and stage classification. J Hepatobiliary Pancreat Surg. 2003; 10:288–291. PMID: 14598147.9. Nakanuma Y, Sato Y, Harada K, Sasaki M, Xu J, Ikeda H. Pathological classification of intrahepatic cholangiocarcinoma based on a new concept. World J Hepatol. 2010; 2:419–427. PMID: 21191517.10. Ke Q, Lin N, Deng M, Wang L, Zeng Y, Liu J. The effect of adjuvant therapy for patients with intrahepatic cholangiocarcinoma after surgical resection: a systematic review and meta-analysis. PLoS One. 2020; 15:e0229292. PMID: 32084210.11. Zhu AX, Knox JJ. Adjuvant therapy for intrahepatic cholangiocarcinoma: the debate continues. Oncologist. 2012; 17:1504–1507. PMID: 23220842.12. Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC Cancer Staging Manual. 8th ed. New York: Springer;2017.13. Murakami Y, Uemura K, Sudo T, Hashimoto Y, Nakashima A, Sueda T. Intrahepatic cholangiocarcinoma: clinicopathological differences between peripheral type and hilar type. J Gastrointest Surg. 2012; 16:540–548. PMID: 22012305.14. Aishima S, Kuroda Y, Nishihara Y, Iguchi T, Taguchi K, Taketomi A, et al. Proposal of progression model for intrahepatic cholangiocarcinoma: clinicopathologic differences between hilar type and peripheral type. Am J Surg Pathol. 2007; 31:1059–1067. PMID: 17592273.15. Lee W, Jeong CY, Jang JY, Roh YH, Kim KW, Kang SH, et al. Clinical implication of tumor site in terms of node metastasis for intrahepatic cholangiocarcinoma. Eur J Surg Oncol. 2020; 46:832–838. PMID: 31806519.16. Lu J, Li B, Li FY, Ye H, Xiong XZ, Cheng NS. Long-term outcome and prognostic factors of intrahepatic cholangiocarcinoma involving the hepatic hilus versus hilar cholangiocarcinoma after curative-intent resection: should they be recognized as perihilar cholangiocarcinoma or differentiated? Eur J Surg Oncol. 2019; 45:2173–2179. PMID: 31208772.17. Zhang XF, Bagante F, Chen Q, Beal EW, Lv Y, Weiss M, et al. Perioperative and long-term outcome of intrahepatic cholangiocarcinoma involving the hepatic hilus after curative-intent resection: comparison with peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma. Surgery. 2018; 163:1114–1120. PMID: 29398035.18. Kang MJ, Lim J, Han SS, Park HM, Kim SW, Won YJ, et al. Impact of changes in the topographic classification of Klatskin tumor on incidence of intra- and extrahepatic bile duct cancer: a population-based national cancer registry study. J Hepatobiliary Pancreat Sci. 2021; 28:740–750. PMID: 33615747.19. Khan SA, Tavolari S, Brandi G. Cholangiocarcinoma: epidemiology and risk factors. Liver Int. 2019; 39 Suppl 1:19–31. PMID: 30851228.20. Zhang XF, Xue F, Dong DH, Weiss M, Popescu I, Marques HP, et al. Number and station of lymph node metastasis after curative-intent resection of intrahepatic cholangiocarcinoma impact prognosis. Ann Surg. 2021; 274:e1187–e1195. PMID: 31972643.21. Bagante F, Gani F, Spolverato G, Xu L, Alexandrescu S, Marques HP, et al. Intrahepatic cholangiocarcinoma: prognosis of patients who did not undergo lymphadenectomy. J Am Coll Surg. 2015; 221:1031–1040. PMID: 26474514.22. Jutric Z, Johnston WC, Hoen HM, Newell PH, Cassera MA, Hammill CW, et al. Impact of lymph node status in patients with intrahepatic cholangiocarcinoma treated by major hepatectomy: a review of the National Cancer Database. HPB (Oxford). 2016; 18:79–87. PMID: 26776855.23. Li DY, Zhang HB, Yang N, Quan Y, Yang GS. Routine lymph node dissection may be not suitable for all intrahepatic cholangiocarcinoma patients: results of a monocentric series. World J Gastroenterol. 2013; 19:9084–9091. PMID: 24379635.24. Tsilimigras DI, Sahara K, Paredes AZ, Moro A, Mehta R, Moris D, et al. Predicting lymph node metastasis in intrahepatic cholangiocarcinoma. J Gastrointest Surg. 2021; 25:1156–1163. PMID: 32757124.25. Hu J, Chen FY, Zhou KQ, Zhou C, Cao Y, Sun HC, et al. Intrahepatic cholangiocarcinoma patients without indications of lymph node metastasis not benefit from lymph node dissection. Oncotarget. 2017; 8:113817–113827. PMID: 29371948.26. Zhang XF, Chakedis J, Bagante F, Beal EW, Lv Y, Weiss M, et al. Implications of intrahepatic cholangiocarcinoma etiology on recurrence and prognosis after curative-intent resection: a multi-institutional study. World J Surg. 2018; 42:849–857. PMID: 28879598.27. Hyder O, Hatzaras I, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H, et al. Recurrence after operative management of intrahepatic cholangiocarcinoma. Surgery. 2013; 153:811–818. PMID: 23499016.28. Ma KW, Cheung TT, Leung B, She BW, Chok KS, Chan AC, et al. Adjuvant chemotherapy improves oncological outcomes of resectable intrahepatic cholangiocarcinoma: a meta-analysis. Medicine (Baltimore). 2019; 98:e14013. PMID: 30702559.29. Primrose JN, Fox RP, Palmer DH, Malik HZ, Prasad R, Mirza D, et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019; 20:663–673. PMID: 30922733.30. Edeline J, Benabdelghani M, Bertaut A, Watelet J, Hammel P, Joly JP, et al. Gemcitabine and oxaliplatin chemotherapy or surveillance in resected biliary tract cancer (PRODIGE 12-ACCORD 18-UNICANCER GI): a randomized phase III study. J Clin Oncol. 2019; 37:658–667. PMID: 30707660.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Histopathology of a benign bile duct lesion in the liver: Morphologic mimicker or precursor of intrahepatic cholangiocarcinoma
- Obstructive Jaundice by Tumor Emboli from Intrahepatic Cholangiocarcinoma
- Intrahepatic cholangiocarcinoma presenting as liver Abscess: Report of Two Cases
- Radiological Staging of Hilar Cholangiocarcinoma
- Review: Analysis of Survival Rate and Prognostic Factors of Intrahepatic Cholangiocarcinoma: 318 Cases in Single Institute