Ewha Med J.
2022 Apr;45(2):29-34. 10.12771/emj.2022.45.2.29.
Prevention and Management of Small-for-Size Syndrome of Liver Transplantation
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2529433
- DOI: http://doi.org/10.12771/emj.2022.45.2.29
Abstract
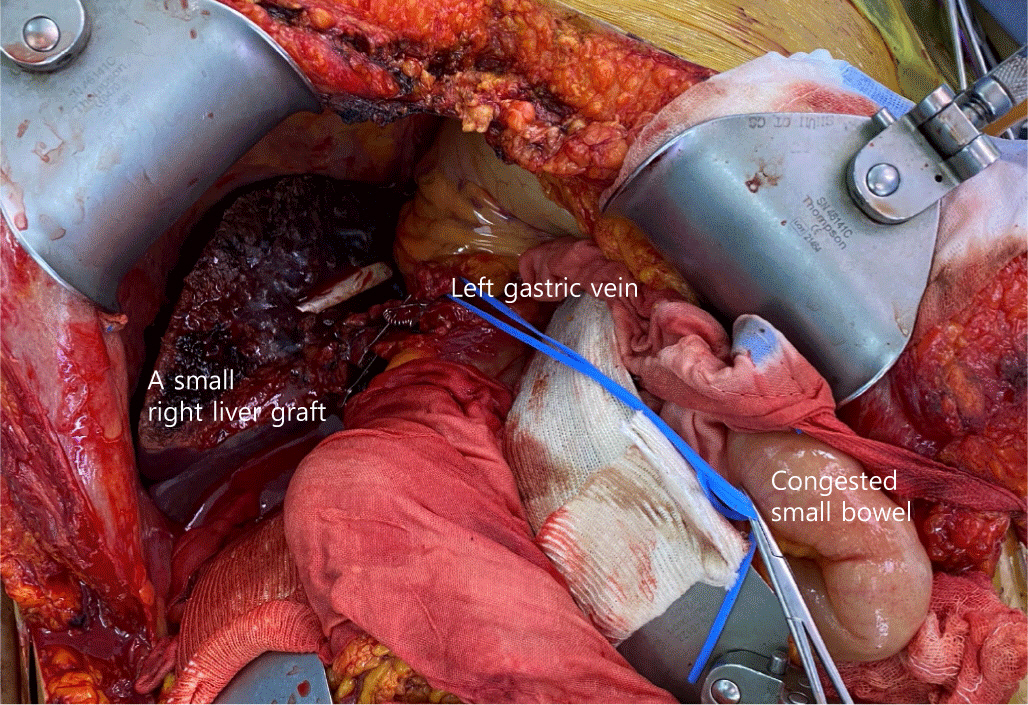
- Small-for-size syndrome (SFSS) is a critical complication of partial liver transplantation, particularly in adult-to-adult living donor liver transplantation (ALDLT) using a small graft. Minimally required liver graft size for a successful ALDLT is classically 40% of a standard recipient’s liver volume or 0.8% of recipient body weight. Recent progress in perioperative care and technical improvement push the lower limit of safe graft size to 25% of the recipient’s standard liver volume or 0.6% of the graft versus recipient weight ratio although this is an ongoing debate. The clinical manifestations of SFSS include various symptoms and signs related to graft dysfunction and portal hypertension in patients with small grafts. The risk factors for SFSS include poor preoperative patient condition, including portal pressure, surgical techniques to reduce portal pressure, and graft quality and size. Hence, various approaches have been explored to modulate inflow and pressure to a small graft and to decrease the outflow block to alleviate this SFSS as well as the selection of a patient and graft. Additionally, recent research and efforts to prevent and treat SFSS are reviewed.
Keyword
Figure
Reference
-
References
1. Chen CL, Fan ST, Lee SG, Makuuchi M, Tanaka K. Living-donor liver transplantation: 12 years of experience in Asia. Transplantation. 2003; 75:S6–S11. DOI: 10.1097/01.TP.0000046533.93621.C7. PMID: 12589130.2. Hashikura Y, Makuuchi M, Kawasaki S, Matsunami H, Ikegami T, Nakazawa Y, et al. Successful living-related partial liver transplantation to an adult patient. Lancet. 1994; 343:1233–1234. DOI: 10.1016/S0140-6736(94)92450-3.3. Tanaka K, Uemoto S, Tokunaga Y, Fujita S, Sano K, Nishizawa T, et al. Surgical techniques and innovations in living related liver transplantation. Ann Surg. 1993; 217:82–91. DOI: 10.1097/00000658-199301000-00014. PMID: 8424706. PMCID: PMC1242738.4. Hong SK, Choe S, Yi NJ, Shin A, Choe EK, Yoon KC, et al. Long-term survival of 10,116 Korean live liver donors. Ann Surg. 2021; 274:375–382. DOI: 10.1097/SLA.0000000000003752. PMID: 31850982.5. Kiuchi T, Kasahara M, Uryuhara K, Inomata Y, Uemoto S, Asonuma K, et al. Impact of graft size mismatching on graft prognosis in liver transplantation from living donors. Transplantation. 1999; 67:321–327. DOI: 10.1097/00007890-199901270-00024. PMID: 10075602.6. Kiuchi T, Tanaka K, Ito T, Oike F, Ogura Y, Fujimoto Y, et al. Small-for-size graft in living donor liver transplantation: how far should we go? Liver Transpl. 2003; 9:S29–S35. DOI: 10.1053/jlts.2003.50198. PMID: 12942476.7. Lo CM, Fan ST, Liu CL, Chan JK, Lam BK, Lau GK, et al. Minimum graft size for successful living donor liver transplantation. Transplantation. 1999; 68:1112–1116. DOI: 10.1097/00007890-199910270-00009. PMID: 10551638.8. Masuda Y, Yoshizawa K, Ohno Y, Mita A, Shimizu A, Soejima Y. Small-for-size syndrome in liver transplantation: definition, pathophysiology and management. Hepatobiliary Pancreat Dis Int. 2020; 19:334–341. DOI: 10.1016/j.hbpd.2020.06.015. PMID: 32646775.9. Ben-Haim M, Emre S, Fishbein TM, Sheiner PA, Bodian CA, Kim-Schluger L, et al. Critical graft size in adult-to-adult living donor liver transplantation: impact of the recipient’s disease. Liver Transpl. 2001; 7:948–953. DOI: 10.1053/jlts.2001.29033. PMID: 11699030.10. Dahm F, Georgiev P, Clavien PA. Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant. 2005; 5:2605–2610. DOI: 10.1111/j.1600-6143.2005.01081.x. PMID: 16212618.11. Yi NJ, Suh KS, Cho YB, Lee HW, Cho EH, Cho JY, et al. The right small-for-size graft results in better outcomes than the left small-for-size graft in adult-to-adult living donor liver transplantation. World J Surg. 2008; 32:1722–1730. DOI: 10.1007/s00268-008-9641-6. PMID: 18553047.12. Emond JC, Renz JF, Ferrell LD, Rosenthal P, Lim RC, Roberts JP, et al. Functional analysis of grafts from living donors: implications for the treatment of older recipients. Ann Surg. 1996; 224:544–554. DOI: 10.1097/00000658-199610000-00012. PMID: 8857858. PMCID: PMC1235420.13. Demetris AJ, Kelly DM, Eghtesad B, Fontes P, Wallis Marsh J, Tom K, et al. Pathophysiologic observations and histopathologic recognition of the portal hyperperfusion or small-for-size syndrome. Am J Surg Pathol. 2006; 30:986–993. DOI: 10.1097/00000478-200608000-00009. PMID: 16861970.14. Yi NJ, Suh KS, Lee HW, Shin WY, Kim J, Kim W, et al. Improved outcome of adult recipients with a high model for end-stage liver disease score and a small-for-size graft. Liver Transpl. 2009; 15:496–503. DOI: 10.1002/lt.21606. PMID: 19399732.15. Ma KW, Wong KHC, Chan ACY, Cheung TT, Dai WC, Fung JYY, et al. Impact of small-for-size liver grafts on medium-term and long-term graft survival in living donor liver transplantation: a meta-analysis. World J Gastroenterol. 2019; 25:5559–5568. DOI: 10.3748/wjg.v25.i36.5559. PMID: 31576100. PMCID: PMC6767984.16. Ikegami T, Balci D, Jung DH, Kim JM, Quintini C. Living donor liver transplantation in small-for-size setting. Int J Surg. 2020; 82:134–137. DOI: 10.1016/j.ijsu.2020.07.003. PMID: 32738547.17. Chan SC, Fan ST, Lo CM, Liu CL. Effect of side and size of graft on surgical outcomes of adult-to-adult live donor liver transplantation. Liver Transpl. 2007; 13:91–98. DOI: 10.1002/lt.20987. PMID: 17192891.18. Ito T, Kiuchi T, Yamamoto H, Oike F, Ogura Y, Fujimoto Y, et al. Changes in portal venous pressure in the early phase after living donor liver transplantation: pathogenesis and clinical implications. Transplantation. 2003; 75:1313–1317. DOI: 10.1097/01.TP.0000063707.90525.10. PMID: 12717222.19. Troisi R, Cammu G, Militerno G, De Baerdemaeker L, Decruyenaere J, Hoste E, et al. Modulation of portal graft inflow: a necessity in adult living-donor liver transplantation? Ann Surg. 2003; 237:429–436. DOI: 10.1097/01.SLA.0000055277.78876.B7. PMID: 12616129. PMCID: PMC1514313.20. Botha JF, Langnas AN, Campos BD, Grant WJ, Freise CE, Ascher NL, et al. Left lobe adult-to-adult living donor liver transplantation: small grafts and hemiportocaval shunts in the prevention of small-for-size syndrome. Liver Transpl. 2010; 16:649–657. DOI: 10.1002/lt.22043. PMID: 20440774.21. Moon DB, Lee SG, Hwang S, Ahn CS, Kim KH, Ha TY, et al. Splenic devascularization can replace splenectomy during adult living donor liver transplantation: a historical cohort study. Transpl Int. 2019; 32:535–545. DOI: 10.1111/tri.13405. PMID: 30714245.22. Ito K, Akamatsu N, Ichida A, Ito D, Kaneko J, Arita J, et al. Splenectomy is not indicated in living donor liver transplantation. Liver Transpl. 2016; 22:1526–1535. DOI: 10.1002/lt.24489. PMID: 27253521.23. Yi NJ, Suh KS, Lee HW, Cho EH, Shin WY, Cho JY, et al. An artificial vascular graft is a useful interpositional material for drainage of the right anterior section in living donor liver transplantation. Liver Transpl. 2007; 13:1159–1167. DOI: 10.1002/lt.21213. PMID: 17663413.24. Lee SG. A complete treatment of adult living donor liver transplantation: a review of surgical technique and current challenges to expand indication of patients. Am J Transplant. 2015; 15:17–38. DOI: 10.1111/ajt.12907. PMID: 25358749.25. Kasahara M, Kiuchi T, Uryuhara K, Takakura K, Egawa H, Asonuma K, et al. Auxiliary partial orthotopic liver transplantation as a rescue for small-for-size grafts harvested from living donors. Transpl Proc. 1998; 30:132–133. DOI: 10.1016/S0041-1345(97)01210-4.26. Kasahara M, Takada Y, Egawa H, Fujimoto Y, Ogura Y, Ogawa K, et al. Auxiliary partial orthotopic living donor liver transplantation: Kyoto University experience. Am J Transplant. 2005; 5:558–565. DOI: 10.1111/j.1600-6143.2005.00717.x. PMID: 15707411.27. Lee SG, Hwang S, Park KM, Kim KH, Ahn CS, Lee YJ, et al. Seventeen adult-to-adult living donor liver transplantations using dual grafts. Transpl Proc. 2001; 33:3461–3463. DOI: 10.1016/S0041-1345(01)02491-5.28. Soejima Y, Taketomi A, Ikegami T, Yoshizumi T, Uchiyama H, Yamashita Y, et al. Living donor liver transplantation using dual grafts from two donors: a feasible option to overcome small-for-size graft problems? Am J Transplant. 2008; 8:887–892. DOI: 10.1111/j.1600-6143.2008.02153.x. PMID: 18294350.29. Konigsrainer A, Templin S, Capobianco I, Konigsrainer I, Bitzer M, Zender L, et al. Paradigm shift in the management of irresectable colorectal liver metastases: living donor auxiliary partial orthotopic liver transplantation in combination with two-stage hepatectomy (LD-RAPID). Ann Surg. 2019; 270:327–332. DOI: 10.1097/SLA.0000000000002861. PMID: 29916882.30. Lim C, Turco C, Balci D, Savier E, Goumard C, Perdigao F, et al. Auxiliary liver transplantation for cirrhosis: from APOLT to RAPID: a scoping review. Ann Surg. 2022; 275:551–559. DOI: 10.1097/SLA.0000000000005336. PMID: 34913893.31. Ravaioli M, Brandi G, Siniscalchi A, Renzulli M, Bonatti C, Fallani G, et al. Heterotopic segmental liver transplantation on splenic vessels after splenectomy with delayed native hepatectomy alter graft regeneration: a new technique to enhance liver transplantation. Am J Transplant. 2021; 21:870–875. DOI: 10.1111/ajt.16222. PMID: 32715576.32. Cho JY, Suh KS, Kwon CH, Yi NJ, Kim MA, Jang JJ, et al. Auxiliary partial orthotopic living donor liver transplantation in a patient with alcoholic liver cirrhosis to overcome donor steatosis. Transpl Int. 2006; 19:424–429. DOI: 10.1111/j.1432-2277.2006.00295.x. PMID: 16623878.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- "Small-for-size Graft" and "Small-for-size Syndrome" in Living Donor Liver Transplantation
- Anatomical limits in living donor liver transplantation
- Multivisceral Transplantation
- Anesthetic management of living donor liver transplantation for complement factor H deficiency hemolytic uremic syndrome: a case report
- Clinical implication of hepatic volumetry for living donor liver transplantation