Acute Crit Care.
2022 Feb;37(1):94-100. 10.4266/acc.2021.01354.
Diaphragm ultrasound as a better predictor of successful extubation from mechanical ventilation than rapid shallow breathing index
- Affiliations
-
- 1Department of Critical Care Medicine, Imperial Hospital, Chattogram, Bangladesh
- 2Department of Public Health, North South University, Dhaka, Bangladesh
- 3Department of Anaesthesia and Intensive Care Medicine, Chattogram Medical College Hospital, Chattogram, Bangladesh
- KMID: 2527911
- DOI: http://doi.org/10.4266/acc.2021.01354
Abstract
- Background
In 3%–19% of patients, reintubation is needed 48–72 hours following extubation, which increases intensive care unit (ICU) morbidity, mortality, and expenses. Extubation failure is frequently caused by diaphragm dysfunction. Ultrasonography can be used to determine the mobility and thickness of the diaphragm. This study looked at the role of diaphragm excursion (DE) and thickening fraction in predicting successful extubation from mechanical ventilation.
Methods
Thirty-one patients were extubated with the advice of an ICU consultant using the ICU weaning regimen and diaphragm ultrasonography was performed. Ultrasound DE and thickening fraction were measured three times: at the commencement of the t-piece experiment, at 10 minutes, and immediately before extubation. All patients' parameters were monitored for 48 hours after extubation. Rapid shallow breathing index (RSBI) was also measured at the same time.
Results
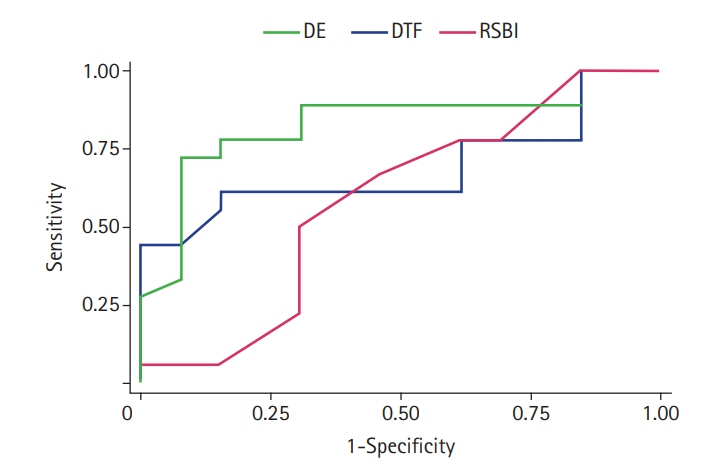
Successful extubation was significantly correlated with DE (P=0.01). Receiver curve analysis for DE to predict successful extubation revealed good properties (area under the curve [AUC], 0.83; P<0.001); sensitivity, 77.8%; specificity, 84.6%, positive predictive value (PPV), 87.5%; negative predictive value (NPV), 73.3% while cut-off value, 11.43 mm. Diaphragm thickening fraction (DTF) also revealed moderate curve properties (AUC, 0.69; P=0.06); sensitivity, 61.1%; specificity, 84.6%; PPV, 87.5%; NPV, 61.1% with cut-off value 22.33% although former one was slightly better. RSBI could not reach good receiver operating characteristic value at cut-off points 100 b/min/L (AUC, 0.58; P=0.47); sensitivity, 66.7%; specificity, 53.8%; PPV, 66.7%; NPV, 53.8%).
Conclusions
To decrease the rate of reintubation, DE and DTF are better indicators of successful extubation. DE outperforms DTF.
Keyword
Figure
Cited by 2 articles
-
The role of diaphragmatic thickness measurement in weaning prediction and its comparison with rapid shallow breathing index: a single-center experience
Lokesh Kumar Lalwani, Manjunath B Govindagoudar, Pawan Kumar Singh, Mukesh Sharma, Dhruva Chaudhry
Acute Crit Care. 2022;37(3):347-354. doi: 10.4266/acc.2022.00108.Diaphragm ultrasound in weaning from mechanical ventilation: a last step to predict successful extubation?
Domenica Di Costanzo, Mariano Mazza, Antonio Esquinas
Acute Crit Care. 2022;37(4):681-682. doi: 10.4266/acc.2022.00227.
Reference
-
1. Kulkarni AP, Agarwal V. Extubation failure in intensive care unit: predictors and management. Indian J Crit Care Med. 2008; 12:1–9.
Article2. Mokhlesi B, Tulaimat A, Gluckman TJ, Wang Y, Evans AT, Corbridge TC. Predicting extubation failure after successful completion of a spontaneous breathing trial. Respir Care. 2007; 52:1710–7.3. Zein H, Baratloo A, Negida A, Safari S. Ventilator weaning and spontaneous breathing trials; an educational review. Emerg (Tehran). 2016; 4:65–71.4. Sigala I, Vassilakopoulos T. Diaphragmatic ultrasound as a monitoring tool in the intensive care unit. Ann Transl Med. 2017; 5:79.
Article5. Jung B, Moury PH, Mahul M, de Jong A, Galia F, Prades A, et al. Diaphragmatic dysfunction in patients with ICU-acquired weakness and its impact on extubation failure. Intensive Care Med. 2016; 42:853–61.
Article6. Liu YY, Li LF. Ventilator-induced diaphragm dysfunction in critical illness. Exp Biol Med (Maywood). 2018; 243:1329–37.7. Petrof BJ, Hussain SN. Ventilator-induced diaphragmatic dysfunction: what have we learned? Curr Opin Crit Care. 2016; 22:67–72.8. Ely EW, Baker AM, Evans GW, Haponik EF. The prognostic significance of passing a daily screen of weaning parameters. Intensive Care Med. 1999; 25:581–7.9. Karthika M, Al Enezi FA, Pillai LV, Arabi YM. Rapid shallow breathing index. Ann Thorac Med. 2016; 11:167–76.
Article10. Nemer SN, Barbas CS. Predictive parameters for weaning from mechanical ventilation. J Bras Pneumol. 2011; 37:669–79.11. Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, et al. Evolution of diaphragm thickness during mechanical ventilation. impact of inspiratory effort. Am J Respir Crit Care Med. 2015; 192:1080–8.
Article12. Mayo P, Volpicelli G, Lerolle N, Schreiber A, Doelken P, Vieillard-Baron A. Ultrasonography evaluation during the weaning process: the heart, the diaphragm, the pleura and the lung. Intensive Care Med. 2016; 42:1107–17.
Article13. Matamis D, Soilemezi E, Tsagourias M, Akoumianaki E, Dimassi S, Boroli F, et al. Sonographic evaluation of the diaphragm in critically ill patients: technique and clinical applications. Intensive Care Med. 2013; 39:801–10.
Article14. Pirompanich P, Romsaiyut S. Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J Intensive Care. 2018; 6:6.
Article15. Ali ER, Mohamad AM. Diaphragm ultrasound as a new functional and morphological index of outcome, prognosis and discontinuation from mechanical ventilation in critically ill patients and evaluating the possible protective indices against VIDD. Egypt J Chest Dis Tuberc. 2017; 66:339–51.
Article16. Osman AM, Hashim RM. Diaphragmatic and lung ultrasound application as new predictive indices for the weaning process in ICU patients. Egypt J Radiol Nucl Med. 2017; 48:61–6.
Article17. Yoo JW, Lee SJ, Lee JD, Kim HC. Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success. Korean J Intern Med. 2018; 33:331–9.
Article18. Spadaro S, Grasso S, Mauri T, Dalla Corte F, Alvisi V, Ragazzi R, et al. Can diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? The role of diaphragmatic rapid shallow breathing index. Crit Care. 2016; 20:305.
Article19. Farghaly S, Hasan AA. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care. 2017; 30:37–43.
Article20. Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrillo A. Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med. 2017; 43:29–38.
Article21. Danaga AR, Gut AL, Antunes LC, Ferreira AL, Yamaguti FA, Christovan JC, et al. Evaluation of the diagnostic performance and cut-off value for the rapid shallow breathing index in predicting extubation failure. J Bras Pneumol. 2009; 35:541–7.22. Boutou AK, Abatzidou F, Tryfon S, Nakou C, Pitsiou G, Argyropoulou P, et al. Diagnostic accuracy of the rapid shallow breathing index to predict a successful spontaneous breathing trial outcome in mechanically ventilated patients with chronic obstructive pulmonary disease. Heart Lung. 2011; 40:105–10.
Article23. Vidotto MC, Sogame LC, Calciolari CC, Nascimento OA, Jardim JR. The prediction of extubation success of postoperative neurosurgical patients using frequency-tidal volume ratios. Neurocrit Care. 2008; 9:83–9.
Article24. Verceles AC, Diaz-Abad M, Geiger-Brown J, Scharf SM. Testing the prognostic value of the rapid shallow breathing index in predicting successful weaning in patients requiring prolonged mechanical ventilation. Heart Lung. 2012; 41:546–52.
Article25. Teixeira C, Zimermann Teixeira PJ, Hohër JA, de Leon PP, Brodt SF, da Siva Moreira J. Serial measurements of f/VT can predict extubation failure in patients with f/VT < or = 105? J Crit Care. 2008; 23:572–6.26. Shah NG, Lee B, Colice G. Analysis of rapid shallow breathing index as a predictor for successful extubation from mechanical ventilation. Chest. 2004; 126:756S.
Article27. DiNino E, Gartman EJ, Sethi JM, McCool FD. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax. 2014; 69:423–7.
Article28. Demoule A, Jung B, Prodanovic H, Molinari N, Chanques G, Coirault C, et al. Diaphragm dysfunction on admission to the intensive care unit: prevalence, risk factors, and prognostic impact-a prospective study. Am J Respir Crit Care Med. 2013; 188:213–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Weaning Approach with Weaning Index for Postoperative Patients with Mechanical Ventilator Support in the ICU
- The role of diaphragmatic thickness measurement in weaning prediction and its comparison with rapid shallow breathing index: a single-center experience
- Role of Bedside Ultrasonography in Assessment of Diaphragm Function as a Predictor of Success of Weaning in Mechanically Ventilated Patients
- Diaphragm ultrasound in weaning from mechanical ventilation: a last step to predict successful extubation?
- Enhancing breathing through inspiratory muscle training in patients with myasthenia gravis on mechanical ventilation: a case report