Korean J Pain.
2022 Apr;35(2):209-223. 10.3344/kjp.2022.35.2.209.
Impact of coronavirus disease 2019 on patients with chronic pain: multicenter study in Korea
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University School of Medicine, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Inje University Sanggye Paik Hospital, Seoul, Korea
- 3Department of Anesthesiology and Pain Medicine, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea
- 4Department of Anesthesiology and Pain Medicine, Jeong-clinic, Seoul, Korea
- 5Department of Anesthesiology and Pain Medicine, Inje University Seoul Paik Hospital, Seoul, Korea
- 6Department of Anesthesiology and Pain Medicine, Jeju National University School of Medicine, Jeju, Korea
- 7Department of Anesthesiology and Pain Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- KMID: 2527772
- DOI: http://doi.org/10.3344/kjp.2022.35.2.209
Abstract
- Background
The coronavirus disease 2019 (COVID-19) pandemic has caused significant changes. This study aimed to investigate the impact of COVID-19 on patients with chronic pain.
Methods
Patients with chronic pain from 23 university hospitals in South Korea participated in this study. The anonymous survey questionnaire consisted of 25 questions regarding the following: demographic data, diagnosis, hospital visit frequency, exercise duration, time outside, sleep duration, weight change, nervousness and anxiety, depression, interest or pleasure, fatigue, daily life difficulties, and self-harm thoughts. Depression severity was evaluated using the Patient Health Questionnaire-9 (PHQ-9). Logistic regression analysis was used to investigate the relationship between increased pain and patient factors.
Results
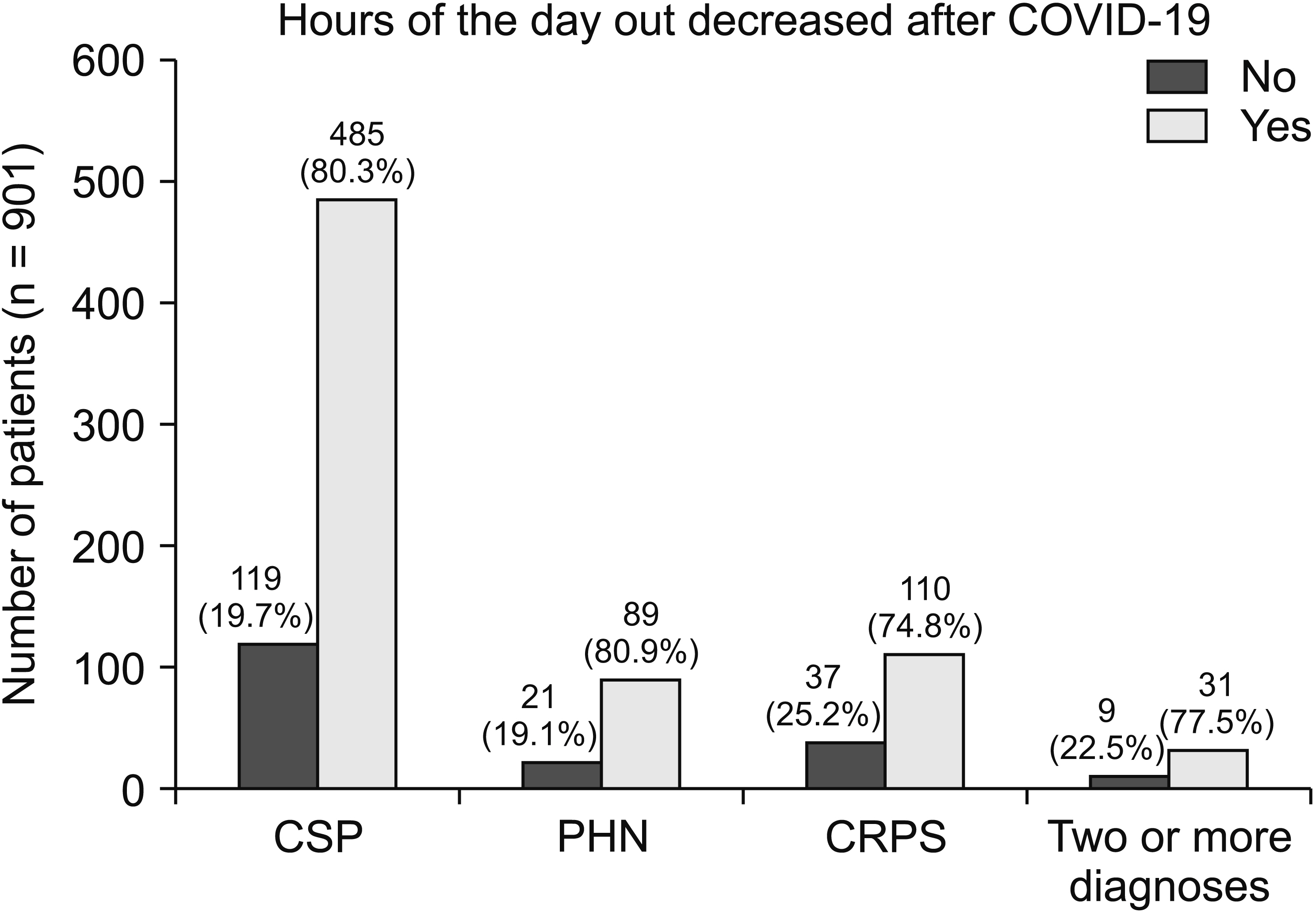
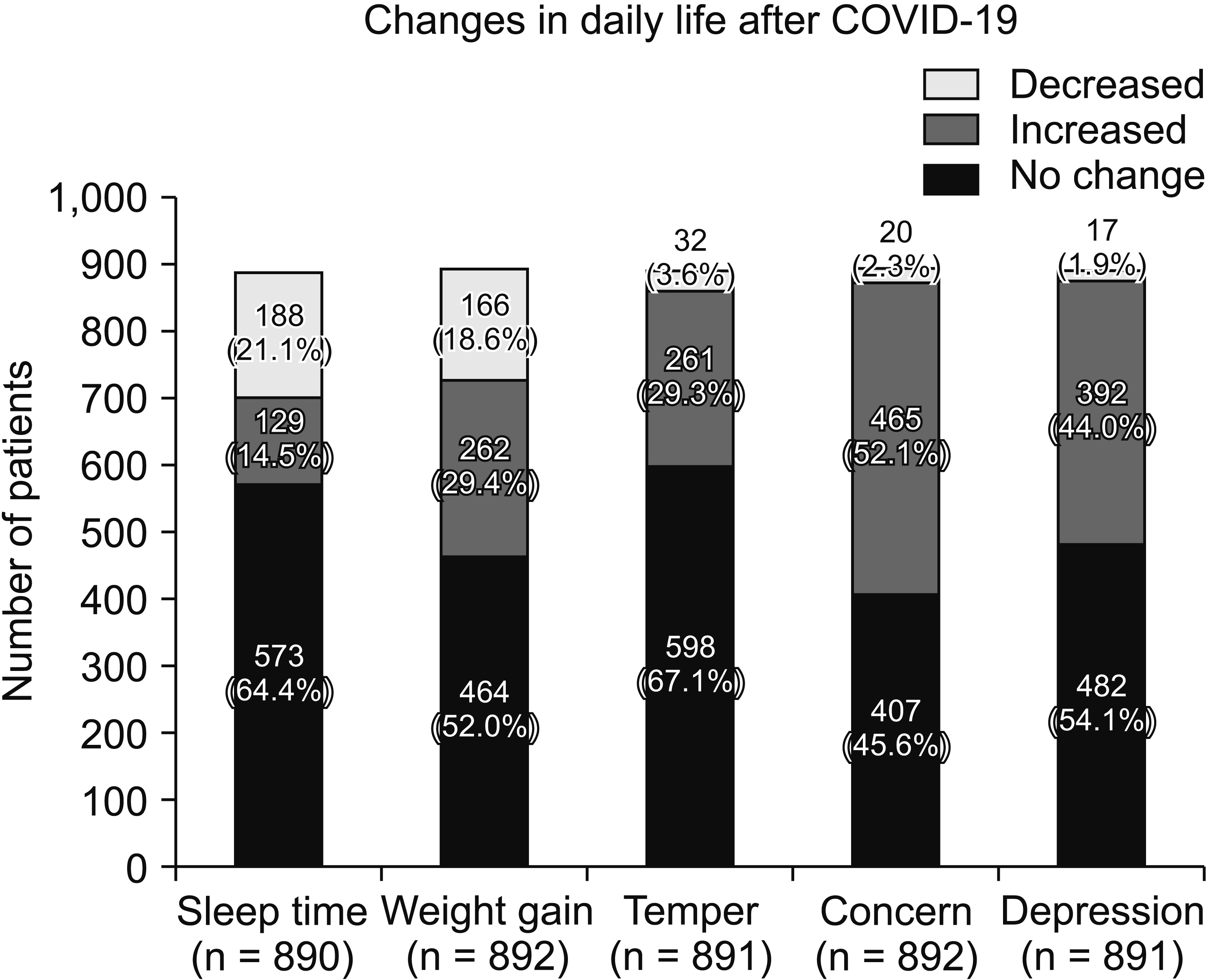
A total of 914 patients completed the survey, 35.9% of whom had decreased their number of visits to the hospital, mostly due to COVID-19. The pain level of 200 patients has worsened since the COVID-19 outbreak, which was more prominent in complex regional pain syndrome (CRPS). Noticeable post-COVID-19 changes such as exercise duration, time spent outside, sleep patterns, mood, and weight affected patients with chronic pain. Depression severity was more significant in patients with CRPS. The total PHQ-9 average score of patients with CRPS was 15.5, corresponding to major depressive orders. The patients’ decreased exercise duration, decreased sleep duration, and increased depression were significantly associated with increased pain.
Conclusions
COVID-19 has caused several changes in patients with chronic pain. During the pandemic, decreased exercise and sleep duration and increased depression were associated with patients’ increasing pain.
Keyword
Figure
Cited by 1 articles
-
Transition of COVID-19 to endemic phase and emergence of COVID-19 related neuropathic pain
Jeong Il Choi
Korean J Pain. 2022;35(3):237-239. doi: 10.3344/kjp.2022.35.3.237.
Reference
-
1. Karos K, McParland JL, Bunzli S, Devan H, Hirsh A, Kapos FP, et al. 2020; The social threats of COVID-19 for people with chronic pain. Pain. 161:2229–35. DOI: 10.1097/j.pain.0000000000002004. PMID: 32694381. PMCID: PMC7382418.
Article2. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. 2020; Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 7:547–60. DOI: 10.1016/S2215-0366(20)30168-1. PMID: 32304649. PMCID: PMC7159850.
Article3. Choi EPH, Hui BPH, Wan EYF. 2020; Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 17:3740. DOI: 10.3390/ijerph17103740. PMID: 32466251. PMCID: PMC7277420. PMID: b72fa842c3694addb75ad55ffe49d3d4.
Article4. Killgore WDS, Cloonan SA, Taylor EC, Dailey NS. 2020; Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 290:113117. DOI: 10.1016/j.psychres.2020.113117. PMID: 32480121. PMCID: PMC7255345.
Article5. Shah SMA, Mohammad D, Qureshi MFH, Abbas MZ, Aleem S. 2021; Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the Coronavirus Disease (COVID-19) pandemic. Community Ment Health J. 57:101–10. DOI: 10.1007/s10597-020-00728-y. PMID: 33108569. PMCID: PMC7590908.
Article6. Petzold MB, Bendau A, Plag J, Pyrkosch L, Mascarell Maricic L, Betzler F, et al. 2020; Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 10:e01745. DOI: 10.1002/brb3.1745. PMID: 32633464. PMCID: PMC7361063. PMID: e4225f147d254c40aebd128dc1f50af4.
Article7. Griffin KM, Karas MG, Ivascu NS, Lief L. 2020; Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 201:1337–44. DOI: 10.1164/rccm.202004-1037CP. PMID: 32298146. PMCID: PMC7258631.
Article8. MacIntyre CR, Wang Q. 2020; Physical distancing, face masks, and eye protection for prevention of COVID-19. Lancet. 395:1950–1. Erratum in: Lancet 2020; 395: 1972. DOI: 10.1016/S0140-6736(20)31183-1. PMID: 32497511. PMCID: PMC7263820.
Article9. Hruschak V, Flowers KM, Azizoddin DR, Jamison RN, Edwards RR, Schreiber KL. 2021; Cross-sectional study of psychosocial and pain-related variables among patients with chronic pain during a time of social distancing imposed by the coronavirus disease 2019 pandemic. Pain. 162:619–29. DOI: 10.1097/j.pain.0000000000002128. PMID: 33230007. PMCID: PMC7808279.
Article10. Park GE, Ko JH, Peck KR, Lee JY, Lee JY, Cho SY, et al. 2016; Control of an outbreak of Middle East respiratory syndrome in a tertiary hospital in Korea. Ann Intern Med. 165:87–93. DOI: 10.7326/M15-2495. PMID: 27272273.
Article11. Hämmig O. 2019; Health risks associated with social isolation in general and in young, middle and old age. PLoS One. 14:e0219663. Erratum in: PLoS One 2019; 14: e0222124. DOI: 10.1371/journal.pone.0222124. PMID: 31465506. PMCID: PMC6715192. PMID: 1d35ce26a9064b6ca69ec2d1de140638.
Article12. Mogil JS. 2015; Social modulation of and by pain in humans and rodents. Pain. 156 Suppl 1:S35–41. DOI: 10.1097/01.j.pain.0000460341.62094.77. PMID: 25789435.
Article13. Karayannis NV, Baumann I, Sturgeon JA, Melloh M, Mackey SC. 2019; The impact of social isolation on pain interference: a longitudinal study. Ann Behav Med. 53:65–74. DOI: 10.1093/abm/kay017. PMID: 29668841. PMCID: PMC6301311.
Article14. Jeong S, An J, Cho S. 2021; Role of affective instability on suicidal risk in complex regional pain syndrome: a diary approach (preliminary report). Korean J Pain. 34:94–105. DOI: 10.3344/kjp.2021.34.1.94. PMID: 33380572. PMCID: PMC7783859.
Article15. Blyth FM, March LM, Brnabic AJ, Cousins MJ. 2004; Chronic pain and frequent use of health care. Pain. 111:51–8. DOI: 10.1016/j.pain.2004.05.020. PMID: 15327808.
Article16. Kroenke K, Spitzer RL, Williams JB. 2001; The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 16:606–13. DOI: 10.1046/j.1525-1497.2001.016009606.x. PMID: 11556941. PMCID: PMC1495268.17. Ford J, Thomas F, Byng R, McCabe R. 2020; Use of the Patient Health Questionnaire (PHQ-9) in practice: interactions between patients and physicians. Qual Health Res. 30:2146–59. DOI: 10.1177/1049732320924625. PMID: 32564676. PMCID: PMC7549295.
Article18. Levis B, Benedetti A, Thombs BD. DEPRESsion Screening Data (DEPRESSD) Collaboration. 2019; Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 365:l1476. Erratum in: BMJ 2019; 365: l1781. DOI: 10.1136/bmj.l1476. PMID: 30967483. PMCID: PMC6454318.
Article19. Park KY. 2017; Reliability, validity and clinical usefulness of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Glob Health Nurs. 7:71–8. http://journal.kci.go.kr/rins/archive/articleView?artiId=ART002249208. DOI: 10.35144/ghn.2017.7.2.71.
Article20. Levis B, Sun Y, He C, Wu Y, Krishnan A, Bhandari PM, et al. 2020; Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: systematic review and meta-analysis. JAMA. 323:2290–300. DOI: 10.1001/jama.2020.6504. PMID: 32515813. PMCID: PMC7284301.
Article21. Manea L, Gilbody S, McMillan D. 2015; A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry. 37:67–75. DOI: 10.1016/j.genhosppsych.2014.09.009. PMID: 25439733.
Article22. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. 2009; Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 31:318–26. DOI: 10.1016/j.genhosppsych.2009.03.001. PMID: 19555791. PMCID: PMC7112501.
Article23. Galer BS, Henderson J, Perander J, Jensen MP. 2000; Course of symptoms and quality of life measurement in Complex Regional Pain Syndrome: a pilot survey. J Pain Symptom Manage. 20:286–92. DOI: 10.1016/S0885-3924(00)00183-4. PMID: 11027911.24. Li LW, Chew AMK, Gunasekeran DV. 2020; Digital health for patients with chronic pain during the COVID-19 pandemic. Br J Anaesth. 125:657–60. DOI: 10.1016/j.bja.2020.08.003. PMID: 32863018. PMCID: PMC7416745.
Article25. Consonni M, Telesca A, Grazzi L, Cazzato D, Lauria G. 2021; Life with chronic pain during COVID-19 lockdown: the case of patients with small fibre neuropathy and chronic migraine. Neurol Sci. 42:389–97. DOI: 10.1007/s10072-020-04890-9. PMID: 33205374. PMCID: PMC7670980.
Article26. Savaş S, Baloğlu HH, Ay G, Cerçi SS. 2009; The effect of sequel symptoms and signs of Complex Regional Pain Syndrome type 1 on upper extremity disability and quality of life. Rheumatol Int. 29:545–50. DOI: 10.1007/s00296-008-0748-8. PMID: 18953539.
Article27. Lee J, Lim YH, Hong SJ, Jeong JH, Choi HR, Park SK, et al. 2021; Multicenter survey of symptoms, work life, economic status, and quality of life of complex regional pain syndrome patients. Korean J Pain. 34:288–303. DOI: 10.3344/kjp.2021.34.3.288. PMID: 34193635. PMCID: PMC8255153.
Article28. Geertzen JH, Dijkstra PU, van Sonderen EL, Groothoff JW, ten Duis HJ, Eisma WH. 1998; Relationship between impairments, disability and handicap in reflex sympathetic dystrophy patients: a long-term follow-up study. Clin Rehabil. 12:402–12. DOI: 10.1191/026921598676761735. PMID: 9796931.
Article29. Velavan TP, Meyer CG. 2020; The COVID-19 epidemic. Trop Med Int Health. 25:278–80. DOI: 10.1111/tmi.13383. PMID: 32052514. PMCID: PMC7169770.
Article30. Moraes EN, Viana LG, Resende LMH, Vasconcellos LS, Moura AS, Menezes A, et al. 2020; COVID-19 in long-term care facilities for the elderly: laboratory screening and disease dissemination prevention strategies. Cien Saude Colet. 25:3445–58. DOI: 10.1590/1413-81232020259.20382020. PMID: 32876277.31. Huang Y, Wang Y, Zeng L, Yang J, Song X, Rao W, et al. 2020; Prevalence and correlation of anxiety, insomnia and somatic symptoms in a Chinese population during the COVID-19 epidemic. Front Psychiatry. 11:568329. DOI: 10.3389/fpsyt.2020.568329. PMID: 33005165. PMCID: PMC7485113. PMID: 39733ca5377e44b6b5e5b09deba8f459.
Article32. Zhai L, Zhang H, Zhang D. 2015; Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 32:664–70. DOI: 10.1002/da.22386. PMID: 26047492.
Article33. Schuh-Hofer S, Wodarski R, Pfau DB, Caspani O, Magerl W, Kennedy JD, et al. 2013; One night of total sleep deprivation promotes a state of generalized hyperalgesia: a surrogate pain model to study the relationship of insomnia and pain. Pain. 154:1613–21. DOI: 10.1016/j.pain.2013.04.046. PMID: 23707287.
Article34. Xu Z, Su H, Zou Y, Chen J, Wu J, Chang W. 2012; Sleep quality of Chinese adolescents: distribution and its associated factors. J Paediatr Child Health. 48:138–45. DOI: 10.1111/j.1440-1754.2011.02065.x. PMID: 21470332.
Article35. Kim SH, Sun JM, Yoon KB, Moon JH, An JR, Yoon DM. 2015; Risk factors associated with clinical insomnia in chronic low back pain: a retrospective analysis in a university hospital in Korea. Korean J Pain. 28:137–43. DOI: 10.3344/kjp.2015.28.2.137. PMID: 25852836. PMCID: PMC4387459.
Article36. O'Donoghue GM, Fox N, Heneghan C, Hurley DA. 2009; Objective and subjective assessment of sleep in chronic low back pain patients compared with healthy age and gender matched controls: a pilot study. BMC Musculoskelet Disord. 10:122. DOI: 10.1186/1471-2474-10-122. PMID: 19799778. PMCID: PMC2765952.37. Kelly GA, Blake C, Power CK, O'Keeffe D, Fullen BM. 2011; The association between chronic low back pain and sleep: a systematic review. Clin J Pain. 27:169–81. DOI: 10.1097/AJP.0b013e3181f3bdd5. PMID: 20842008.38. Lee HJ, Choi EJ, Nahm FS, Yoon IY, Lee PB. 2018; Prevalence of unrecognized depression in patients with chronic pain without a history of psychiatric diseases. Korean J Pain. 31:116–24. DOI: 10.3344/kjp.2018.31.2.116. PMID: 29686810. PMCID: PMC5904346.
Article39. Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K. 2008; Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 70:890–7. DOI: 10.1097/PSY.0b013e318185c510. PMID: 18799425. PMCID: PMC2902727.
Article40. Bair MJ, Robinson RL, Katon W, Kroenke K. 2003; Depression and pain comorbidity: a literature review. Arch Intern Med. 163:2433–45. DOI: 10.1001/archinte.163.20.2433. PMID: 14609780.41. Ten Brink AF, Peters L, Kompouli PI, Jordan A, McCabe CS, Goebel A, et al. 2020; Bodily changes and sensory sensitivity in complex regional pain syndrome and fibromyalgia. Pain. 161:1361–70. DOI: 10.1097/j.pain.0000000000001830. PMID: 32049896.
Article42. Chan DX, Lin XF, George JM, Liu CW. 2020; Clinical challenges and considerations in management of chronic pain patients during a COVID-19 pandemic. Ann Acad Med Singap. 49:669–73. DOI: 10.47102/annals-acadmedsg.2020130. PMID: 33241255.
Article43. Lassen CL, Siam L, Degenhart A, Klier TW, Bundscherer A, Lindenberg N. 2021; Short-term impact of the COVID-19 pandemic on patients with a chronic pain disorder. Medicine (Baltimore). 100:e25153. DOI: 10.1097/MD.0000000000025153. PMID: 33725917. PMCID: PMC7969217.
Article44. O'Brien EM, Waxenberg LB, Atchison JW, Gremillion HA, Staud RM, McCrae CS, et al. 2011; Intraindividual variability in daily sleep and pain ratings among chronic pain patients: bidirectional association and the role of negative mood. Clin J Pain. 27:425–33. DOI: 10.1097/AJP.0b013e318208c8e4. PMID: 21415723.45. Gilan D, Röthke N, Blessin M, Kunzler A, Stoffers-Winterling J, Müssig M, et al. 2020; Psychomorbidity, resilience, and exacerbating and protective factors during the SARS-CoV-2 pandemic. Dtsch Arztebl Int. 117:625–30. DOI: 10.3238/arztebl.2020.0625. PMID: 33200744. PMCID: PMC7817784.
Article46. Serrano-Ibáñez ER, Esteve R, Ramírez-Maestre C, Ruiz-Párraga GT, López-Martínez AE. 2021; Chronic pain in the time of COVID-19: stress aftermath and central sensitization. Br J Health Psychol. 26:544–52. DOI: 10.1111/bjhp.12483. PMID: 33099793.
Article47. Sim K, Huak Chan Y, Chong PN, Chua HC, Wen Soon S. 2010; Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res. 68:195–202. DOI: 10.1016/j.jpsychores.2009.04.004. PMID: 20105703. PMCID: PMC7094450.
Article48. Park SJ, Choi HR, Choi JH, Kim K, Hong JP. 2010; Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Anxiety Mood. 6:119–24. https://www.koreascience.or.kr/article/JAKO201025247234261.page.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The coronavirus disease 2019 pandemic and chronic diseases
- Erratum: Impact of coronavirus disease 2019 on patients with chronic pain: multicenter study in Korea
- Are Patients with Asthma and Chronic Obstructive Pulmonary Disease Preferred Targets of COVID-19?
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)-Associated Urogenital Disease: A Current Update