J Cerebrovasc Endovasc Neurosurg.
2022 Mar;24(1):73-78. 10.7461/jcen.2022.E2021.05.002.
Endoport-assisted microsurgical treatment for a ruptured posterior cerebral artery aneurysm: A technical note
- Affiliations
-
- 1Department of Skull-Base Neurosurgery, National Institute of Neurology and Neurosurgery Manuel Velasco Sáurez, Mexico City, Mexico
- 2Department of Neurosurgery, National Institute of Neurology and Neurosurgery Manuel Velasco Sáurez, Mexico City, Mexico
- KMID: 2527598
- DOI: http://doi.org/10.7461/jcen.2022.E2021.05.002
Abstract
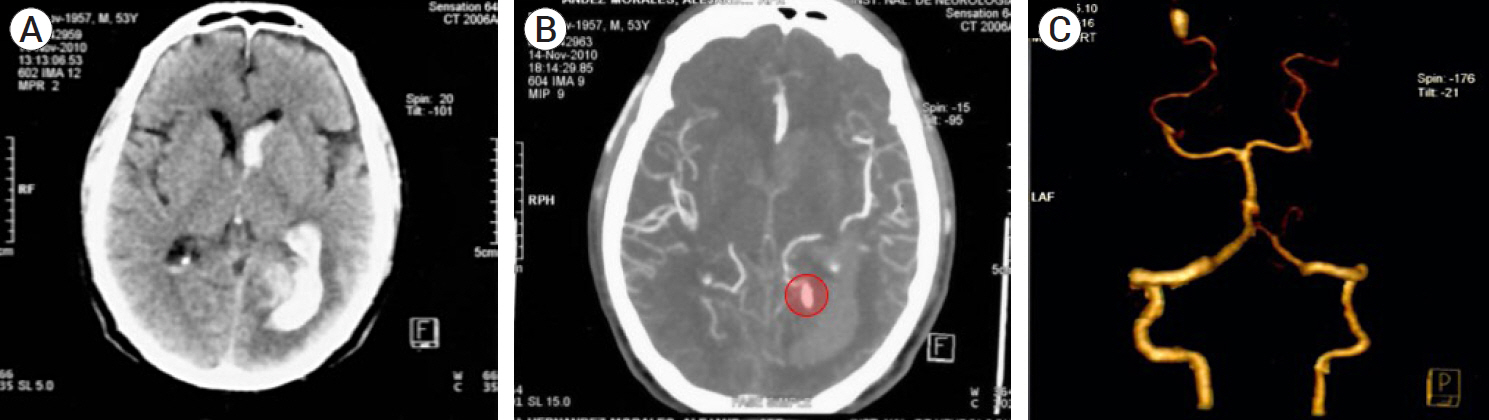
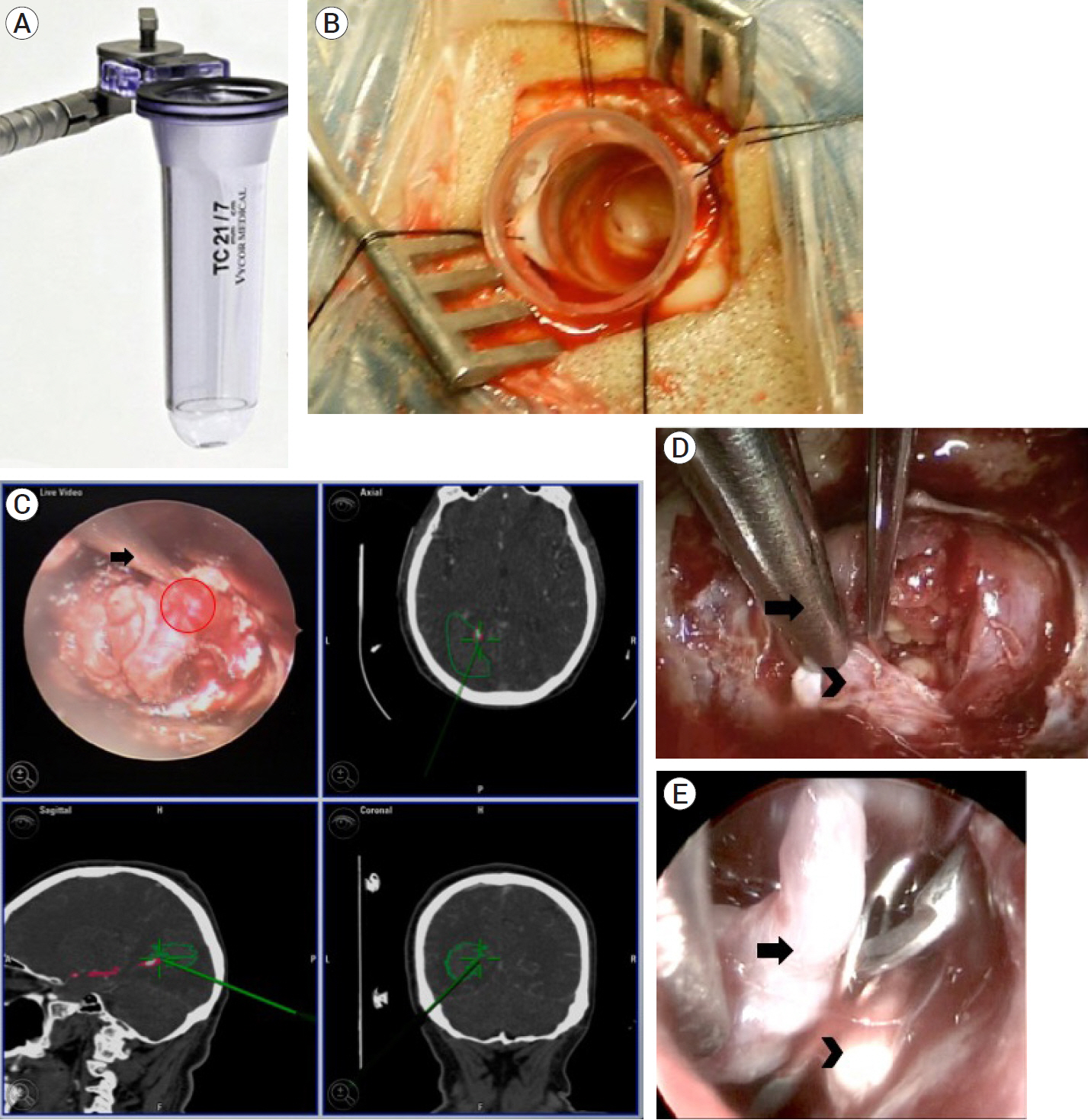
- Posterior Cerebral Artery aneurysms are scarce, yet its territory is frequently associated to large and giant aneurysms. Treatment is mostly a binary option between microsurgical clipping and endovascular coiling. Hybrid approaches are an option too, whereas innovation with less frequent techniques such as endoscope-controlled and endoscope-assisted procedure may provide a safer surgical approach with same successful results. Hereby we report a case of a 53 years old male examined at the ER after presenting generalized seizures and altered state of consciousness. Upon arrival, neurological evaluation revealed homonymous right hemianopia. Computed tomography (CT) scan revealed a subarachnoid hemorrhage and left parieto-occipital intraparenchymal hemorrhage with intraventricular extension; computed tomography angiogram (CTA) revealed an aneurysm at the left posterior cerebral artery (PCA) in its P4 segment. We performed a vascular exploration with drainage of the occipital and intraventricular hematoma through a single endoscopic port through transulcal approach guided by neuronavigation, in addition to clipping and aneurysmectomy. The combination of microsurgical clipping with previous Endoport-guided endoscopic procedure may be a surgical-operative option that not only may facilitate the approach to the desired lesion, but also provides a safer surgical scenario.
Keyword
Figure
Reference
-
1. Ciceri EF, Klucznik RP, Grossman RG, Rose JE, Mawad ME. Aneurysms of the posterior cerebral artery: classification and endovascular treatment. AJNR Am J Neuroradiol. 2001; Jan. 22(1):27–34.2. Ding D, Starke RM, Crowley RW, Liu KC. Endoport-assisted microsurgical resection of cerebral cavernous malformations. J Clin Neurosci. 2015; Jun. 22(6):1025–9.
Article3. Drake CG. Giant posterior cerebral aneurysms: 66 patients. In : Drake CG, Peerless SJ, Hruesniemi JA, editors. Surgery of Vertebrobasilar Aneurysms: London, Ontario, Experience on 1767 Patients. New York: Springer Verlag;1996. p. 230–48.4. Ferrante L, Acqui M, Trillo G, Lunardi P, Fortuna A. Aneurysms of the posterior cerebral artery: do they present specific characteristics? Acta Neurochir (Wien). 1996; 138(7):840–52.
Article5. Fischer J, Mustafa H. Endoscopic-guided clipping of cerebral aneurysms. Br J Neurosurg. 1994; 8(5):559–65.
Article6. Gerber CJ, Neil-Dwyer G. A review of the management of 15 cases of aneurysms of the posterior cerebral artery. Br J Neurosurg. 1992; 6(6):521–7.
Article7. Honda M, Tsutsumi K, Yokoyama H, Yonekura N, Nagata I. Aneurysms of the posterior cerebral artery: retrospective review of surgical treatment. Neurol Med Chir (Tokyo). 2004; Apr. 44(4):164–8.
Article8. Hopf NJ, Perneczky A. Endoscopic neurosurgery and endoscope-assisted microneurosurgery for the treatment on intracranial cysts. Neurosurgery. 1998; Dec. 43(6):1330–6.
Article9. Jo KW, Shin HJ, Nam DH, Lee JI, Park K, Kim JH, et al. Efficacy of endoport-guided endoscopic resection for deep-seated brain lesions. Neurosur Rev. 2011; Oct. 34(4):457–63.
Article10. Locksley HB. Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg. 1966; Aug. 25(2):219–39.11. Longatti P, Fiorindi A, Di Paola F, Curtolo S, Basaldella L, Martinuzzi A. Coiling and neuroendoscopy: a new perspective in the treatment of intraventricular haemorrhages due to bleeding aneurysms. J Neurol Neurosurg Psychiatry. 2006; Dec. 77(12):1354–8.
Article12. Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. STICH investigators. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Hemorrhage (STICH): a randomized trial. Lancet. 2005; Jan 29-Feb 4. 365(9457):387–97.13. Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomized trial. Lancet. 2013; Aug. 382(9890):397–408.
Article14. Perneczky A, Boecher-Schwarz HG. Endoscope-assisted microsurgery for cerebral aneurysms. Neurol Med Chir (Tokyo). 1998; 38(Suppl):33–4.
Article15. Pia HW, Fontana H. Aneurysms of the posterior cerebral artery. Locations and clinical pictures. Acta Neurochir (Wien). 1977; 38(1-2):13–35.
Article16. Rhoton AL Jr. The supratentorial arteries. Neurosurgery. 2002; Oct. 51(4 Suppl):S53–120.
Article17. Schroeder HWS. General principles and intraventricular neuroendoscopy: endoscopic techniques. World Neurosurg. 2013; Feb. 79(2 Suppl):S14.e23–8.
Article18. Terasaka S, Sawamura Y, Kamiyama H, Fukushima T. Surgical approaches for the treatment of aneurysms on the P2 segment of the posterior cerebral artery. Neurosurgery. 2000; Aug. 47(2):359–64. discussion 364-6.
Article19. Wong J, Tymianski R, Radovanovic I, Tymianski M. Minimally invasive surgery for cerebral aneurysms. Stroke. 2015; Sep. 46(9):2699–706.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coil Embolization for Distal Middle Cerebral Artery Aneurysm
- Microsurgical Anatomy of the Basilar Artery and Posterior Cerebral Artery
- Subdural Hematoma Due to Ruptured Intracerebral Aneurysm
- Fusiform “True” Posterior Communicating Artery Aneurysm with Basilar Artery Occlusion: A Case Report
- Traumatic Rupture of Middle Cerebral Artery Aneurysm