J Cerebrovasc Endovasc Neurosurg.
2022 Mar;24(1):24-35. 10.7461/jcen.2021.E2021.07.009.
The effectiveness of systemic and endovascular intra-arterial thrombectomy protocol for decreasing door-to-recanalization time duration
- Affiliations
-
- 1Department of Neurosurgery, Keimyung University, Dong-San Medical Center, Daegu, Korea
- 2Department of Neurology, Keimyung University, Dong-San Medical Center, Daegu, Korea
- KMID: 2527592
- DOI: http://doi.org/10.7461/jcen.2021.E2021.07.009
Abstract
Objective
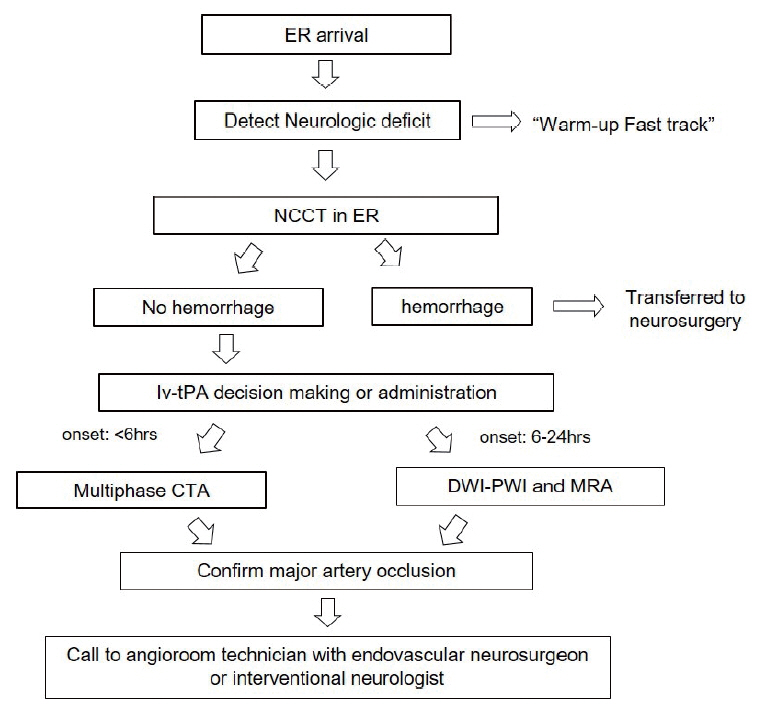
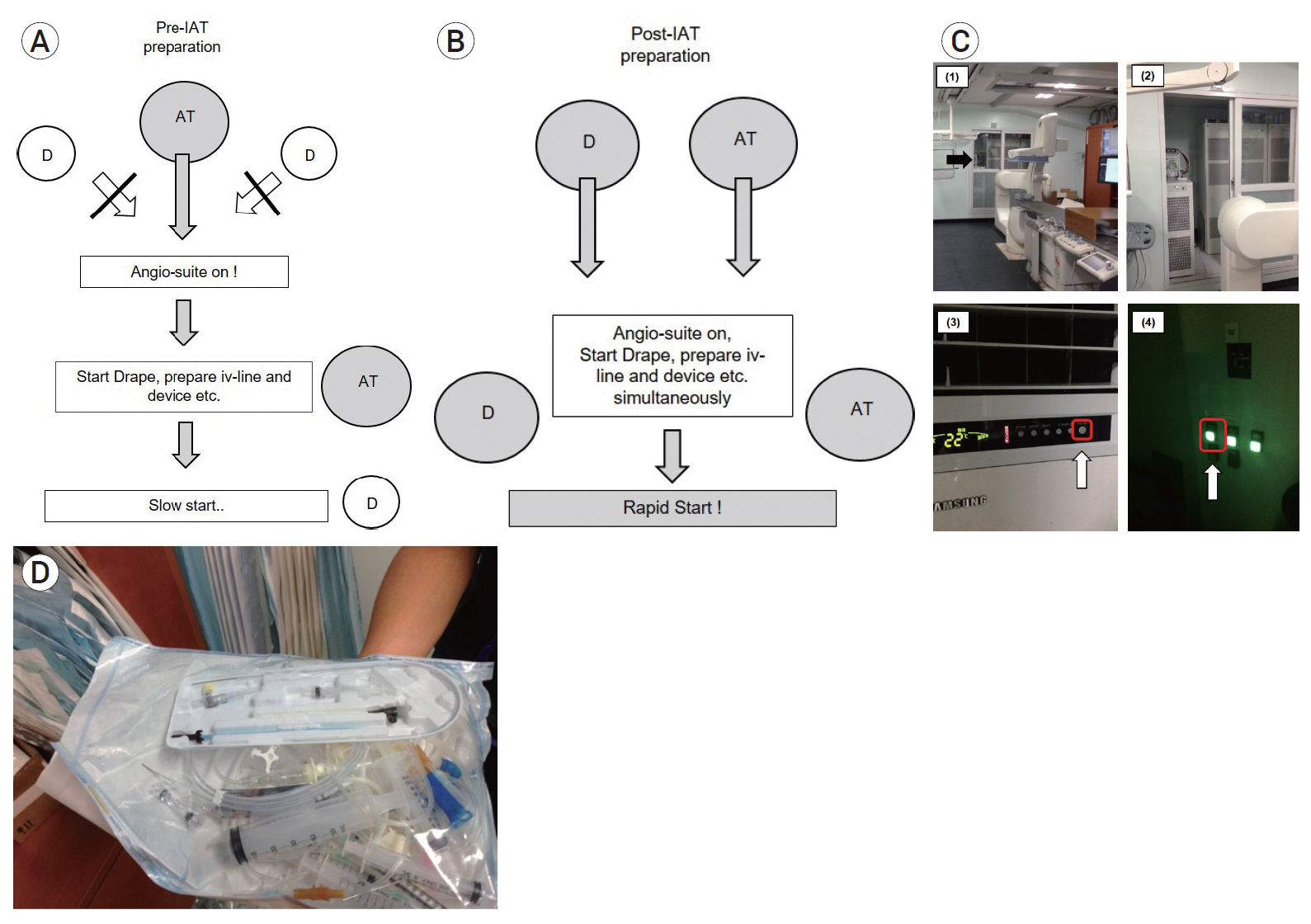
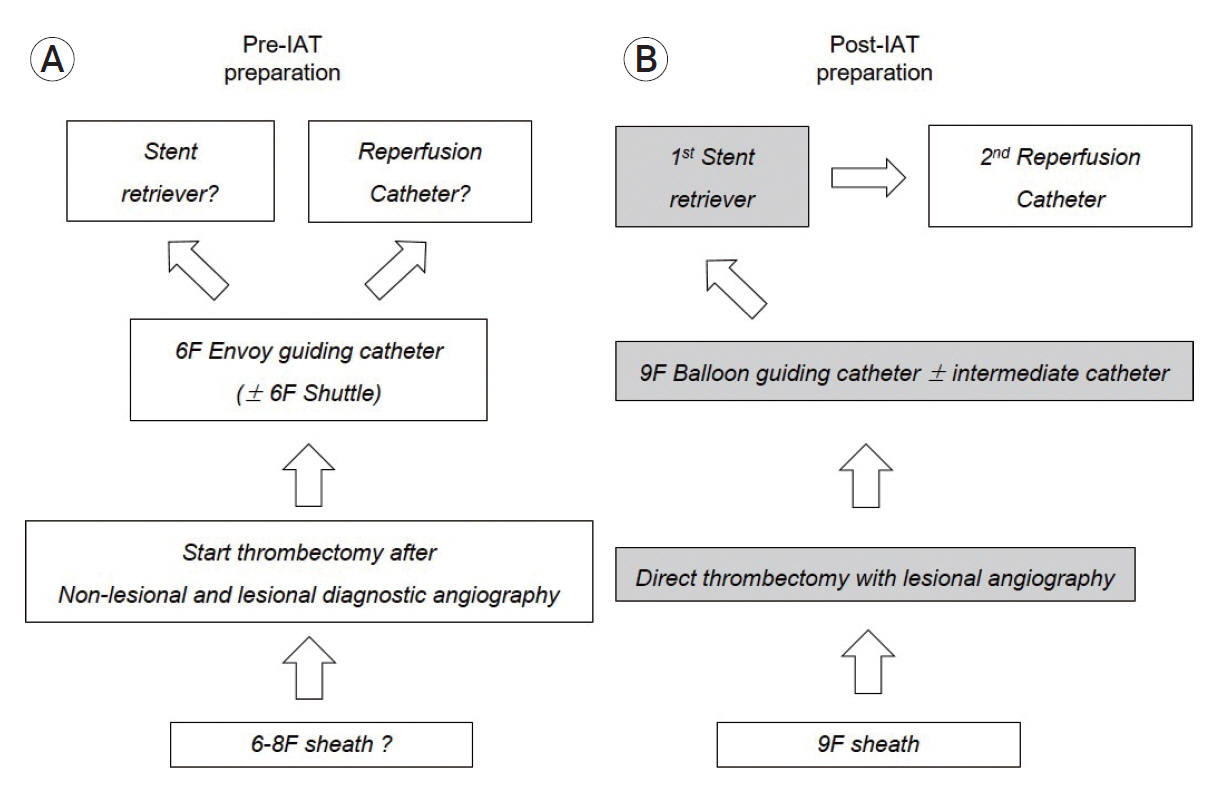
Variable treatment strategies and protocols have been applied to reduce time durations in the process of acute stroke management. The aim of this study is to investigate the effectiveness of our intra-arterial thrombectomy (IAT) protocol for decreasing door-to-recanalization time duration and improve successful recanalization.
Methods
A systemic and endovascular protocol included door-to-image, image-to-puncture and puncture-to-recanalization. We retrospectively analyzed the patients of pre- (Sep 2012–Apr 2014) and post-IAT protocol (May 2014–Jul 2018). Univariate analysis was used for the statistical significance according to variable factors (age, gender, the location of occluded vessel, successful recanalization TICI 2b-3). Independent t-test was used to compare the time duration.
Results
Among all 267 patients with acute stroke of anterior circulation, there were 50 and 217 patients with pre- and post-IAT protocol. Age, gender, and the location of occluded vessel have no statistical significance (p>0.05). In pre- and post-IAT group, successful recanalization was 39 of 50 (78.0%) and 185/217 (85.3%), respectively (p<0.05). Post-IAT (48.8%, 106/217) group had a higher tendency of good outcome than pre-IAT group (36.0%, 18/50) (p>0.05). Pre- and post-IAT group showed 61.7±21.4 vs. 25±16.0 (p<0.05), 102.0±29.8 vs. 82.7±30.4 (min) (p<0.05), and 79.1±47.5 vs. 58.4±75.3 (p<0.05) in three steps, respectively.
Conclusions
We suggest that the application of systemic and endovascular IAT protocols showed a significant time reduction for faster recanalization in patients with LVO. To build-up the well-designed IAT protocol through puncture-to-recanalization can be needed to decrease time duration and improve clinical outcome in recanalization therapy in acute stroke patients.
Figure
Reference
-
1. Aghaebrahim A, Streib C, Rangaraju S, Kenmuir CL, Giurgiutiu DV, Horev A, et al. Streamlining door to recanalization processes in endovascular stroke therapy. J Neurointerv Surg. 2017; Apr. 9(4):340–5.
Article2. Bourcier R, Goyal M, Liebeskind DS, Muir KW, Desal H, Siddiqui AH, et al. Association of time from stroke onset to groin puncture with quality of reperfusion after mechanical thrombectomy: a meta-analysis of individual patient data from 7 randomized clinical trials. JAMA Neurol. 2019; Apr. 76(4):405–11.
Article3. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; Mar. 368(10):893–903.
Article4. Casaubon LK, Boulanger JM, Blacquiere D, Boucher S, Brown K, Goddard T, et al. Canadian stroke best practice recommendations: hyperacute stroke care guidelines, update 2015. Int J Stroke. 2015; Aug. 10(6):924–40.5. Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013; Mar. 368(10):904–13.
Article6. Fennell VS, Setlur Nagesh SV, Meess KM, Gutierrez L, James RH, Springer ME, et al. What to do about fibrin rich ‘tough clots’? Comparing the Solitaire stent retriever with a novel geometric clot extractor in an in vitro stroke model. J Neurointerv Surg. 2018; Sep. 10(9):907–10.
Article7. Frei D, McGraw C, McCarthy K, Whaley M, Bellon RJ, Loy D, et al. A standardized neurointerventional thrombectomy protocol leads to faster recanalization times. J Neurointerv Surg. 2017; Nov. 9(11):1035–40.
Article8. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; Mar. 372(11):1019–30.
Article9. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; Mar. 44(3):870–947.
Article10. Kansagra AP, Meyers GC, Kruzich MS, Cross DT 3rd, Moran CJ. Wide variability in prethrombectomy workflow practices in the United States: a multicenter survey. AJNR Am J Neuroradiol. 2017; Dec. 38(12):2238–42.
Article11. Khatri P, Yeatts SD, Mazighi M, Broderick JP, Liebeskind DS, Demchuk AM, et al. Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol. 2014; Jun. 13(6):567–74.
Article12. Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013; Mar. 7. 368(10):914–23.
Article13. Kim DH, Kim B, Jung C, Nam HS, Lee JS, Kim JW, et al. Consensus statements by Korean Society of Interventional Neuroradiology and Korean Stroke Society: hyperacute endovascular treatment workflow to reduce door-to-reperfusion time. Korean J Radiol. 2018; Sep-Oct. 19(5):838–48.
Article14. Laridan E, Denorme F, Desender L, François O, Andersson T, Deckmyn H, et al. Neutrophil extracellular traps in ischemic stroke thrombi. Ann Neurol. 2017; Aug. 82(2):223–32.
Article15. Leifer D, Bravata DM, Connors JJ 3rd, Hinchey JA, Jauch EC, Johnston SC, et al. Metrics for measuring quality of care in comprehensive stroke centers: detailed follow-up to Brain Attack Coalition comprehensive stroke center recommendations: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; Mar. 42(3):849–77.
Article16. Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012; Jul. 5(4):514–22.
Article17. McDonald JS, Brinjikji W, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF. Conscious sedation versus general anaesthesia during mechanical thrombectomy for stroke: a propensity score analysis. J Neurointerv Surg. 2015; Nov. 7(11):789–94.
Article18. Mehta BP, Leslie-Mazwi TM, Chandra RV, Bell DL, Sun CH, Hirsch JA, et al. Reducing door-to-puncture times for intra-arterial stroke therapy: a pilot quality improvement project. J Am Heart Assoc. 2014; Nov. 3(6):e000963.
Article19. Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM, et al. Multiphase CT angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology. 2015; May. 275(2):510–20.
Article20. Menon BK, Demchuk AM. Computed tomography angiography in the assessment of patients with stroke/TIA. Neurohospitalist. 2011; Oct. 1(4):187–99.
Article21. Panezai S, Meghpara S, Kulhari A, Brar J, Suhan L, Singh A, et al. Institution of code neurointervention and its impact on reaction and treatment times. J Vasc Interv Neurol. 2020; Jan. 11(1):1–5.22. Patel MD, Rose KM, O’Brien EC, Rosamond WD. Prehospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina stroke care collaborative. Stroke. 2011; Aug. 42(8):2263–8.
Article23. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; Oct. 46(10):3020–35.
Article24. Qureshi AI, Egila H, Adil MM, Siddiqi H, Mian N, Hassan AE, et al. “No turn back approach” to reduce treatment time for endovascular treatment of acute ischemic stroke. J Stroke Cerebrovasc Dis. 2014; May-Jun. 23(5):e317–23.
Article25. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; Sep. 316(12):1279–88.
Article26. Schregel K, Behme D, Tsogkas I, Knauth M, Maier I, Karch A, et al. Effects of workflow optimization in endovascularly treated stroke patients - a pre-post effectiveness study. PLoS One. 2016; Dec. 11(12):e0169192.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of an Infection Control Protocol for Coronavirus Disease in Emergency Mechanical Thrombectomy
- Evolution of Endovascular Therapy in Acute Stroke: Implications of Device Development
- Intra-Arterial Thrombolysis to Improve Final Thrombolysis in Cerebral Infarction Score after Thrombectomy: A Case-Series Analysis
- Evidence-Based Changes in Devices and Methods of Endovascular Recanalization Therapy
- Adjuvant Tirofiban Injection Through Deployed Solitaire Stent As a Rescue Technique After failed Mechanical Thrombectomy in Acute Stroke