Clin Endosc.
2022 Mar;55(2):292-296. 10.5946/ce.2021.005.
Endoscopic Treatment of Iatrogenic Perforation of Sigmoid Diverticulum: A Case Report of Multidisciplinary Management
- Affiliations
-
- 1Section of Gastroenterology & Hepatology, Department of Health Promotion Sciences Maternal and Infant Care, Internal Medicine and Medical Specialties, PROMISE, University of Palermo, Palermo, Italy
- 2Department of Surgical, Oncological and Oral Science, Palermo University Hospital, Palermo, Italy
- 3Section of Endoscopy, Department of General Surgery, San Giovanni di Dio Hospital, Agrigento, Italy
- KMID: 2527575
- DOI: http://doi.org/10.5946/ce.2021.005
Abstract
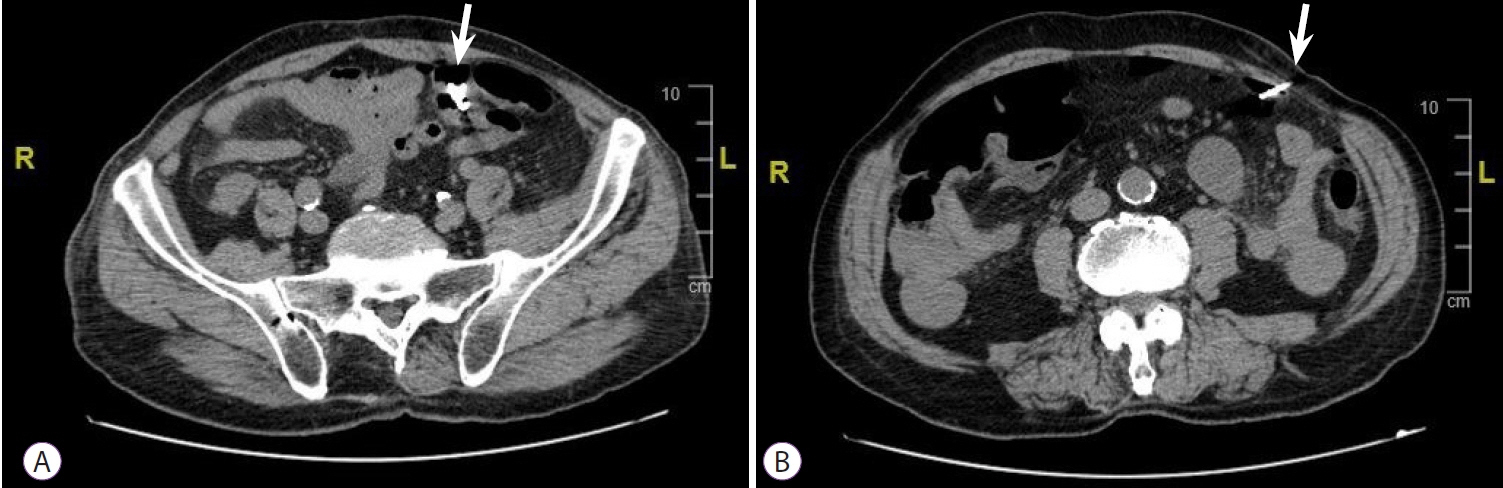
- Iatrogenic perforations are severe complications of gastrointestinal endoscopy; therefore, their management should be adequately planned. A 77-year-old man with a history of diverticulosis underwent a colonoscopy for anemia. During the procedure, an iatrogenic perforation occurred suddenly in the sigmoid colon, near a severe angle among the numerous diverticula. Through-the- scope clips were immediately applied to treat it and close mucosal edges. Laboratory tests showed increased inflammation and infection, and although there were no complaints of abdominal pain, the patient had an extremely distended abdomen. A multidisciplinary board began management based on a conservative approach. Pneumoperitoneum was treated with computed tomography-assisted drainage. After 72 hours, his intestinal canalization and laboratory tests were normal. Though this adverse event is rare, a multidisciplinary board should be promptly gathered upon occurrence, even if the patient appears clinically stable, to consider a conservative approach and avoid surgical treatment.
Keyword
Figure
Reference
-
1. Raju GS, Saito Y, Matsuda T, Kaltenbach T, Soetikno R. Endoscopic management of colonoscopic perforations (with videos). Gastrointest Endosc. 2011; 74:1380–1388.2. Paspatis GA, Arvanitakis M, Dumonceau JM, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement - Update 2020. Endoscopy. 2020; 52:792–810.3. Toyonaga T, Man-i M, East JE, et al. 1,635 Endoscopic submucosal dissection cases in the esophagus, stomach, and colorectum: complication rates and long-term outcomes. Surg Endosc. 2013; 27:1000–1008.4. Paspatis GA, Konstantinidis K, Tribonias G, et al. Sixty- versus thirty-seconds papillary balloon dilation after sphincterotomy for the treatment of large bile duct stones: a randomized controlled trial. Dig Liver Dis. 2013; 45:301–304.5. Mangiavillano B, Caruso A, Manta R, et al. Over-the-scope clips in the treatment of gastrointestinal tract iatrogenic perforation: A multicenter retrospective study and a classification of gastrointestinal tract perforations. World J Gastrointest Surg. 2016; 8:315–320.6. Jayanna M, Burgess NG, Singh R, et al. Cost analysis of endoscopic mucosal resection vs surgery for large laterally spreading colorectal lesions. Clin Gastroenterol Hepatol. 2016; 14:271–8.e82.7. Martínez-Pérez A, de’Angelis N, Brunetti F, et al. Laparoscopic vs. open surgery for the treatment of iatrogenic colonoscopic perforations: a systematic review and meta-analysis. World J Emerg Surg. 2017; 12:8.8. Tursi A, Brandimarte G, Di Mario F, et al. Development and validation of an endoscopic classification of diverticular disease of the colon: the DICA classification. Dig Dis. 2015; 33:68–76.9. de’Angelis N, Di Saverio S, Chiara O, et al. 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation. World J Emerg Surg. 2018; 13:5.10. An SB, Shin DW, Kim JY, Park SG, Lee BH, Kim JW. Decision-making in the management of colonoscopic perforation: a multicentre retrospective study. Surg Endosc. 2016; 30:2914–2921.11. Derbyshire E, Hungin P, Nickerson C, Rutter MD. Colonoscopic perforations in the English National Health Service Bowel Cancer Screening Programme. Endoscopy. 2018; 50:861–870.12. Mai CM, Wen CC, Wen SH, et al. Iatrogenic colonic perforation by colonoscopy: a fatal complication for patients with a high anesthetic risk. Int J Colorectal Dis. 2010; 25:449–454.13. Carpio G, Albu E, Gumbs MA, Gerst PH. Management of colonic perforation after colonoscopy. Report of three cases. Dis Colon Rectum. 1989; 32:624–626.14. Lim DR, Kuk JK, Kim T, Shin EJ. The analysis of outcomes of surgical management for colonoscopic perforations: a 16-years experiences at a single institution. Asian J Surg. 2020; 43:577–584.15. Raju GS. Endoscopic clip closure of gastrointestinal perforations, fistulae, and leaks. Dig Endosc. 2014; 26(Suppl 1):95–104.16. Jung Y. Endoscopic management of iatrogenic colon perforation. Clin Endosc. 2020; 53:29–36.17. Cho SB, Lee WS, Joo YE, et al. Therapeutic options for iatrogenic colon perforation: feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg Endosc. 2012; 26:473–479.18. Saltzman HA, Sieker HO. Intestinal response to changing gaseous environments: normobaric and hyperbaric observations. Ann N Y Acad Sci. 1968; 150:31–39.19. ASGE Technology Committee, Lo SK, Fujii-Lau LL, et al. The use of carbon dioxide in gastrointestinal endoscopy. Gastrointest Endosc. 2016; 83:857–865.20. Memon MA, Memon B, Yunus RM, Khan S. Carbon dioxide versus air insufflation for elective colonoscopy: a meta-analysis and systematic review of randomized controlled trials. Surg Laparosc Endosc Percutan Tech. 2016; 26:102–116.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Successful Clipping of a Colonic Perforation during Diagnostic Colonoscopy
- Diagnosis and Management of Iatrogenic Endoscopic Retrograde Cholangiopancreatography Perforations Based on the European Society of Gastrointestinal Endoscopy Position Statement
- Perforation of a Meckel’s Diverticulum Following Ingestion of a Chicken Bone: A Case Report and Literature Review
- Iatrogenic Gallbladder Perforation during Gastric Endoscopic Mucosal Resection
- A Case of Successful Endoscopic Therapy in Delayed Diagnosed Perforation after Endoscopic Colon Polypectomy