Clin Endosc.
2022 Mar;55(2):270-278. 10.5946/ce.2021.083.
Peroral Pancreatoscopy with Videoscopy and Narrow-Band Imaging in Intraductal Papillary Mucinous Neoplasms with Dilatation of the Main Pancreatic Duct
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Toho University Omori Medical Center, Tokyo, Japan
- KMID: 2527572
- DOI: http://doi.org/10.5946/ce.2021.083
Abstract
- Background/Aims
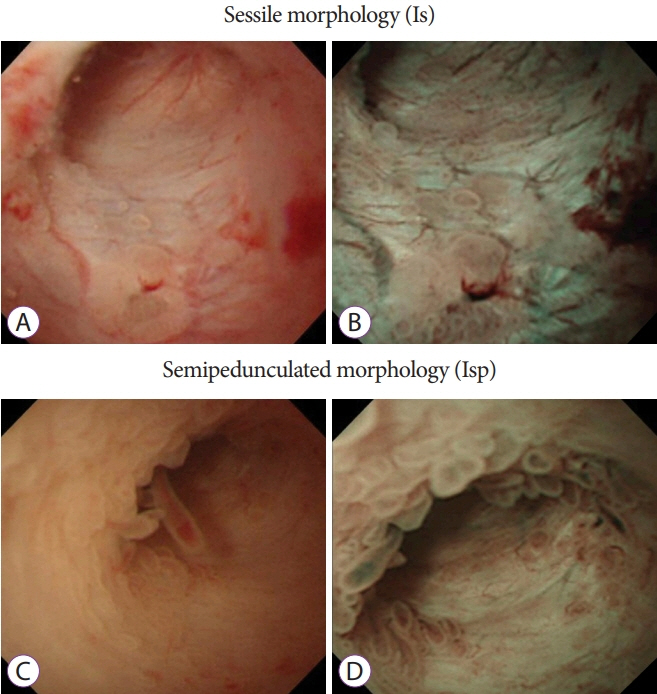
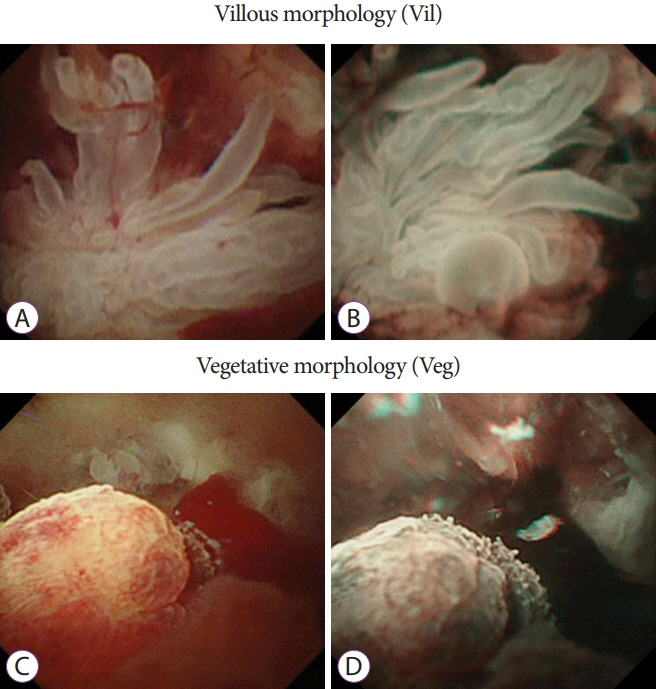
Endoscopic evaluation of intraductal papillary mucinous neoplasms (IPMNs) is useful in determining whether the lesions are benign or malignant. This study aimed to examine the usefulness of peroral pancreatoscopy (POPS) in determining the prognosis of IPMNs.
Methods
POPS with videoscopy was performed using the mother–baby scope technique. After surgery, computed tomography/magnetic resonance cholangiopancreatography or ultrasonography and blood tests were performed every 6 months during the follow-up.
Results
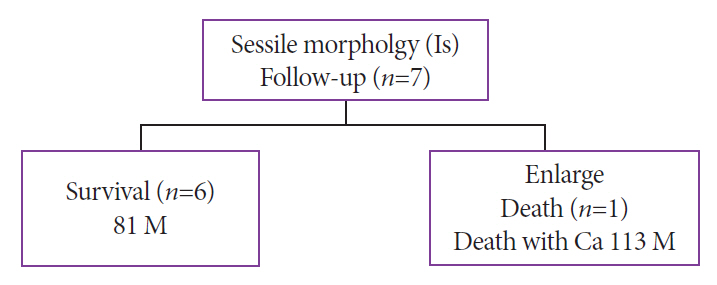
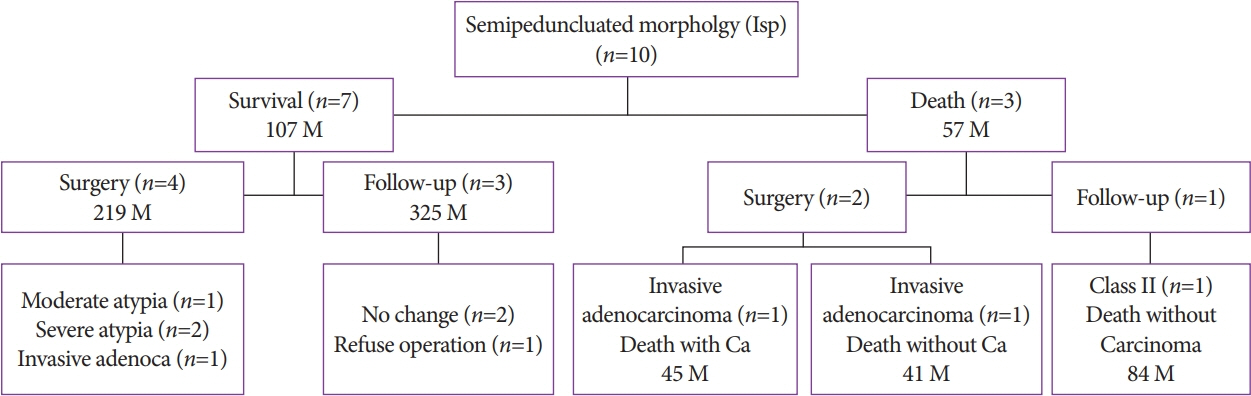
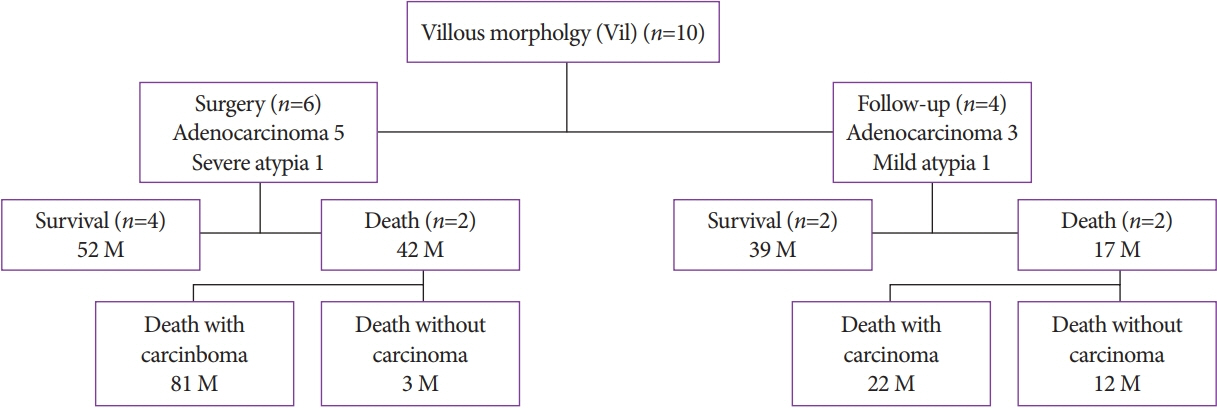
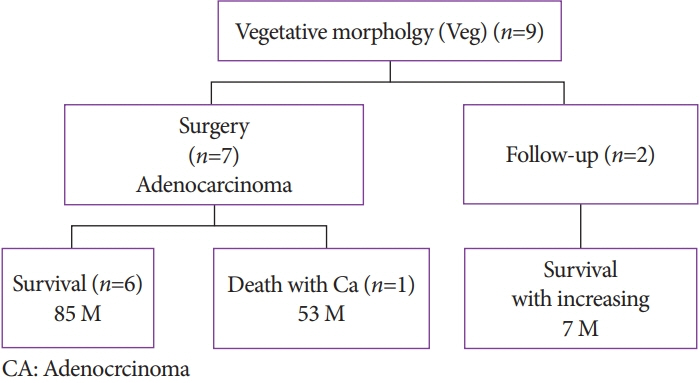
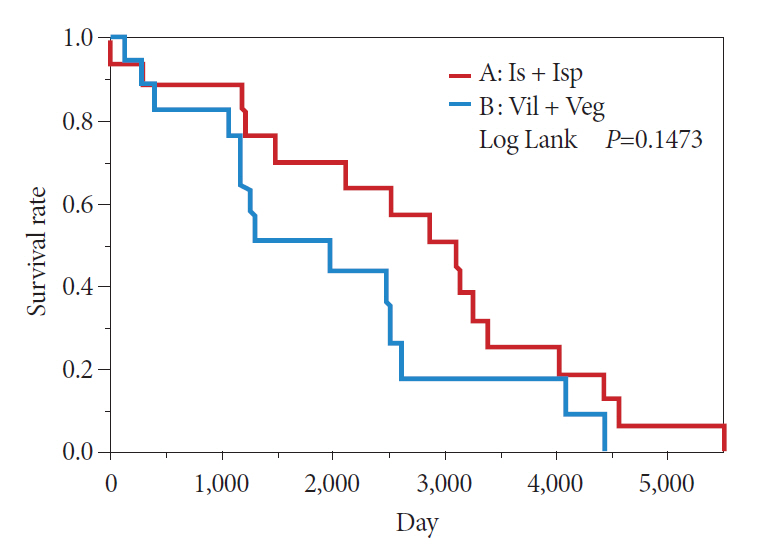
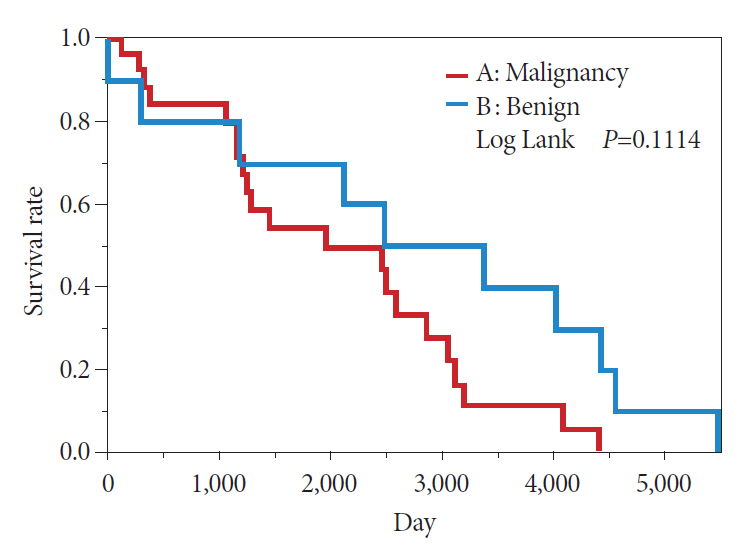
A total of 39 patients with main pancreatic duct (MPD)–type IPMNs underwent POPS using a videoscope, and the protrusions in the MPD were observed in 36 patients. The sensitivity and specificity of cytology/biopsy performed at the time of POPS were 85% and 87.5%, respectively. Of 19 patients who underwent surgery, 18 (95%) patients had negative surgical margins and 1 (5%) patient had a positive margin.
Conclusions
In IPMNs with dilatation of the MPD, POPS is considered effective if the lesions can be directly observed. The diagnosis of benign and malignant lesions is possible depending on the degree of lesion elevation. However, in some cases, slightly elevated lesions may increase in size during the follow-up or multiple lesions may be simultaneously present; therefore, careful follow-up is necessary.
Keyword
Figure
Reference
-
1. Tanaka M, Fernández-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12:183–197.2. Nagai K, Doi R, Kida A, et al. Intraductal papillary mucinous neoplasms of the pancreas: clinicopathologic characteristics and long-term follow-up after resection. World J Surg. 2008; 32:271–278. discussion 279-280.3. Hwang DW, Jang JY, Lee SE, Lim CS, Lee KU, Kim SW. Clinicopathologic analysis of surgically proven intraductal papillary mucinous neoplasms of the pancreas in SNUH: a 15-year experience at a single academic institution. Langenbecks Arch Surg. 2012; 397:93–102.4. Crippa S, Fernández-Del Castillo C, Salvia R, et al. Mucin-producing neoplasms of the pancreas: an analysis of distinguishing clinical and epidemiologic characteristics. Clin Gastroenterol Hepatol. 2010; 8:213–219.5. Schnelldorfer T, Sarr MG, Nagorney DM, et al. Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Arch Surg. 2008; 143:639–646. discussion 646.6. Nara S, Onaya H, Hiraoka N, et al. Preoperative evaluation of invasive and noninvasive intraductal papillary-mucinous neoplasms of the pancreas: clinical, radiological, and pathological analysis of 123 cases. Pancreas. 2009; 38:8–16.7. Fritz S, Klauss M, Bergmann F, et al. Pancreatic main-duct involvement in branch-duct IPMNs: an underestimated risk. Ann Surg. 2014; 260:848–855. discussion 855-856.8. Robles-Medranda C, Valero M, Soria-Alcivar M, et al. Reliability and accuracy of a novel classification system using peroral cholangioscopy for the diagnosis of bile duct lesions. Endoscopy. 2018; 50:1059–1070.9. Tajiri H. Diagnostic evaluation of pancreatic carcinoma and chronic pancreatitis by pancreatoscopy. Diagn Ther Endosc. 1997; 3:177–182.10. Sugiyama M, Atomi Y, Saito M. Intraductal papillary tumors of the pancreas: evaluation with endoscopic ultrasonography. Gastrointest Endosc. 1998; 48:164–171.11. Igarashi Y, Ukita T, Inoue H, et al. Clinical evaluation of the peroral cholangioscopy using a new videoscope. Diagn Ther Endosc. 1999; 5:231–237.12. Kodama T, Sato H, Horii Y, et al. Pancreatoscopy for the next generation: development of the peroral electronic pancreatoscope system. Gastrointest Endosc. 1999; 49:366–371.13. Kobayashi M. A study for the improvement of diagnostic ability of ultra-thin pancreatoscope: comparison of histological findings and application of image processing. Gastroenterological Endoscopy. 1996; 38:2147–2159.14. Uehara H, Nakaizumi A, Tatsuta M, et al. Diagnosis of carcinoma in situ of the pancreas by peroral pancreatoscopy and pancreatoscopic cytology. Cancer. 1997; 79:454–461.15. Tajiri H, Kobayashi M, Ohtsu A, Ryu M, Yoshida S. Peroral pancreatoscopy for the diagnosis of pancreatic diseases. Pancreas. 1998; 16:408–412.16. Jung M, Zipf A, Schoonbroodt D, Herrmann G, Caspary WF. Is pancreatoscopy of any benefit in clarifying the diagnosis of pancreatic duct lesions? Endoscopy. 1998; 30:273–280.17. Kodama T, Koshitani T, Sato H, et al. Electronic pancreatoscopy for the diagnosis of pancreatic diseases. Am J Gastroenterol. 2002; 97:617–622.18. Adler DG. Pancreatoscopy for pancreatic duct stones. Gastrointest Endosc. 2014; 79:208.19. Yasuda K, Sakata M, Ueda M, Uno K, Nakajima M. The use of pancreatoscopy in the diagnosis of intraductal papillary mucinous tumor lesions of the pancreas. Clin Gastroenterol Hepatol. 2005; 3:S53–S57.20. Igarashi Y, Okano N, Satou D, Miura T, Miki K. Peroral cholangioscopy using a new thinner videoscope (chf-B260). Dig Endosc. 2005; 17:S63–S66.21. Muto M, Sano Y, Fujii S, Ochiai A, Yoshida S. Endoscopic diagnosis of intraepithelial squamous neoplasia in head and neck and esophageal mucosal sites. Dig Endosc. 2006; 18:S2–S5.22. Kodama T, Imamura Y, Sato H, et al. Feasibility study using a new small electronic pancreatoscope: description of findings in chronic pancreatitis. Endoscopy. 2003; 35:305–310.23. Ringold DA, Shah RJ. Peroral pancreatoscopy in the diagnosis and management of intraductal papillary mucinous neoplasia and indeterminate pancreatic duct pathology. Gastrointest Endosc Clin N Am. 2009; 19:601–613.24. Parbhu SK, Siddiqui AA, Murphy M, et al. Efficacy, safety, and outcomes of endoscopic retrograde cholangiopancreatography with peroral pancreatoscopy: a multicenter experience. J Clin Gastroenterol. 2017; 51:e101–e105.25. Yamao K, Ohashi K, Nakamura T, et al. Evaluation of various imaging methods in the differential diagnosis of intraductal papillary-mucinous tumor (IPMT) of the pancreas. Hepatogastroenterology. 2001; 48:962–966.26. Yamaguchi T, Hara T, Tsuyuguchi T, et al. Peroral pancreatoscopy in the diagnosis of mucin-producing tumors of the pancreas. Gastrointest Endosc. 2000; 52:67–73.27. Mukai H, Yasuda K, Nakajima M. Differential diagnosis of mucin-producing tumors of the pancreas by intraductal ultrasonography and peroral pancreatoscopy. Endoscopy. 1998; 30:A99–A102.28. Hara T, Yamaguchi T, Ishihara T, et al. Diagnosis and patient management of intraductal papillary-mucinous tumor of the pancreas by using peroral pancreatoscopy and intraductal ultrasonography. Gastroenterology. 2002; 122:34–43.29. Miura T, Igarashi Y, Okano N, Miki K, Okubo Y. Endoscopic diagnosis of intraductal papillary-mucinous neoplasm of the pancreas by means of peroral pancreatoscopy using a small-diameter videoscope and narrow-band imaging. Dig Endosc. 2010; 22:119–123.30. El Hajj II, Brauer BC, Wani S, Fukami N, Attwell AR, Shah RJ. Role of per-oral pancreatoscopy in the evaluation of suspected pancreatic duct neoplasia: a 13-year U.S. single-center experience. Gastrointest Endosc. 2017; 85:737–745.31. Lafemina J, Katabi N, Klimstra D, et al. Malignant progression in IPMN: a cohort analysis of patients initially selected for resection or observation. Ann Surg Oncol. 2013; 20:440–447.32. Brugge WR, Lewandrowski K, Lee-Lewandrowski E, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004; 126:1330–1336.33. Uehara H, Nakaizumi A, Ishikawa O, et al. Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut. 2008; 57:1561–1565.34. Tanno S, Nakano Y, Koizumi K, et al. Pancreatic ductal adenocarcinomas in long-term follow-up patients with branch duct intraductal papillary mucinous neoplasms. Pancreas. 2010; 39:36–40.35. Kamata K, Kitano M, Kudo M, et al. Value of EUS in early detection of pancreatic ductal adenocarcinomas in patients with intraductal papillary mucinous neoplasms. Endoscopy. 2014; 46:22–29.36. Date K, Ohtsuka T, Nakamura S, et al. Surveillance of patients with intraductal papillary mucinous neoplasm with and without pancreatectomy with special reference to the incidence of concomitant pancreatic ductal adenocarcinoma. Surgery. 2018; 163:291–299.37. Tanaka M, Fernández-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17:738–753.38. Igarashi Y, Tada T, Shimura J, et al. Endosonographic diagnosis of intraductal papillary-mucinous pancreatic tumors by intraductal ultrasonography. Dig Endosc. 2003; 15:196–199.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peroral pancreatoscopy with videoscopy and narrow-band imaging in intraductal papillary mucinous neoplasms with dilatation of the main pancreatic duct
- Visible Intraductal Papillary Mucinous Neoplasm after Drinking Water
- Predicting Malignancy by Peroral Pancreatoscopy of an Intraductal Papillary Mucinous Neoplasm with a Dilated Main Pancreatic Duct: Is Seeing Enough?
- Comparison of Mucinous Cystic Tumor and Intraductal Papillary Mucinous Tumor
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report