Clin Endosc.
2022 Mar;55(2):240-247. 10.5946/ce.2021.115.
Risk Stratification in Cancer Patients with Acute Upper Gastrointestinal Bleeding: Comparison of Glasgow-Blatchford, Rockall and AIMS65, and Development of a New Scoring System
- Affiliations
-
- 1Hospital Sírio-Libanês, Brasília, Distrito Federal, Brazil
- 2Department of Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, Ohio, USA
- 3Endoscopy Unit, Cancer Institute of the University of São Paulo, São Paulo, Brazil
- 4Western University, London, ON, Canada
- 5Division of Gastroenterology, McGill University and the McGill University Health Centre, Montreal, QC, Canada
- KMID: 2527568
- DOI: http://doi.org/10.5946/ce.2021.115
Abstract
- Background/Aims
Few studies have measured the accuracy of prognostic scores for upper gastrointestinal bleeding (UGIB) among cancer patients. Thereby, we compared the prognostic scores for predicting major outcomes in cancer patients with UGIB. Secondarily, we developed a new model to detect patients who might require hemostatic care.
Methods
A prospective research was performed in a tertiary hospital by enrolling cancer patients admitted with UGIB. Clinical and endoscopic findings were obtained through a prospective database. Multiple logistic regression analysis was performed to gauge the power of each score.
Results
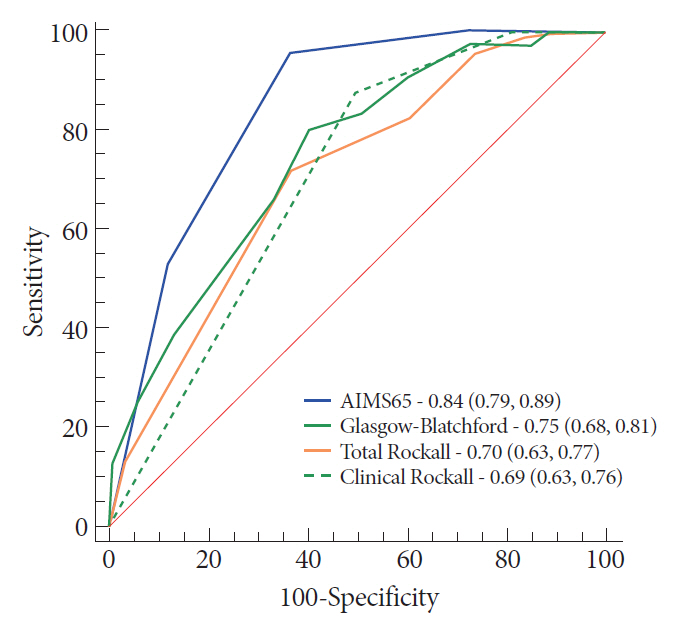
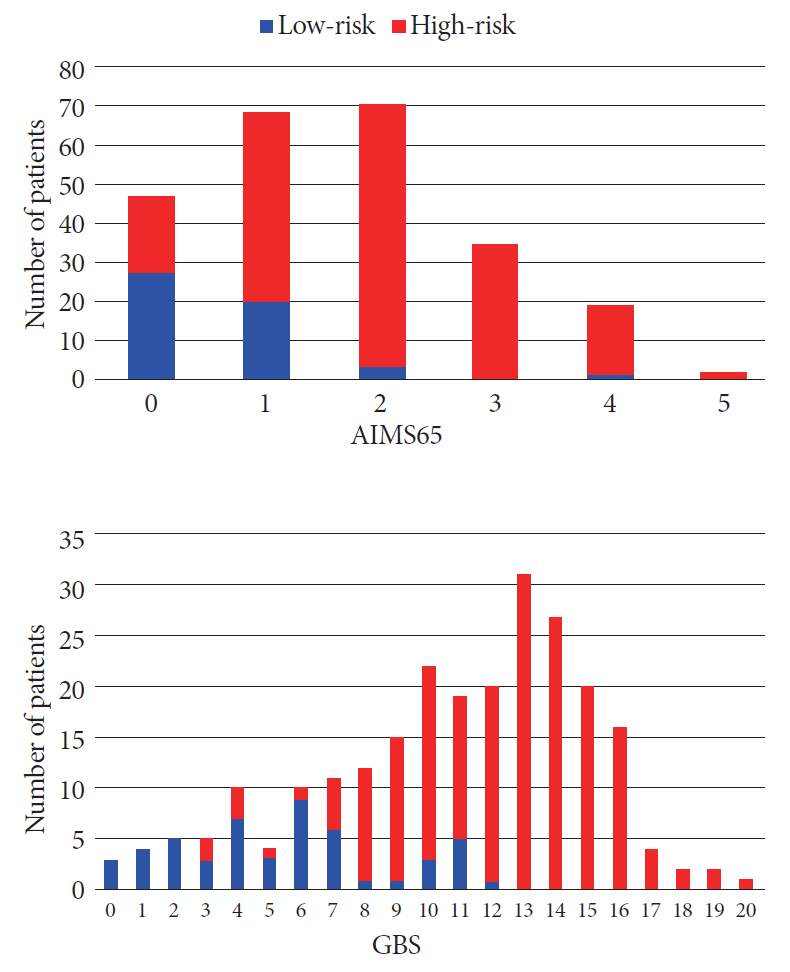
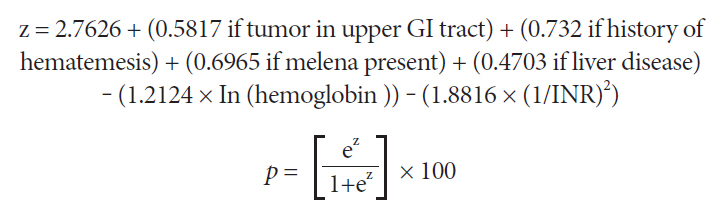
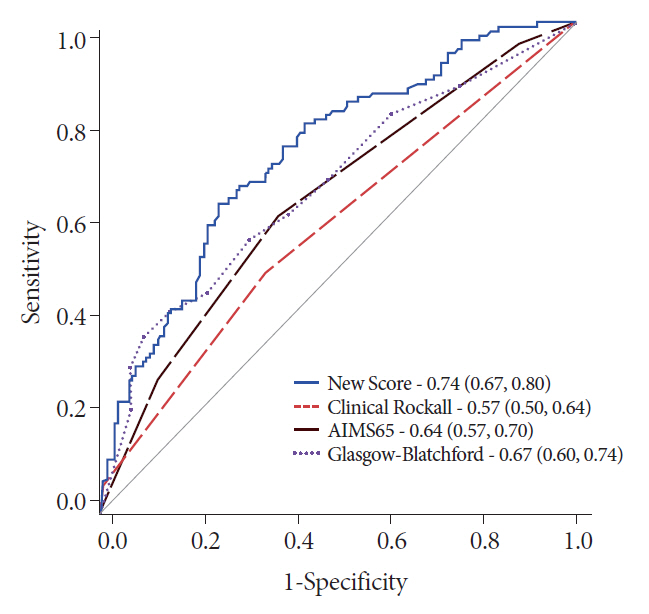
From April 2015 to May 2016, 243 patients met the inclusion criteria. The AIMS65 (area under the curve [AUC] 0.85) best predicted intensive care unit admission, while the Glasgow-Blatchford score best predicted blood transfusion (AUC 0.82) and the low-risk group (AUC 0.92). All scores failed to predict hemostatic therapy and rebleeding. The new score was superior (AUC 0.74) in predicting hemostatic therapy. The AIMS65 (AUC 0.84) best predicted in-hospital mortality.
Conclusions
The scoring systems for prognostication were validated in the group of cancer patients with UGIB. A new score was developed to predict hemostatic therapy. Following this result, future prospective research should be performed to validate the new score.
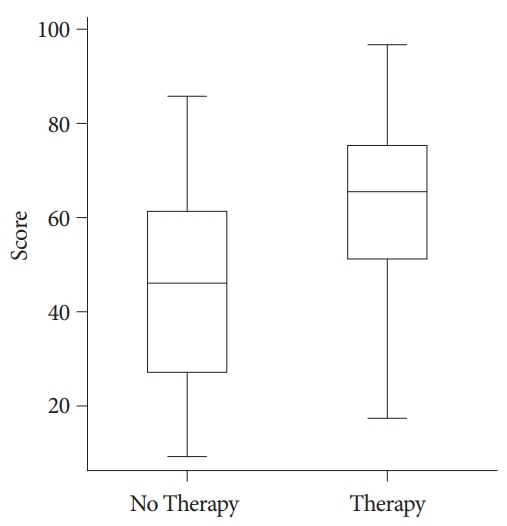
Figure
Reference
-
1. Maluf-Filho F, Martins BC, de Lima MS, et al. Etiology, endoscopic management and mortality of upper gastrointestinal bleeding in patients with cancer. United European Gastroenterol J. 2013; 1:60–67.2. Targownik LE, Nabalamba A. Trends in management and outcomes of acute nonvariceal upper gastrointestinal bleeding: 1993-2003. Clin Gastroenterol Hepatol. 2006; 4:1459–1466.3. Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010; 362:823–832.4. Franco MC, Nakao FS, Rodrigues R, Maluf-Filho F, Paulo GA de, Libera ED. Proposal of a clinical care pathway for the management of acute upper gastrointestinal bleeding. Arq Gastroenterol. 2015; 52:283–292.5. Barkun AN, Almadi M, Kuipers EJ, et al. Management of nonvariceal upper gastrointestinal bleeding: guideline recommendations from the International Consensus Group. Ann Intern Med. 2019; 171:805–822.6. Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996; 38:316–321.7. Vreeburg EM, Terwee CB, Snel P, et al. Validation of the Rockall risk scoring system in upper gastrointestinal bleeding. Gut. 1999; 44:331–335.8. Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000; 356:1318–1321.9. Saltzman JR, Tabak YP, Hyett BH, Sun X, Travis AC, Johannes RS. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. Gastrointest Endosc. 2011; 74:1215–1224.10. Hyett BH, Abougergi MS, Charpentier JP, et al. The AIMS65 score compared with the Glasgow-Blatchford score in predicting outcomes in upper GI bleeding. Gastrointest Endosc. 2013; 77:551–557.11. Martins BC, Wodak S, Gusmon CC, et al. Argon plasma coagulation for the endoscopic treatment of gastrointestinal tumor bleeding: a retrospective comparison with a non-treated historical cohort. United European Gastroenterol J. 2016; 4:49–54.12. Kim YI, Choi IJ, Lee JY, Kim CG, Kim HK, Park YL. Comparison of the performance of risk scoring systems for tumor bleeding in patients with inoperable gastric cancer. Endoscopy. 2020; 52:359–367.13. Ahn S, Lim KS, Lee YS, Lee JL. Blatchford score is a useful tool for predicting the need for intervention in cancer patients with upper gastrointestinal bleeding. J Gastroenterol Hepatol. 2013; 28:1288–1294.14. Laine L, Spiegel B, Rostom A, et al. Methodology for randomized trials of patients with nonvariceal upper gastrointestinal bleeding: recommendations from an international consensus conference. Am J Gastroenterol. 2010; 105:540–550.15. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.16. Youden WJ. Index for rating diagnostic tests. Cancer. 1950; 3:32–35.17. Robertson M, Majumdar A, Boyapati R, et al. Risk stratification in acute upper GI bleeding: comparison of the AIMS65 score with the Glasgow-Blatchford and Rockall scoring systems. Gastrointest Endosc. 2016; 83:1151–1160.18. Martínez-Cara JG, Jiménez-Rosales R, Úbeda-Muñoz M, de Hierro ML, de Teresa J, Redondo-Cerezo E. Comparison of AIMS65, Glasgow-Blatchford score, and Rockall score in a European series of patients with upper gastrointestinal bleeding: performance when predicting in-hospital and delayed mortality. United European Gastroenterol J. 2016; 4:371–379.19. Hwang JH, Fisher DA, Ben-Menachem T, et al. The role of endoscopy in the management of acute non-variceal upper GI bleeding. Gastrointest Endosc. 2012; 75:1132–1138.20. Chen YI, Barkun AN, Soulellis C, Mayrand S, Ghali P. Use of the endoscopically applied hemostatic powder TC-325 in cancer-related upper GI hemorrhage: preliminary experience (with video). Gastrointest Endosc. 2012; 75:1278–1281.21. Shin J, Cha B, Park JS, et al. Efficacy of a novel hemostatic adhesive powder in patients with upper gastrointestinal tumor bleeding. BMC Gastroenterol. 2021; 21:40.22. Stanley AJ, Laine L, Dalton HR, et al. Comparison of risk scoring systems for patients presenting with upper gastrointestinal bleeding: international multicentre prospective study. BMJ. 2017; 356:i6432.23. Abougergi MS, Charpentier JP, Bethea E, et al. A prospective, multicenter study of the AIMS65 score compared with the Glasgow-Blatchford score in predicting upper gastrointestinal hemorrhage outcomes. J Clin Gastroenterol. 2016; 50:464–469.24. van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008; 22:209–224.25. Maluf-Filho F. Predicting clinical outcomes in patients with bleeding from gastric cancer: novel tools are needed to nail it! Endoscopy. 2020; 52:332–333.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prospective Comparison of the AIMS65 Score, Glasgow-Blatchford Score, and Rockall Score for Predicting Clinical Outcomes in Patients with Variceal and Nonvariceal Upper Gastrointestinal Bleeding
- Comparison of AIMS65 Score and Other Scoring Systems for Predicting Clinical Outcomes in Koreans with Nonvariceal Upper Gastrointestinal Bleeding
- Validation of the Glasgow-Blatchford score and the Pre-endoscopic Rockall Score for Predicting Active Gastrointestinal Bleeding in Emergency Department Patients with Suspected Upper Gastrointestinal Bleeding
- Risk Stratification for Patients with Upper Gastrointestinal Bleeding
- Mortality Risk Scoring System in Patients after Bleeding from Cancers in the Upper Gastrointestinal Tract