Ann Rehabil Med.
2022 Feb;46(1):9-23. 10.5535/arm.21170.
Reference Standards for Nerve Conduction Studies of Individual Nerves of Lower Extremity With Expanded Uncertainty in Healthy Korean Adults
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul, Korea
- 2Data Center for Korean Reference Nerve Conductions, Seoul National University Hospital, Seoul, Korea
- 3Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 4National Center for Standard Reference Data, Daejeon, Korea
- 5Korea Research Institute of Standards and Science, Daejeon, Korea
- 6Department of Rehabilitation Medicine, Kosin University Gospel Hospital, Busan, Korea
- 7Department of Rehabilitation Medicine, National Traffic Injury Rehabilitation Hospital, Yangpyeong, Korea
- 8Department of Rehabilitation Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 9Department of Rehabilitation Medicine, Seoul National University Boramae Medical Center, Seoul, Korea
- 10Institute on Aging, Seoul National University, Seoul, Korea
- KMID: 2527095
- DOI: http://doi.org/10.5535/arm.21170
Abstract
Objective
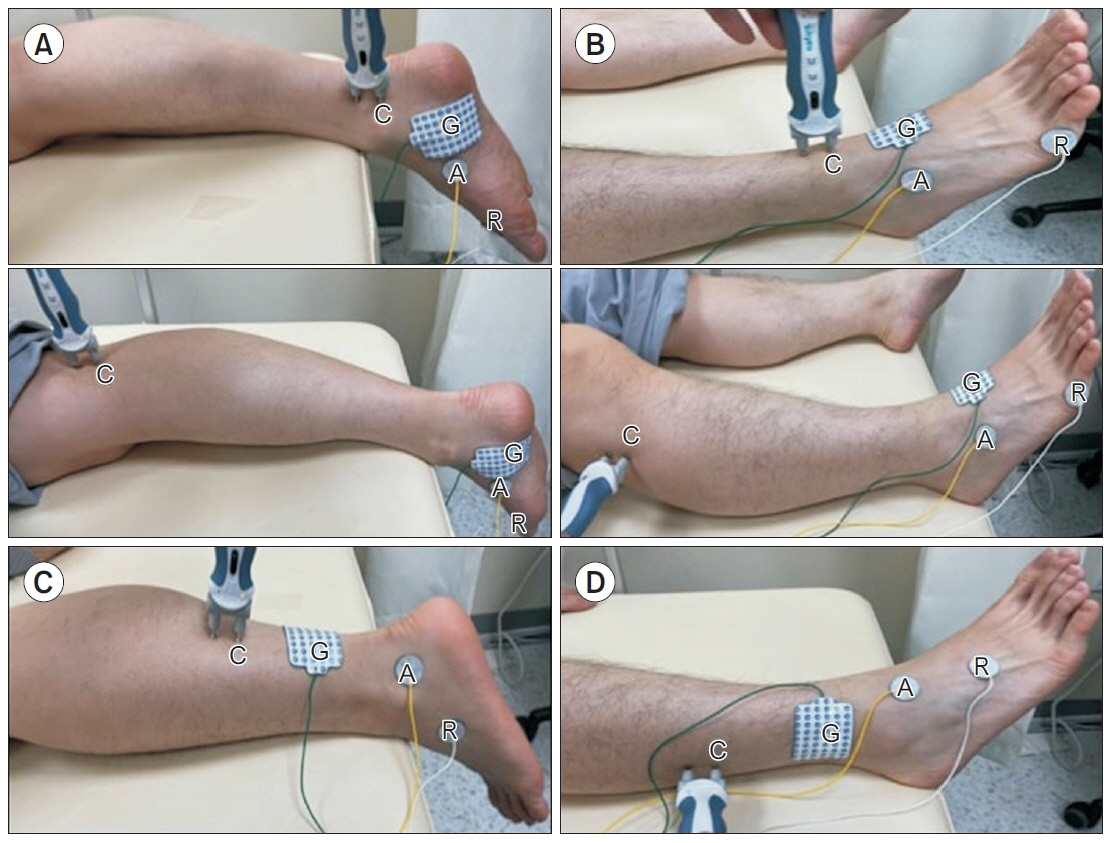
To develop a set of reference standards for tibial motor, common peroneal motor, sural sensory, and superficial peroneal sensory nerve conduction studies (NCSs) with expanded uncertainty in a healthy Korean population.
Methods
Standardized procedures were conducted for individual lower extremity NCSs of 199 healthy participants in their 20s (n=100) and 50s (n=99). Mean values and expanded uncertainties for parameters were analyzed with thorough consideration of multiple uncertainty factors under the International Guide to the Expression of Uncertainty in Measurement. In addition, side-to-side differences in onset latency, amplitude, and nerve conduction velocity (NCV) were analyzed.
Results
Mean (reference range) for distal onset latency, baseline to negative peak amplitude, NCV of tibial motor nerve in males in their 20s were 4.3 ms (3.1–5.4 ms), 7.1 mV (3.4–10.9 mV), and 50.7 m/s (42.2–59.3 m/s), respectively; sural sensory nerve baseline to negative peak amplitude in males in their 20s was 21.7 μV (8.3–35.2 μV). Including the aforementioned data, we present a vast dataset of normative mean values and expanded uncertainties for NCSs of the leg in a healthy Korean population. Furthermore, upper limits for normal side-to-side differences for onset latency, amplitude, and NCV of each nerve are suggested.
Conclusion
To our knowledge, this is the first study to present the reference standards of leg NCSs with consideration for multifactorial uncertainties in an Asian population. We expect these results to help practitioners make reliable and reproducible clinical decisions.
Figure
Cited by 2 articles
-
Refined Diagnostic Protocol for Diabetic Polyneuropathy: Paving the Way for Timely Detection
Byung-Mo Oh
Ann Rehabil Med. 2023;47(4):234-236. doi: 10.5535/arm.23122.Reference Standard of Median Nerve Conduction Study in Korea
Jae Hyun Lee, Eunkyung Kim, Hyung-Seok Shim, Min-Gu Kang, Keewon Kim, Sang Yoon Lee, Goo Joo Lee, Shi-Uk Lee, Jae-Young Lim, Sun Gun Chung, Byung-Mo Oh
Ann Rehabil Med. 2024;48(4):259-270. doi: 10.5535/arm.240015.
Reference
-
1. Kimura J. Principles and pitfalls of nerve conduction studies. Ann Neurol. 1984; 16:415–29.
Article2. Stetson DS, Albers JW, Silverstein BA, Wolfe RA. Effects of age, sex, and anthropometric factors on nerve conduction measures. Muscle Nerve. 1992; 15:1095–104.
Article3. Bolton CF, Sawa GM, Carter K. The effects of temperature on human compound action potentials. J Neurol Neurosurg Psychiatry. 1981; 44:407–13.
Article4. Halar EM, DeLisa JA, Soine TL. Nerve conduction studies in upper extremities: skin temperature corrections. Arch Phys Med Rehabil. 1983; 64:412–6.5. Buschbacher RM. Reference values for peroneal nerve motor conduction to the tibialis anterior and for peroneal vs. tibial latencies. Am J Phys Med Rehabil. 2003; 82:296–301.
Article6. Buschbacher RM. Peroneal nerve motor conduction to the extensor digitorum brevis. Am J Phys Med Rehabil. 1999; 78(6 Suppl):S26–31.7. Chen S, Andary M, Buschbacher R, Del Toro D, Smith B, So Y, et al. Electrodiagnostic reference values for upper and lower limb nerve conduction studies in adult populations. Muscle Nerve. 2016; 54:371–7.
Article8. Dillingham T, Chen S, Andary M, Buschbacher R, Del Toro D, Smith B, et al. Establishing high-quality reference values for nerve conduction studies: a report from the normative data task force of the American Association of Neuromuscular & Electrodiagnostic Medicine. Muscle Nerve. 2016; 54:366–70.
Article9. Buschbacher RM. Sural and saphenous 14-cm antidromic sensory nerve conduction studies. Am J Phys Med Rehabil. 2003; 82:421–6.
Article10. Buschbacher RM. Tibial nerve motor conduction to the abductor hallucis. Am J Phys Med Rehabil. 1999; 78(6 Suppl):S15–20.11. Joint Committee for Guides in Metrology. Evaluation of measurement data - Guide to the expression of uncertainty in measurement. Geneva, Switzerland: International Organization for Standardization;2008. JCGM 100:2008.12. National Health Insurance Service. Korean blood glucose national reference standard. Wonju, Korea: National Health Insurance Service;2019. [cited 2022 Jan 11]. Available from: https://nhiss.nhis.or.kr/bd/ab/bdabf011cv.do.13. Madani S, Doughty C. L ower extremity entrapment neuropathies. Best Pract Res Clin Rheumatol. 2020; 34:101565.14. Chang AS, Dillingham TR, Yu KF. Statistical methods of computing reference values for side-to-side differences in nerve conduction studies. Am J Phys Med Rehabil. 1996; 75:437–42.15. Campbell WW, Robinson LR. Deriving reference values in electrodiagnostic medicine. Muscle Nerve. 1993; 16:424–8.
Article16. Arnold N, Harriman DG. The incidence of abnormality in control human peripheral nerves studied by single axon dissection. J Neurol Neurosurg Psychiatry. 1970; 33:55–61.
Article17. Lascelles RG, Thomas PK. Changes due to age in internodal length in the sural nerve in man. J Neurol Neurosurg Psychiatry. 1966; 29:40–4.
Article18. Vizoso AD, Young JZ. Internode length and fibre diameter in developing and regenerating nerves. J Anat. 1948; 82(Pt 1-2):110–34.19. Bolton CF, Carter KM. Human sensory nerve compound action potential amplitude: variation with sex and finger circumference. J Neurol Neurosurg Psychiatry. 1980; 43:925–8.
Article20. Cummins KL, Dorfman LJ. Nerve fiber conduction velocity distributions: studies of normal and diabetic human nerves. Ann Neurol. 1981; 9:67–74.
Article21. Robinson LR, Rubner DE, Wahl PW, Fujimoto WY, Stolov WC. Influences of height and gender on normal nerve conduction studies. Arch Phys Med Rehabil. 1993; 74:1134–8.22. Buschbacher RM. Body mass index effect on common nerve conduction study measurements. Muscle Nerve. 1998; 21:1398–404.
Article23. Parker V, Warman Chardon J, Mills J, Goldsmith C, Bourque PR. Supramaximal stimulus intensity as a diagnostic tool in chronic demyelinating neuropathy. Neurosci J. 2016; 2016:6796270.
Article24. Barkhaus PE, Kincaid JC, Nandedkar SD. Tibial motor nerve conduction studies: an investigation into the mechanism for amplitude drop of the proximal evoked response. Muscle Nerve. 2011; 44:776–82.
Article25. Oh SJ, Kim DE, Kuruoglu HR. What is the best diagnostic index of conduction block and temporal dispersion? Muscle Nerve. 1994; 17:489–93.
Article26. Taylor PK. CMAP dispersion, amplitude decay, and area decay in a normal population. Muscle Nerve. 1993; 16:1181–7.
Article27. Weber F. Conduction block and abnormal temporal dispersion: diagnostic criteria. Electromyogr Clin Neurophysiol. 1997; 37:305–9.28. Kamel JT, Knight-Sadler RJ, Roberts LJ. Fibular motor nerve conduction studies: Investigating the mechanism for compound muscle action potential amplitude drop with proximal stimulation. Muscle Nerve. 2015; 52:993–6.
Article29. Olney RK. Guidelines in electrodiagnostic medicine. Consensus criteria for the diagnosis of partial conduction block. Muscle Nerve Suppl. 1999; 8:S225–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ulnar Nerve Conduction Studies: Reference Standards with Extended Uncertainty in Healthy South Korean Adults
- Reference Standard of Median Nerve Conduction Study in Korea
- Effects of Age, Sex and Height on Nerve Conduction Studies
- A Study of Nerve Conduction Velocity of Normal Adults
- No Response Rates of Sensory Nerve Conduction Studies and Late Responses in Lower Limbs of Heathy Adults