Korean Circ J.
2022 Mar;52(3):205-217. 10.4070/kcj.2021.0188.
Prognostic Impact of Left Atrial Strain After Mitral Valve Repair Surgery in Patients With Severe Mitral Regurgitation
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chungnam National University Sejong Hospital, Chungnam National University College of Medicine, Sejong, Korea
- 2Department of Cardiology in Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea
- 3Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Division of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2526954
- DOI: http://doi.org/10.4070/kcj.2021.0188
Abstract
- Background and Objectives
The prognostic value of left atrial (LA) function in terms of long-term clinical outcomes after mitral regurgitation (MR) surgery remains unclear. Therefore, we investigated the impact of preoperative LA global longitudinal strain (LAGLS) on the long-term postoperative clinical outcomes in chronic severe MR patients who underwent mitral valve (MV) repair surgery.
Methods
From January 2012 to December 2017, we analyzed 338 patients (mean age, 51.9±12.5 years; 218 males [64.5%]) treated with MV repair surgery for severe MR. The primary outcome was cardiovascular events, defined as the composite of all-cause death, newly developed atrial fibrillation (AF), and re-hospitalization for cardiovascular causes.
Results
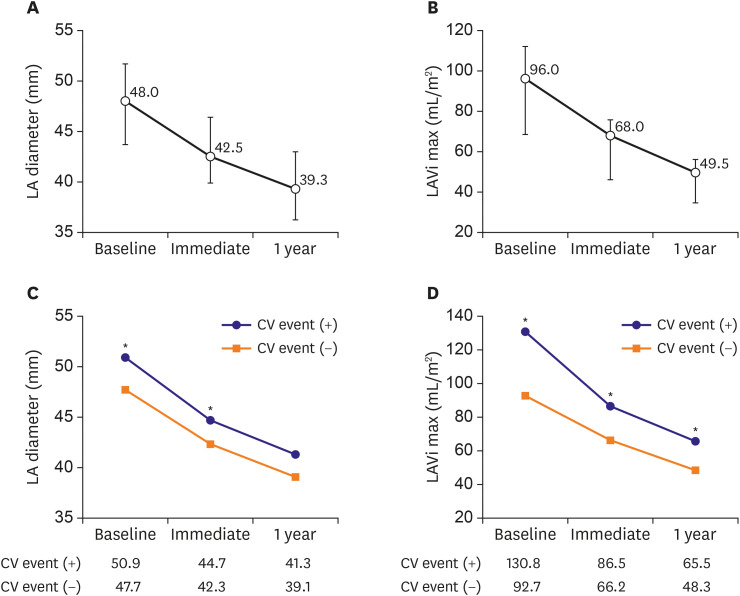
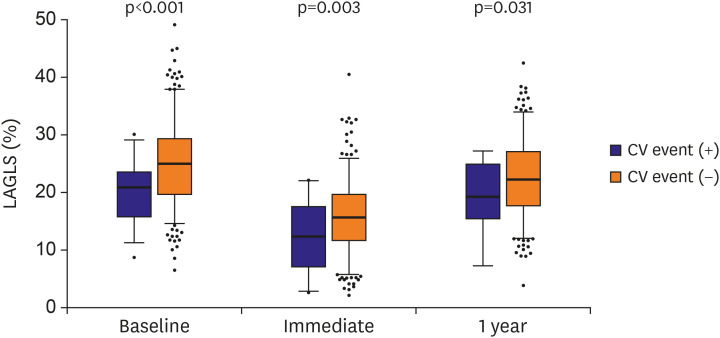
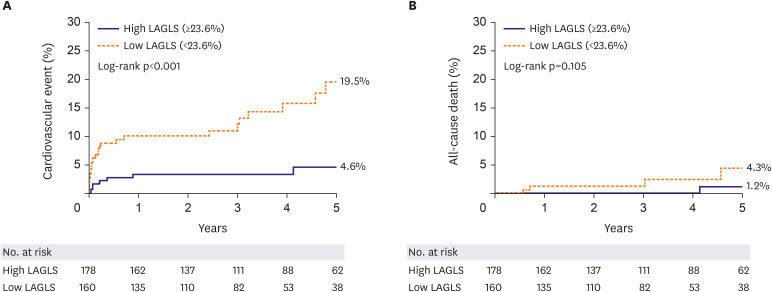
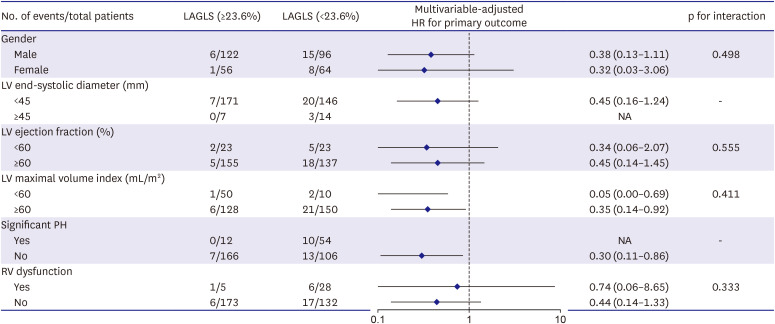
During a median follow-up of 45 months (interquartile range, 26–65), 30 (8.9%) cardiovascular events, 5 (1.5%) all-cause death, 8 (2.4%) newly developed AF, and 26 (7.7%) re-hospitalizations occurred. On multivariable analysis, baseline LAGLS was an independent predictor of cardiovascular events (adjusted hazard ratio [HR], 0.91; 95% confidential interval [CI], 0.85–0.97; p=0.004) and re-hospitalization (adjusted HR, 0.93; 95% CI,0.86–1.00; p=0.037). According to the optimal cutoff value of LAGLS, patients with low LAGLS (<23.6%) had a significantly higher risk of cardiovascular events (adjusted HR, 2.70; 95% CI, 1.04–7.00; p=0.041) than those with high LAGLS (≥23.6%). In a subgroup analysis, patients with high LAGLS had better clinical outcomes regardless of whether the patient had a LA volume index <60 mL/m2 .
Conclusions
In patients with chronic severe MR who received successful MV repair surgery, preoperative LAGLS is an independent predictor of long-term postoperative outcomes.
Figure
Cited by 2 articles
-
Expanding Role of Left Atrial Strain in Valvular Heart Disease
Jah Yeon Choi
Korean Circ J. 2022;52(3):218-219. doi: 10.4070/kcj.2022.0004.Current Unmet Needs and Clues to the Solution in the Management of Tricuspid Regurgitation
Byung Joo Sun, Jae-Hyeong Park
Korean Circ J. 2022;52(6):414-428. doi: 10.4070/kcj.2022.0117.
Reference
-
1. Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018; 137:e67–492. PMID: 29386200.2. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006; 368:1005–1011. PMID: 16980116.
Article3. Falk V, Baumgartner H, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg. 2017; 52:616–664. PMID: 29156023.4. Cameli M, Lisi M, Giacomin E, et al. Chronic mitral regurgitation: left atrial deformation analysis by two-dimensional speckle tracking echocardiography. Echocardiography. 2011; 28:327–334. PMID: 21323986.
Article5. Borg AN, Pearce KA, Williams SG, Ray SG. Left atrial function and deformation in chronic primary mitral regurgitation. Eur J Echocardiogr. 2009; 10:833–840. PMID: 19531539.
Article6. Benjamin EJ, D’Agostino RB, Belanger AJ, Wolf PA, Levy D. Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation. 1995; 92:835–841. PMID: 7641364.7. Toprak C, Kahveci G, Kilicgedik A, et al. Left atrial remodeling in patients undergoing percutaneous mitral valve repair with the MitraClip system: an advanced echocardiography study. Echocardiography. 2016; 33:1504–1511. PMID: 27350336.
Article8. Cameli M, Lisi M, Righini FM, et al. Usefulness of atrial deformation analysis to predict left atrial fibrosis and endocardial thickness in patients undergoing mitral valve operations for severe mitral regurgitation secondary to mitral valve prolapse. Am J Cardiol. 2013; 111:595–601. PMID: 23211360.
Article9. Melenovsky V, Hwang SJ, Redfield MM, Zakeri R, Lin G, Borlaug BA. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail. 2015; 8:295–303. PMID: 25593126.
Article10. Park JH, Hwang IC, Park JJ, Park JB, Cho GY. Prognostic power of left atrial strain in patients with acute heart failure. Eur Heart J Cardiovasc Imaging. 2021; 22:210–219. PMID: 32031588.
Article11. Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017; 30:303–371. PMID: 28314623.
Article12. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270. PMID: 25712077.
Article13. Vianna-Pinton R, Moreno CA, Baxter CM, Lee KS, Tsang TS, Appleton CP. Two-dimensional speckle-tracking echocardiography of the left atrium: feasibility and regional contraction and relaxation differences in normal subjects. J Am Soc Echocardiogr. 2009; 22:299–305. PMID: 19258177.
Article14. Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016; 29:277–314. PMID: 27037982.
Article15. Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997; 30:1527–1533. PMID: 9362412.
Article16. Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984; 70:657–662. PMID: 6478568.
Article17. Brennan JM, Blair JE, Goonewardena S, et al. Reappraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr. 2007; 20:857–861. PMID: 17617312.
Article18. Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018; 19:591–600. PMID: 29596561.
Article19. Mor-Avi V, Lang RM, Badano LP, et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr. 2011; 24:277–313. PMID: 21338865.
Article20. Pathan F, D’Elia N, Nolan MT, Marwick TH, Negishi K. Normal ranges of left atrial strain by speckle-tracking echocardiography: a systematic review and meta-analysis. J Am Soc Echocardiogr. 2017; 30:59–70.e8. PMID: 28341032.
Article21. Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993; 88:107–115. PMID: 8319323.
Article22. Pritchett AM, Jacobsen SJ, Mahoney DW, Rodeheffer RJ, Bailey KR, Redfield MM. Left atrial volume as an index of left atrial size: a population-based study. J Am Coll Cardiol. 2003; 41:1036–1043. PMID: 12651054.
Article23. Park JH, Kim KH, Rink L, et al. Left atrial enlargement and its association with left atrial strain in university athletes participated in 2015 Gwangju Summer Universiade. Eur Heart J Cardiovasc Imaging. 2020; 21:865–872. PMID: 32380526.
Article24. Facchini E, Degiovanni A, Marino PN. Left atrium function in patients with coronary artery disease. Curr Opin Cardiol. 2014; 29:423–429. PMID: 24945488.
Article25. Appleton CP, Kovács SJ. The role of left atrial function in diastolic heart failure. Circ Cardiovasc Imaging. 2009; 2:6–9. PMID: 19808558.
Article26. Park JH. Two-dimensional echocardiographic assessment of myocardial strain: important echocardiographic parameter readily useful in clinical field. Korean Circ J. 2019; 49:908–931. PMID: 31456367.
Article27. Cameli M, Pastore MC, Righini FM, et al. Prognostic value of left atrial strain in patients with moderate asymptomatic mitral regurgitation. Int J Cardiovasc Imaging. 2019; 35:1597–1604. PMID: 30972528.
Article28. Debonnaire P, Leong DP, Witkowski TG, et al. Left atrial function by two-dimensional speckle-tracking echocardiography in patients with severe organic mitral regurgitation: association with guidelines-based surgical indication and postoperative (long-term) survival. J Am Soc Echocardiogr. 2013; 26:1053–1062. PMID: 23860096.
Article