J Korean Med Sci.
2022 Feb;37(8):e61. 10.3346/jkms.2022.37.e61.
A Case Report of Varicella Zoster Meningitis as Co-Infection With Breakthrough COVID-19 in an Immunocompetent Patient
- Affiliations
-
- 1Department of Neurology, Dankook University Hospital, Cheonan, Korea
- KMID: 2526796
- DOI: http://doi.org/10.3346/jkms.2022.37.e61
Abstract
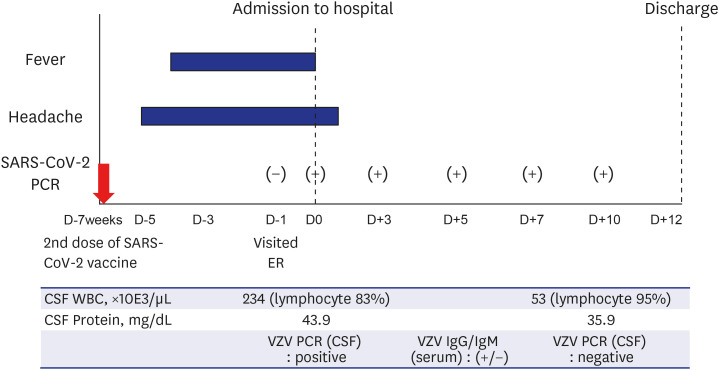
- There are several previous reports that infection or reactivation of varicella zoster virus (VZV) can occur after coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Herein, we report a rare case of VZV meningitis in breakthrough COVID-19. An 18-years-old male visited the emergency room, presenting with a headache and fever of up to 38.4°C for 5 days. He received the second dose of BNT162b2 mRNA SARS-CoV-2 vaccine 7 weeks prior to symptom onset. The symptoms persisted with headache, fever, and nausea. His cerebrospinal fluid (CSF) showed an elevated opening pressure of 27 cm H2O, 6/µL red blood cells, 234/µL white blood cells polymorphonuclear leukocytes 3%, lymphocytes 83%, and other 14%), 43.9 mg/dL protein, and 59 mg/dL glucose, and CSF polymerase chain reaction (PCR) test was positive for VZV. Also, he was diagnosed with COVID-19 by reverse transcriptase-PCR examining upper and lower respiratory tract. We administered intravenous acyclovir for 12 days, and he was discharged without any neurologic complication.
Keyword
Figure
Reference
-
1. Diez-Domingo J, Parikh R, Bhavsar AB, Cisneros E, McCormick N, Lecrenier N. Can COVID-19 increase the risk of herpes zoster? A narrative review. Dermatol Ther (Heidelb). 2021; 11(4):1119–1126. PMID: 33999370.
Article2. Maia CMF, Marques NP, de Lucena EHG, de Rezende LF, Martelli DRB, Martelli-Júnior H. Increased number of herpes zoster cases in Brazil related to the COVID-19 pandemic. Int J Infect Dis. 2021; 104:732–733. PMID: 33582367.
Article3. Patel P, Undavia A, Choudry R, Zhang Y, Prabhu AM. COVID-19 associated with concomitant varicella zoster viral encephalitis. Neurol Clin Pract. 2021; 11(2):e219–e221. PMID: 33842100.
Article4. Voisin O, Deluca N, Mahé A, Lelorc’h E, Hubert S, Ménage E, et al. Disseminated herpes zoster during COVID-19. Infect Dis Clin Pract (Baltim Md). 2021; 29(2):e109–e110. PMID: 34191904.
Article5. Katsikas Triantafyllidis K, Giannos P, Mian IT, Kyrtsonis G, Kechagias KS. Varicella zoster virus reactivation following COVID-19 vaccination: a systematic review of case reports. Vaccines (Basel). 2021; 9(9):1013. PMID: 34579250.
Article6. Furer V, Zisman D, Kibari A, Rimar D, Paran Y, Elkayam O.. Herpes zoster following BNT162b2 mRNA COVID-19 vaccination in patients with autoimmune inflammatory rheumatic diseases: a case series. Rheumatology (Oxford). 2021; 60(SI):SI90–SI95. PMID: 33848321.
Article7. Koh S, Kim HN, Kim YS, Kim TJ. Varicella zoster virus reactivation in central and peripheral nervous systems following COVID-19 vaccination in an immunocompetent patient. J Clin Neurol. 2022; 18(1):99–101. PMID: 35021285.
Article8. Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020; 20(6):355–362. PMID: 32376901.
Article9. Zheng HY, Zhang M, Yang CX, Zhang N, Wang XC, Yang XP, et al. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell Mol Immunol. 2020; 17(5):541–543. PMID: 32203186.
Article10. Nagel MA, Gilden D. Neurological complications of varicella zoster virus reactivation. Curr Opin Neurol. 2014; 27(3):356–360. PMID: 24792344.
Article11. Huh K, Jung J, Hong J, Kim M, Ahn JG, Kim JH, et al. Impact of nonpharmaceutical interventions on the incidence of respiratory infections during the coronavirus disease 2019 (COVID-19) outbreak in Korea: a nationwide surveillance study. Clin Infect Dis. 2021; 72(7):e184–e191. PMID: 33150393.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of varicella zoster meningitis in immunocompetent children
- A Case of Aseptic Meningitis with Herpes Zoster
- A case of acute aseptic meningitis associated with herpes zoster
- Varicella Zoster Viral Myelitis in Immunocompetent Patient
- Dysphagia with Unilateral Vocal Cord Paralysis in Herpes Zoster: A Case Report