Neurointervention.
2022 Mar;17(1):45-49. 10.5469/neuroint.2021.00472.
Y Stent Rendezvous to Treat Symptomatic Innominate Artery Stenosis
- Affiliations
-
- 1Department of Radiology, Austin Health, Melbourne, VIC, Australia
- KMID: 2526625
- DOI: http://doi.org/10.5469/neuroint.2021.00472
Abstract
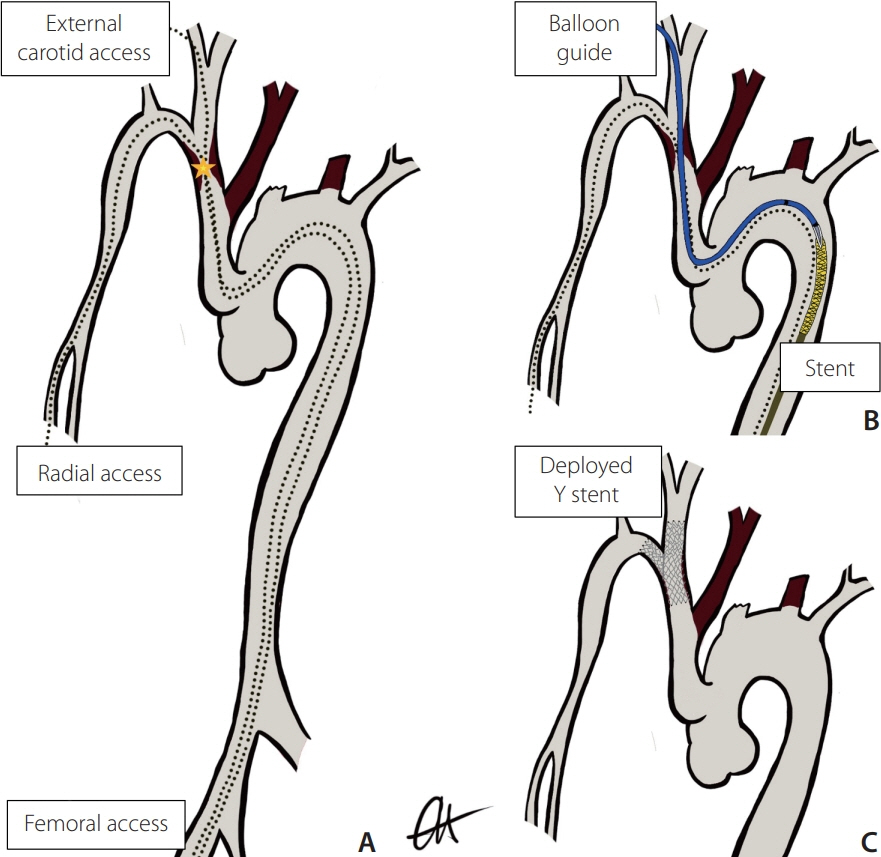
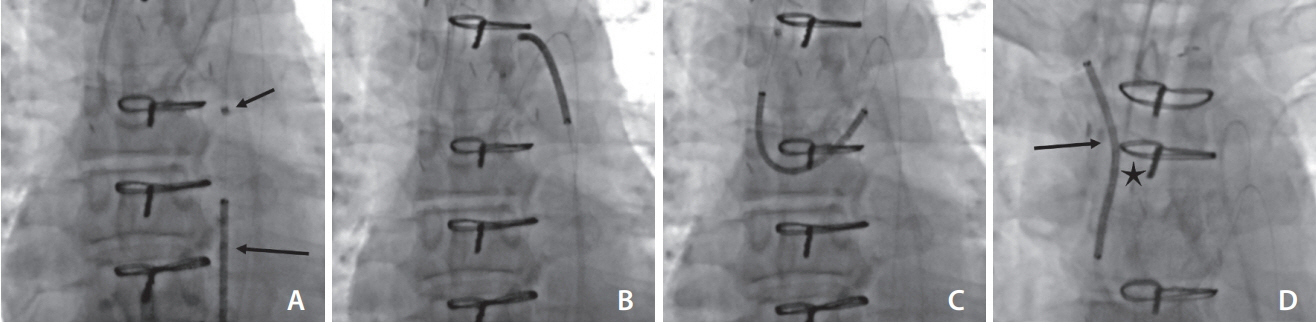
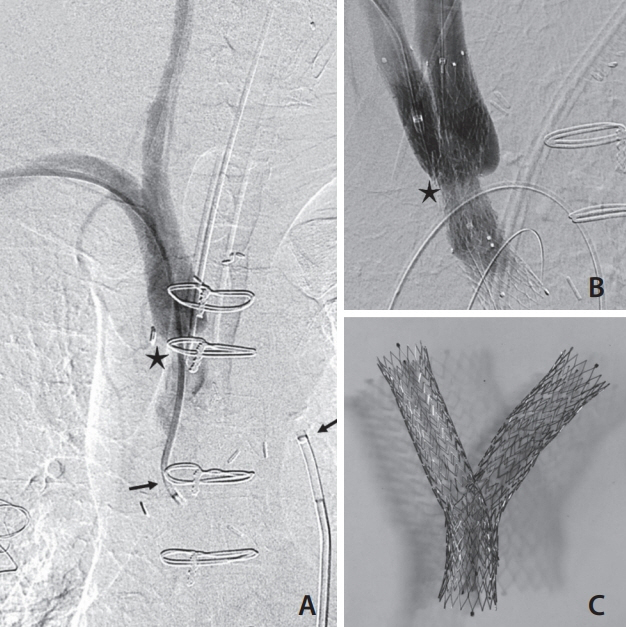
- A male in his 60s presented with transient ischemic attacks 5 years after aortic arch branch graft repair for type A aortic dissection. Computed tomographic angiography demonstrated 80% stenosis of the brachiocephalic artery close to the origins of the right common carotid and subclavian arteries. The case was reviewed at our multidisciplinary aortic meeting and a plan for endovascular management was made. Percutaneous endovascular Y stenting from the innominate artery into the left common carotid and subclavian arteries was achieved using self-expanding nitinol stents with a rendezvous technique that included retrograde right radial artery, retrograde right external carotid artery, and retrograde right femoral arterial approaches. At 6 months review, the stents remained widely patent and the patient was symptom-free.
Keyword
Figure
Reference
-
1. White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, et al. Ischemic stroke subtype incidence among Whites, Blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005; 111:1327–1331.
Article2. Veith FJ, Amor M, Ohki T, Beebe HG, Bell PR, Bolia A, et al. Current status of carotid bifurcation angioplasty and stenting based on a consensus of opinion leaders. J Vasc Surg. 2001; 33(2 Suppl):S111–S116.
Article3. van de Weijer MA, Vonken EJ, de Vries JP, Moll FL, Vos JA, de Borst GJ. Technical and clinical success and long-term durability of endovascular treatment for atherosclerotic aortic arch branch origin obstruction: evaluation of 144 procedures. Eur J Vasc Endovasc Surg. 2015; 50:13–20.
Article4. Clavel P, Hebert S, Saleme S, Mounayer C, Rouchaud A, Marin B. Cumulative incidence of restenosis in the endovascular treatment of extracranial carotid artery stenosis: a meta-analysis. J Neurointerv Surg. 2019; 11:916–923.
Article5. Bonati LH, Gregson J, Dobson J, McCabe DJH, Nederkoorn PJ, van der Worp HB, International Carotid Stenting Study investigators, et al. Restenosis and risk of stroke after stenting or endarterectomy for symptomatic carotid stenosis in the International Carotid Stenting Study (ICSS): secondary analysis of a randomised trial. Lancet Neurol. 2018; 17:587–596.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wingspan Stenting for Symptomatic Severe In-Stent Stenosis of a Closed-Cell Stent after Stent-Assisted Coiling of a Ruptured Intracranial Aneurysm
- An Experience of Carotid-Carotid Bypass In Innominate Artery Stenosis
- Retrieval of a dislodged and dismounted coronary stent; using a rendezvous and snare technique at the brachial artery level via femoral approach
- Successful Open Surgical Treatment of Tracheo-Innominate Artery Fistula after Endovascular Stent Graft Repair: A Case Report
- Surgical Treatment of an Innominate Artery Aneurysm Using Near-Infrared Spectroscopy for Cerebral Monitoring: A Case Report