Anesth Pain Med.
2022 Jan;17(1):12-23. 10.17085/apm.21113.
Recent update on epidural blood patch
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chung-Ang University College of Medicine, Seoul, KoreaDepartment of Anesthesiology and Pain medicine, College of Medicine, Chung-Ang University, Seoul, Korea
- KMID: 2526523
- DOI: http://doi.org/10.17085/apm.21113
Abstract
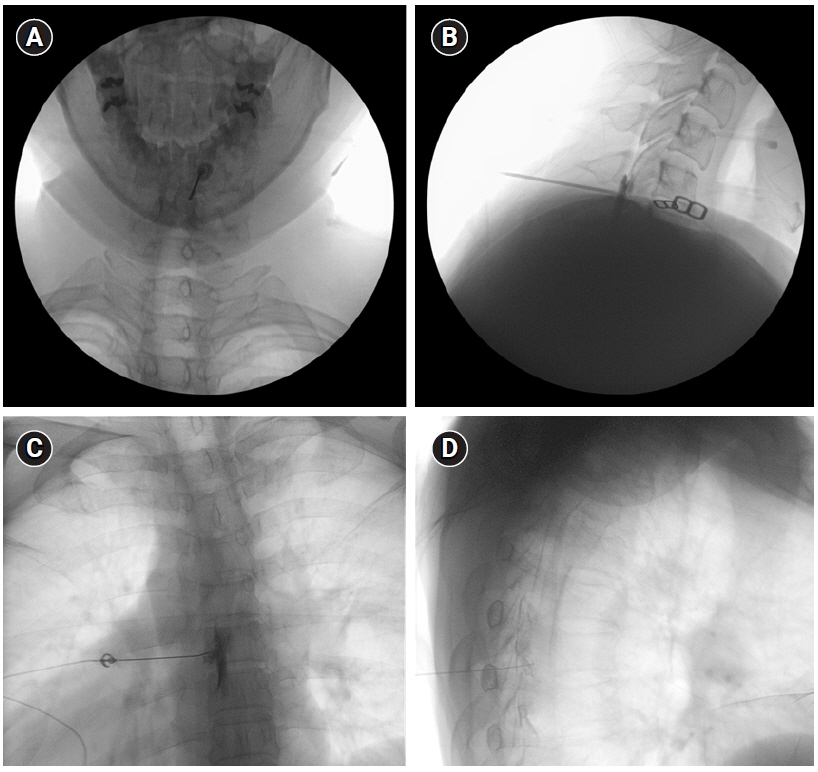
- Epidural blood patch (EBP) is the injection of autologous blood into the epidural space with the intent of sealing off a dural tear and stopping the leakage of cerebrospinal fluid (CSF). EBP may cause an increase in intracranial pressure (ICP) due to the mass effect of the injected blood volume, causing CSF from the spinal compartment to enter the intracranial compartment. EBP is usually considered in the management of moderate to severe headache (HA) attributed to low CSF pressure, such as post-dural puncture HA (PDPH), CSF fistula HA, and HA attributed to spontaneous intracranial hypotension (SIH) that does not respond to conservative management. However, prophylactic administration of EBP after accidental dural puncture can hardly be substantiated at present. EBP is generally safe but may rarely be associated with serious complications. Therefore, it should be carefully planned and performed under C-arm fluoroscopic guidance. Although many studies on PDPH and SIH have been conducted until recently, only few reviews have summarized the effectiveness of EBP from the perspective of a pain physician. This article reviews the current literature on the indication, contraindication, procedural consideration, post-procedural management, outcomes, and complications of EBP and the considerations for EBP in patients with COVID-19.
Keyword
Figure
Reference
-
1. Ljubisavljevic S. Postdural puncture headache as a complication of lumbar puncture: clinical manifestations, pathophysiology, and treatment. Neurol Sci. 2020; 41:3563–8.2. Fichtner J, Fung C, Z'Graggen W, Raabe A, Beck J. Lack of increase in intracranial pressure after epidural blood patch in spinal cerebrospinal fluid leak. Neurocrit Care. 2012; 16:444–9.3. Gormley JB. Treatment of postspinal headache. Anesthesiology. 1960; 21:565–6.4. Russell R, Laxton C, Lucas DN, Niewiarowski J, Scrutton M, Stocks G. Treatment of obstetric post-dural puncture headache. Part 2: epidural blood patch. Int J Obstet Anesth. 2019; 38:104–18.5. Buddeberg BS, Bandschapp O, Girard T. Post-dural puncture headache. Minerva Anestesiol. 2019; 85:543–53.6. Crawford JS. Experiences with epidural blood patch. Anaesthesia. 1980; 35:513–5.7. Kwak KH. Postdural puncture headache. Korean J Anesthesiol. 2017; 70:136–43.8. Patel R, Urits I, Orhurhu V, Orhurhu MS, Peck J, Ohuabunwa E, et al. A comprehensive update on the treatment and management of postdural puncture headache. Curr Pain Headache Rep. 2020; 24:24.9. Turnbull DK, Shepherd DB. Post-dural puncture headache: pathogenesis, prevention and treatment. Br J Anaesth. 2003; 91:718–29.10. Mokri B. Spontaneous intracranial hypotension. Continuum (Minneap Minn). 2015; 21:1086–108.11. Ferrante E, Trimboli M, Rubino F. Spontaneous intracranial hypotension: review and expert opinion. Acta Neurol Belg. 2020; 120:9–18.12. Grant R, Condon B, Hart I, Teasdale GM. Changes in intracranial CSF volume after lumbar puncture and their relationship to post-LP headache. J Neurol Neurosurg Psychiatry. 1991; 54:440–2.13. Bolden N, Gebre E. Accidental dural puncture management: 10-year experience at an academic tertiary care center. Reg Anesth Pain Med. 2016; 41:169–74.14. Tubben RE, Jain S, Murphy PB. Epidural blood patch. In: StatPearls. Edited by Abai B, Abu-Ghosh A, Acharya AB, Acharya U, Adhia SG, Aeby TC, et al.: Treasure Island (FL), StatPearls Publishing;2021.15. Katz D, Beilin Y. Review of the alternatives to epidural blood patch for treatment of postdural puncture headache in the parturient. Anesth Analg. 2017; 124:1219–28.16. Russell R, Laxton C, Lucas DN, Niewiarowski J, Scrutton M, Stocks G. Treatment of obstetric post-dural puncture headache. Part 1: conservative and pharmacological management. Int J Obstet Anesth. 2019; 38:93–103.17. Scemama P, Farah F, Mann G, Margulis R, Gritsenko K, Shaparin N. Considerations for epidural blood patch and other postdural puncture headache treatments in patients with COVID-19. Pain Physician. 2020; 23:S305–10.18. Gaiser RR. Postdural puncture headache: an evidence-based approach. Anesthesiol Clin. 2017; 35:157–67.19. Arevalo-Rodriguez I, Muñoz L, Godoy-Casasbuenas N, Ciapponi A, Arevalo JJ, Boogaard S, et al. Needle gauge and tip designs for preventing post-dural puncture headache (PDPH). Cochrane Database Syst Rev. 2017; 4:CD010807.20. Kumar V, Maves T, Barcellos W. Epidural blood patch for treatment of subarachnoid fistula in children. Anaesthesia. 1991; 46:117–8.21. Chauhan C, Francis GA, Kemeny AA. The avoidance of surgery in the treatment of subarachnoid cutaneous fistula by the use of an epidural blood patch: technical case report. Neurosurgery. 1995; 36:612–3; discussion 613-4.22. Katz J. Treatment of a subarachnoid-cutaneous fistula with an epidural blood patch. Anesthesiology. 1984; 60:603–4.23. Signorelli F, Caccavella VM, Giordano M, Ioannoni E, Caricato A, Polli FM, et al. A systematic review and meta-analysis of factors affecting the outcome of the epidural blood patching in spontaneous intracranial hypotension. Neurosurg Rev. 2021; 44:3079–85.24. Kranz PG, Gray L, Malinzak MD, Amrhein TJ. Spontaneous intracranial hypotension: pathogenesis, diagnosis, and treatment. Neuroimaging Clin N Am. 2019; 29:581–94.25. Amrhein TJ, Kranz PG. Spontaneous intracranial hypotension: imaging in diagnosis and treatment. Radiol Clin North Am. 2019; 57:439–451.26. D'Antona L, Jaime Merchan MA, Vassiliou A, Watkins LD, Davagnanam I, Toma AK, et al. Clinical presentation, investigation findings, and treatment outcomes of spontaneous intracranial hypotension syndrome: a systematic review and meta-analysis. JAMA Neurol. 2021; 78:329–37.27. Kranz PG, Malinzak MD, Amrhein TJ, Gray L. Update on the diagnosis and treatment of spontaneous intracranial hypotension. Curr Pain Headache Rep. 2017; 21:37.28. Upadhyaya P, Ailani J. A review of spontaneous intracranial hypotension. Curr Neurol Neurosci Rep. 2019; 19:22.29. Davidson B, Nassiri F, Mansouri A, Badhiwala JH, Witiw CD, Shamji MF, et al. Spontaneous intracranial hypotension: a review and introduction of an algorithm for management. World Neurosurg. 2017; 101:343–9.30. Rettenmaier LA, Park BJ, Holland MT, Hamade YJ, Garg S, Rastogi R, et al. Value of targeted epidural blood patch and management of subdural hematoma in spontaneous intracranial hypotension: case report and review of the literature. World Neurosurg. 2017; 97:27–38.31. So Y, Park JM, Lee PM, Kim CL, Lee C, Kim JH. Epidural blood patch for the treatment of spontaneous and iatrogenic orthostatic headache. Pain Physician. 2016; 19:E1115–22.32. McInerney HJ, Lee M, Saunders T, Schabel J, Adsumelli RSN. Symptomatic intrathecal hematoma following an epidural blood patch for an obstetric patient with postdural puncture headache: a case report and synthesis of the literature. Case Rep Anesthesiol. 2020; 2020:8925731.33. Seemiller J, Challagundla S, Taylor T, Zand R. Intrathecal blood injection: a case report of a rare complication of an epidural blood patch. BMC Neurol. 2020; 20:187.34. Lee YG, Sa M, Oh I, Lim JA, Woo NS, Kim J. Multiple epidural fibrin glue patches in a patient with spontaneous intracranial hypotension - a case report -. Anesth Pain Med. 2019; 14:335–40.35. Turner M. Epidural blood patch with allogeneic blood for post-dural puncture headache. Int J Obstet Anesth. 2006; 15:261; author reply 261-2.36. McKenzie A, Manson L. Allogeneic blood for epidural blood patch–not without risk. Int J Obstet Anesth. 2006; 15:260; author reply 61-2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case Report of Epidnral Blood Patch for Post-Lumbar Puneture Headache
- Effect of Epidural Autologous Blood Patch on the Prevention of Post-dural Puncture Headche after Spinal Anesthesia
- Pseudomeningocele after lumbar discectomy treated with fibrin glue and epidural blood patch: A case report
- Multiple Metastatic Brain Tumor: Complicated with Post-dural Puncture Headache : A case report
- Epidural Blood Patch to Treat Spontaneous Intracranial Hypotension