Healthc Inform Res.
2022 Jan;28(1):35-45. 10.4258/hir.2022.28.1.35.
Analysis of the Effects of Electronic Medical Records and a Payment Scheme on the Length of Hospital Stay
- Affiliations
-
- 1Information Healthcare Science Course, Graduate School of Integrated Arts and Sciences, Kochi University, Kochi, Japan
- 2Healthcare Informatics Division, Basic Nursing Department, Medical School, Kochi University, Kochi, Japan
- KMID: 2526492
- DOI: http://doi.org/10.4258/hir.2022.28.1.35
Abstract
Objectives
This study analyzed the effects of computerization of medical information systems and a hospital payment scheme on medical care outcomes. Specifically, we examined the effects of Electronic Medical Records (EMRs) and a diagnosis procedure combination/per-diem payment scheme (DPC/PDPS) on the average length of hospital stay (ALOS).
Methods
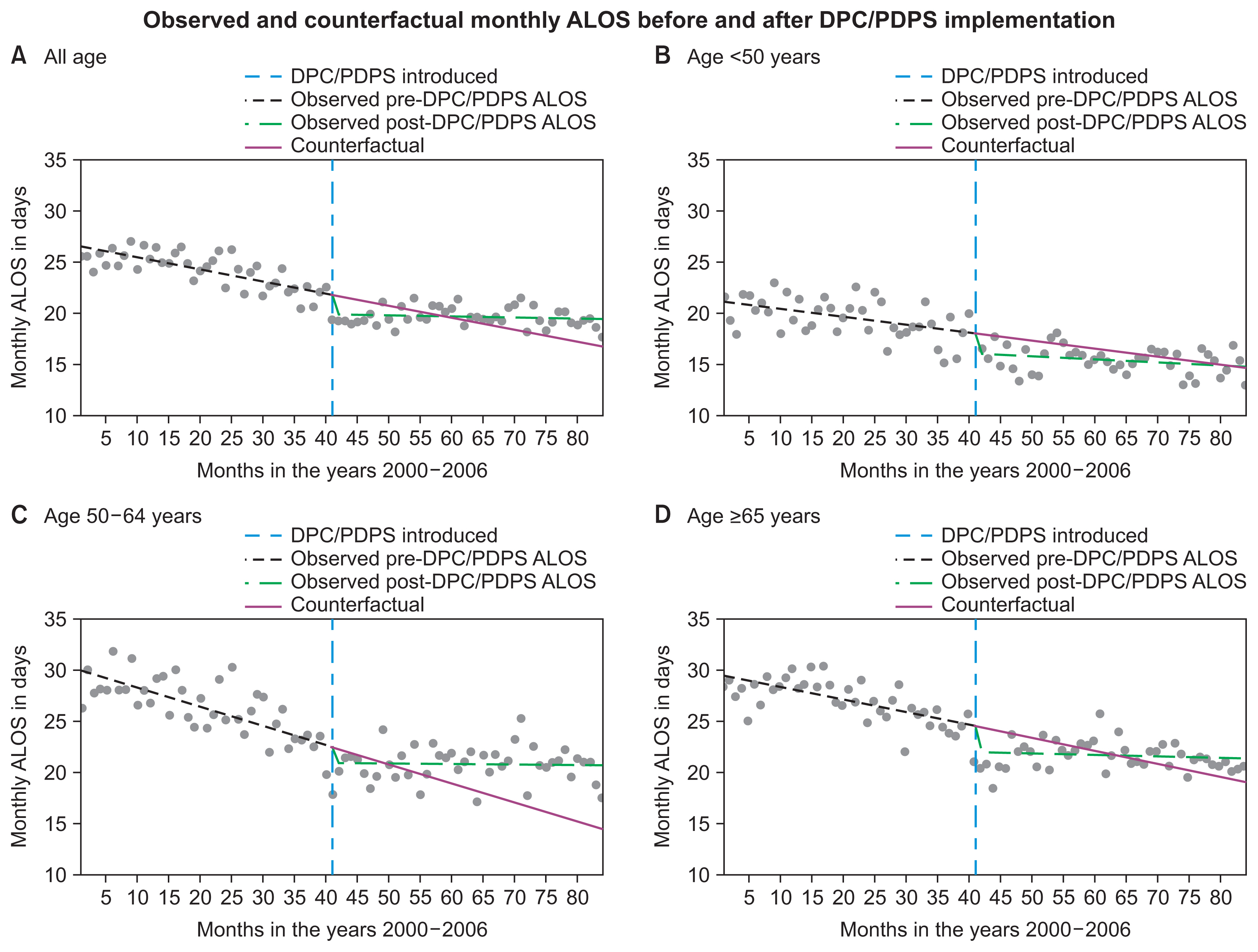
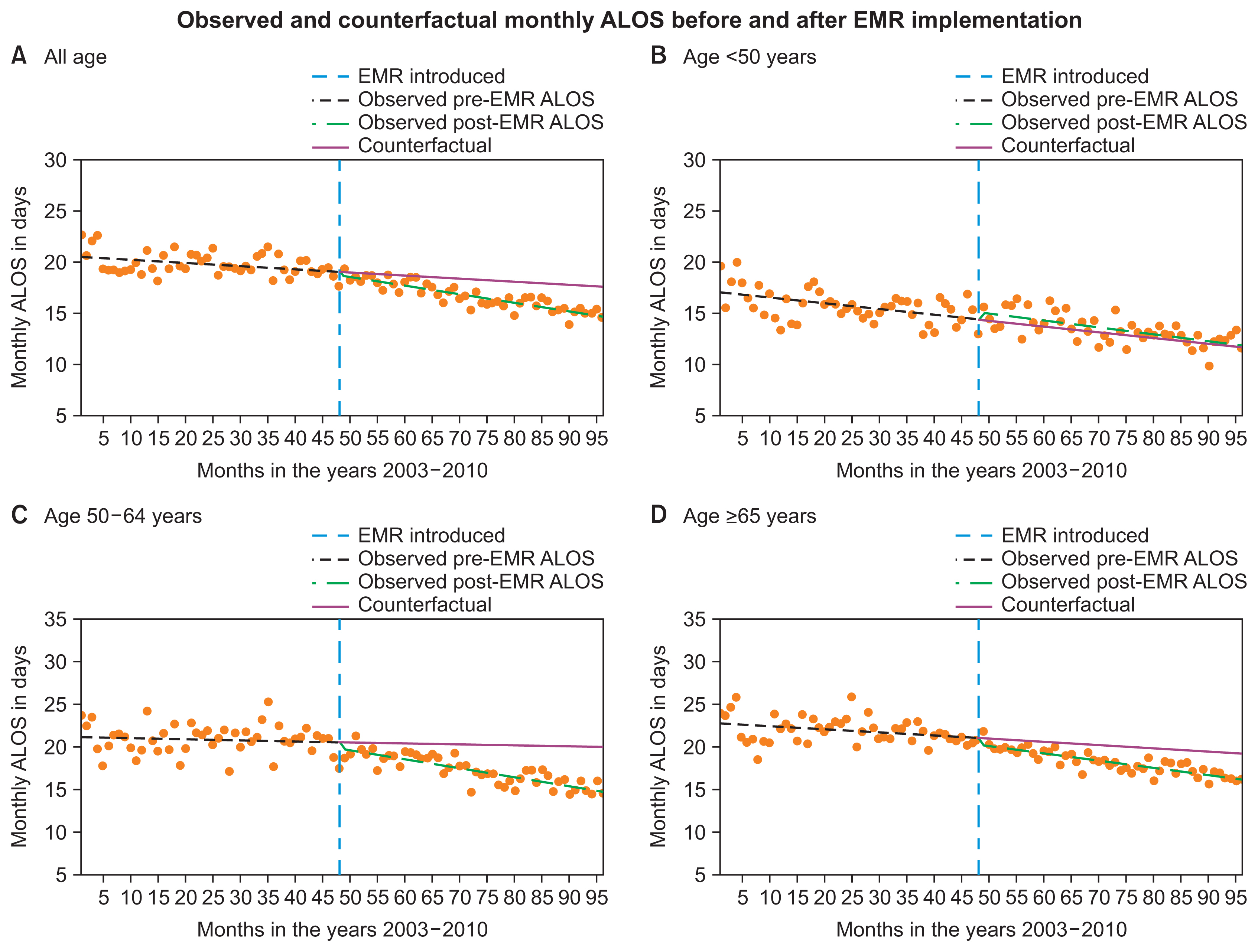
Post-intervention changes in the monthly ALOS were measured using an interrupted time-series analysis.
Results
The level changes observed in the monthly ALOS immediately post-DPC/PDPS were –1.942 (95% confidence interval [CI], –2.856 to –1.028), –1.885 (95% CI, –3.176 to –0.593), –1.581 (95% CI, –3.081 to –0.082) and –2.461 (95% CI, –3.817 to 1.105) days in all ages, <50, 50–64, and ≥65 years, respectively. During the post-DPC/PDPS period, trends of 0.107 (95% CI, 0.069 to 0.144), 0.048 (95% CI, –0.006 to 0.101), 0.183 (95% CI, 0.122 to 0.245) and 0.110 (95% CI, 0.054 to 0.167) days/month, respectively, were observed. During the post-EMR period, trends of –0.053 (95% CI, –0.080 to –0.027), –0.093 (95% CI, –0.135 to –0.052), and –0.049 (95% CI, –0.087 to –0.012) days/month were seen for all ages, 50–64 and ≥65 years, respectively.
Conclusions
The increasing post-DPC/PDPS trends offset the decline in ALOS observed immediately post-DPC/PDPS, and the observed ALOS was longer than the counterfactual at the end of the DPC/PDPS study periods. Conversely, due to the downward trend seen after EMR introduction, the actual ALOS at the end of the EMR study period was shorter than the counterfactual, suggesting that EMRs might be more effective than the DPC/PDPS in sustainably reducing the LOS.
Keyword
Figure
Reference
-
References
1. Mihailovic N, Kocic S, Jakovljevic M. Review of diagnosis-related group-based financing of hospital care. Health Serv Res Manag Epidemiol. 2016; 3:2333392816647892.
Article2. Organization for Economic Co-operation and Development. Health at a glance 2019 OECD indicators. Paris, France: Organization for Economic Co-operation and Development;2019.3. Ishii M. DRG/PPS and DPC/PDPS as prospective payment systems. Japan Med Assoc J. 2012; 55(4):279–91.4. Annear PL, Kwon S, Lorenzoni L, Duckett S, Huntington D, Langenbrunner JC, et al. Pathways to DRG-based hospital payment systems in Japan, Korea, and Thailand. Health Policy. 2018; 122(7):707–13.
Article5. Jang SI, Nam CM, Lee SG, Kim TH, Park S, Park EC. Impact of payment system change from per-case to perdiem on high severity patient’s length of stay. Medicine (Baltimore). 2016; 95(37):e4839.
Article6. O’Reilly J, Busse R, Hakkinen U, Or Z, Street A, Wiley M. Paying for hospital care: the experience with implementing activity-based funding in five European countries. Health Econ Policy Law. 2012; 7(1):73–101.7. Meng Z, Hui W, Cai Y, Liu J, Wu H. The effects of DRGs-based payment compared with cost-based payment on inpatient healthcare utilization: a systematic review and meta-analysis. Health Policy. 2020; 124(4):359–67.
Article8. Jung YW, Pak H, Lee I, Kim EH. The effect of diagnosis-related group payment system on quality of care in the field of obstetrics and gynecology among Korean tertiary hospitals. Yonsei Med J. 2018; 59(4):539–45.
Article9. Choi JW, Kim SJ, Park HK, Jang SI, Kim TH, Park EC. Effects of a mandatory DRG payment system in South Korea: analysis of multi-year nationwide hospital claims data. BMC Health Serv Res. 2019; 19(1):776.
Article10. Hamada H, Sekimoto M, Imanaka Y. Effects of the per diem prospective payment system with DRG-like grouping system (DPC/PDPS) on resource usage and healthcare quality in Japan. Health Policy. 2012; 107(2–3):194–201.
Article11. Kondo A, Kawabuchi K. Evaluation of the introduction of a diagnosis procedure combination system for patient outcome and hospitalisation charges for patients with hip fracture or lung cancer in Japan. Health Policy. 2012; 107(2–3):184–93.
Article12. Jian W, Lu M, Chan KY, Poon AN, Han W, Hu M, et al. Payment reform pilot in Beijing hospitals reduced expenditures and out-of-pocket payments per admission. Health Aff (Millwood). 2015; 34(10):1745–52.
Article13. Hu WY, Yeh CF, Shiao AS, Tu TY. Effects of diagnosis-related group payment on health-care provider behaviors: a consecutive three-period study. J Chin Med Assoc. 2015; 78(11):678–85.
Article14. Kaneko K, Onozuka D, Shibuta H, Hagihara A. Impact of electronic medical records (EMRs) on hospital productivity in Japan. Int J Med Inform. 2018; 118:36–43.
Article15. Centers for Medicaid and Medicare Services. Electronic Health Records [Internet]. Baltimore (MD): Centers for Medicaid and Medicare Services;2012. [cited at 2021 Oct 18]. Available from: https://www.cms.gov/Medicare/E-Health/EHealthRecords .16. Japan Association of Medical Informatics. JAMI viewpoint concerning the definition of the electronic medical record [Internet]. Tokyo, Japan: Japan Association of Medical Informatics;2003. [cited at 2021 Oct 18]. Available from: http://jami.jp/english/about/doc/denshika-rute_en.pdf .17. Thompson G, O’Horo JC, Pickering BW, Herasevich V. Impact of the electronic medical record on mortality, length of stay, and cost in the hospital and ICU: a systematic review and metaanalysis. Crit Care Med. 2015; 43(6):1276–82.18. Agha L. The effects of health information technology on the costs and quality of medical care. J Health Econ. 2014; 34:19–30.
Article19. Barnett ML, Mehrotra A, Jena AB. Adverse inpatient outcomes during the transition to a new electronic health record system: observational study. BMJ. 2016; 354:i3835.
Article20. Yanamadala S, Morrison D, Curtin C, McDonald K, Hernandez-Boussard T. Electronic health records and quality of care: an observational study modeling impact on mortality, readmissions, and complications. Medicine (Baltimore). 2016; 95(19):e3332.21. Wani D, Malhotra M. Does the meaningful use of electronic health records improve patient outcomes? J Oper Manag. 2018; 60:1–18.
Article22. Yang P, Cao Y, Liu D, Bai Y, Pan F, Xu Y. The effect of electronic medical record application on the length of stay in a Chinese general hospital: a department- and disease-focused interrupted time-series study. J Med Syst. 2014; 38(5):53.
Article23. Xue Y, Liang H, Wu X, Gong H, Li B, Zhang Y. Effects of electronic medical record in a Chinese hospital: a time series study. Int J Med Inform. 2012; 81(10):683–9.
Article24. Freedman S, Lin H, Prince J. Information technology and patient health: analyzing outcomes, populations, and mechanisms. Am J Health Econ. 2018; 4(1):51–79.
Article25. Inokuchi R, Sato H, Nakamura K, Aoki Y, Shinohara K, Gunshin M, et al. Motivations and barriers to implementing electronic health records and ED information systems in Japan. Am J Emerg Med. 2014; 32(7):725–30.
Article26. Kanakubo T, Kharrazi H. Comparing the trends of electronic health record adoption among hospitals of the United States and Japan. J Med Syst. 2019; 43(7):224.
Article27. Kawaguchi H, Koike S, Ohe K. Regional differences in electronic medical record adoption in Japan: a nationwide longitudinal ecological study. Int J Med Inform. 2018; 115:114–9.
Article28. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017; 46(1):348–55.29. Hategeka C, Ruton H, Karamouzian M, Lynd LD, Law MR. Use of interrupted time series methods in the evaluation of health system quality improvement interventions: a methodological systematic review. BMJ Glob Health. 2020; 5(10):e003567.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of DRG Payment on the Length of Stay and the Number of Outpatient Visits After Discharge for Caesarean Section During 2004-2007
- Factors Affecting the Postoperative Pain and Length of Hospital Stay of Liver Transplantation Donors
- Determinants of Length of Hospital Stay by Insured and Non-insured Patients
- The Effect of Emergency Department Expansion on the Emergency Department Length of Stay in a Tertiary Hospital
- A Review of Healthcare Provider Payment System in Korea